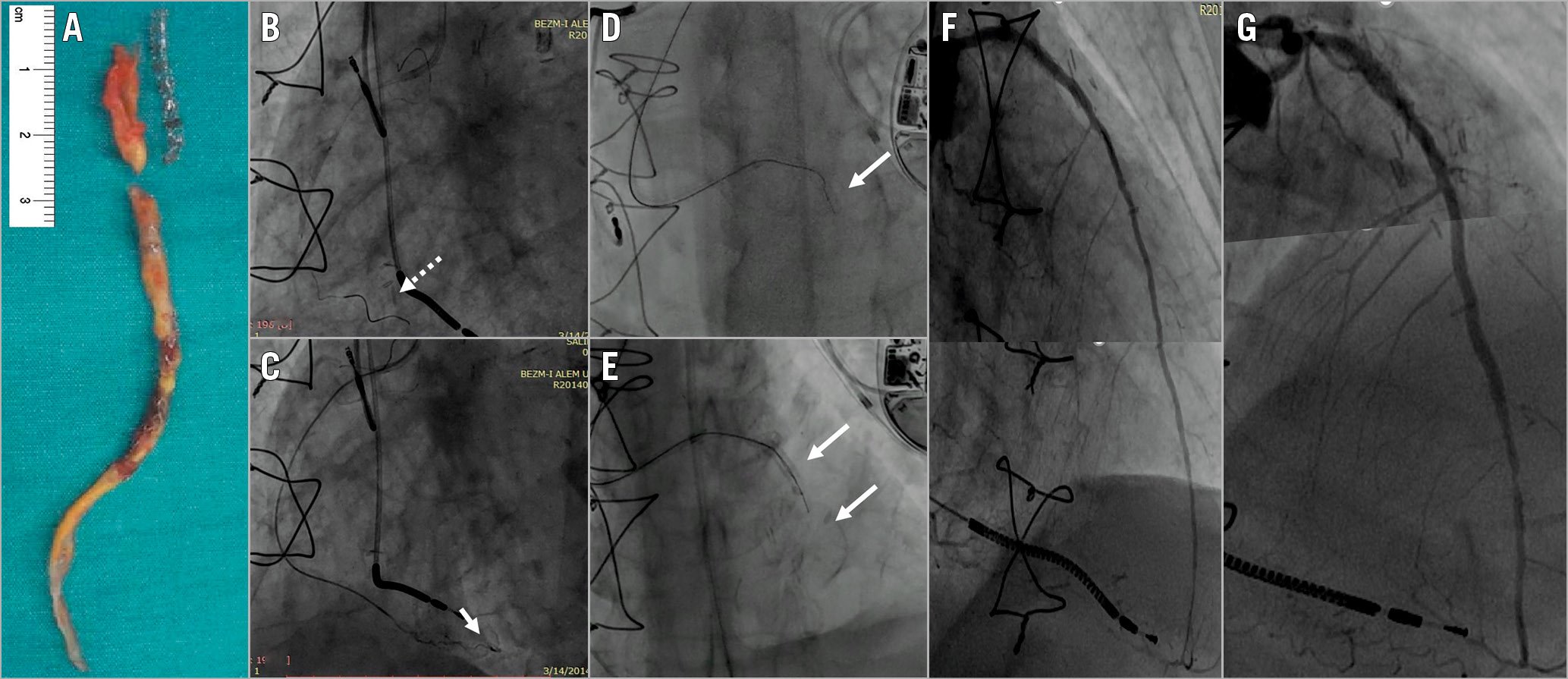
Figure 1. Percutaneous revascularisation of a chronic total occlusion in a surgically reconstructed vessel. Endarterectomy material and stents extracted during bypass surgery (A). Although a guidewire was advanced to the distal segment of the artery (dashed arrow indicates distal RCA, B), and a tip injection confirmed the true lumen (arrow, C), a guidewire could not be advanced through the collaterals. The operator switched to the antegrade approach (D & E) and the lesion was crossed using the parallel wire technique. Two bioresorbable vascular scaffolds were implanted (F). The control angiogram showed good results (G).
Treatment options for recurrent in-stent restenosis in patients with long and multiple stents include coronary artery bypass grafting (CABG) with endarterectomy and/or stent removal. A 63-year-old man was referred for percutaneous coronary intervention (PCI). Five years prior to his presentation, after five repeated PCIs between 2002 and 2011 with a total of 10 stents to the left anterior descending artery (LAD) due to recurrent restenosis, he had undergone CABG. The operation included an open endarterectomy on the LAD and extraction of previously implanted stents to enable anastomosis. The arteriotomy site was then closed with a saphenous vein patch, and the left internal mammary artery (LIMA) was subsequently anastomosed onto it. The procedure was reported at the time (Figure 1A). Three months before his presentation, after surviving a cardiac arrest, a coronary angiogram showed that the LIMA and LAD were occluded. Positron emission tomography (PET)/computed tomography (CT) scan confirmed viability in the LAD territory.
The operator started with the retrograde approach through the well-developed collaterals from the diminutive right coronary artery. Despite a microcatheter being advanced to the distal segment of the artery and a tip injection which confirmed the true lumen, a guidewire could not be advanced through the collaterals. At that point, the operator switched to the antegrade approach. The lesion was crossed using the parallel wire technique and two overlapping Absorb™ bioresorbable vascular scaffolds (Abbott Vascular, Santa Clara, CA, USA) were implanted (Figure 1B-Figure 1F). The control angiogram at six-month follow-up showed good results (Figure 1G) and he was asymptomatic at two years.
This case of a chronic total occlusion procedure in a surgically reconstructed vessel highlights that revascularisation options may still not be exhausted and can be achieved percutaneously in experienced centres. However, this experience is limited to one case and requires further research.
Conflict of interest statement
O. Goktekin is a proctor for Terumo, Abbott, Asahi, Boston Scientific, and Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.