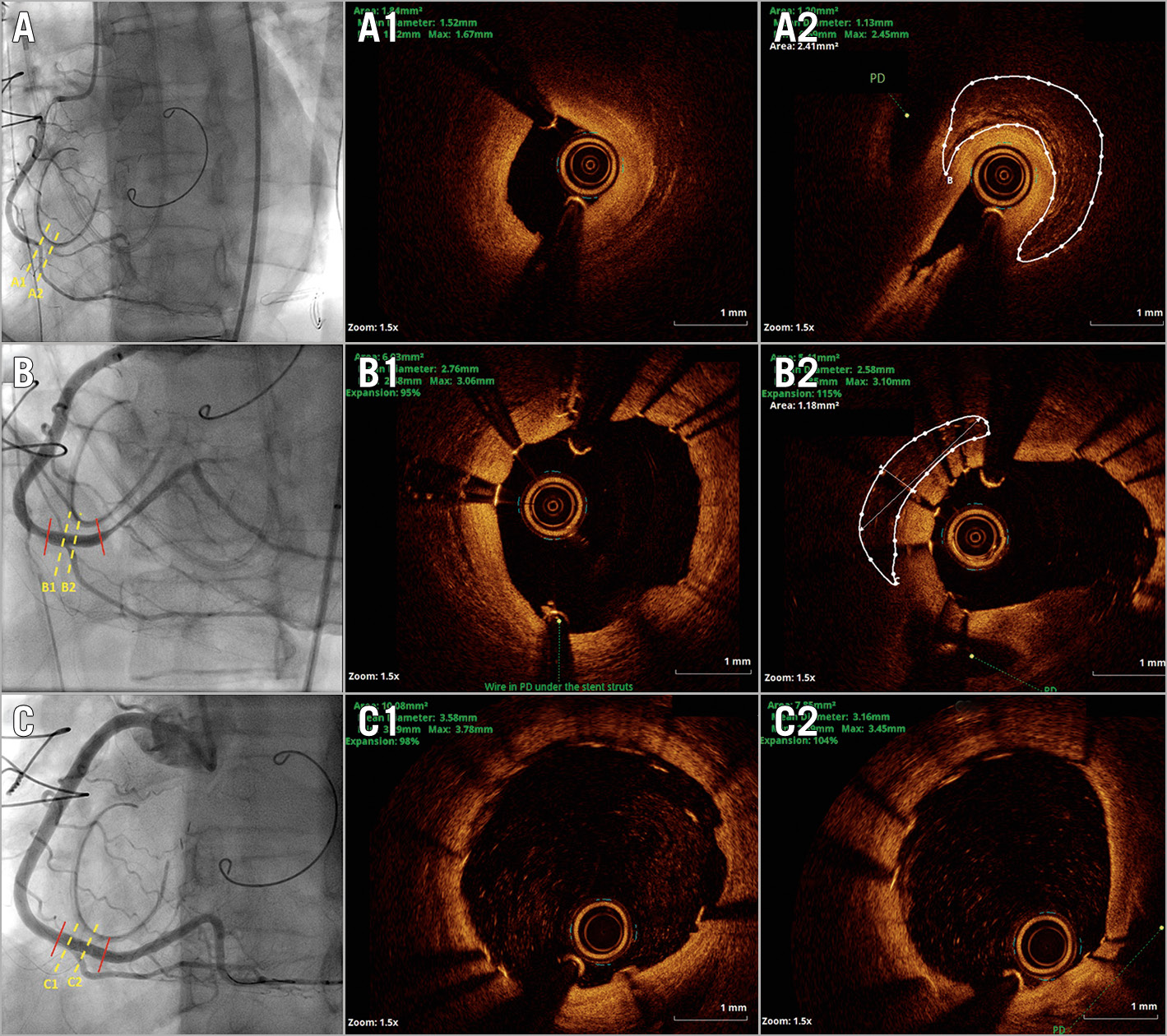
Figure 1. Angiographic and optical coherence tomography (OCT) images of the lesion. A) A subocclusive stenosis of the posterolateral branch just under the implanted tricuspid annuloplasty ring. A1) OCT image at the beginning of the stenosis, just before the posterior descending artery (PD). A2) OCT image of the most stenotic part with visible artery narrowing caused by entrapment, without intimal injury. The area encircled by the white line represents tissue beyond the adventitia layer. B) Angiographic and OCT results after stent implantation demonstrating appropriate stent expansion before and after the PD (B1, B2). In OCT image B2, a lesser extent of the tissue beyond the adventitia is visible (encircled area with white line). C) Positive remodelling of the artery on follow-up angiography, with OCT confirmation of optimal stent expansion after additional dilatation (C1, C2). The dotted yellow line represents the place of the corresponding cross-sectional OCT image presented. To ensure the same position of all images, measurements using OCT were performed with the PD as a referent point. Red lines represent stent edges.
Iatrogenic coronary artery stenosis following surgical valve repair is a rare but potentially lethal complication. However, it can be successfully treated using percutaneous coronary intervention (PCI).
A 49-year-old female patient was referred for urgent coronary angiography due to cardiogenic shock developed within three hours after surgical mitral and tricuspid valve repair. Bedside echo-cardio-graphy revealed severe right ventricular failure and moderately reduced left ventricular function, with normal valve function. The patient’s coronary angiography before surgery was unremarkable.
Urgent coronary angiography showed a subocclusive stenosis of the posterolateral (PL) branch with Thrombolysis In Myocardial Infarction (TIMI) 1 flow (Figure 1A, Moving image 1A). The stenosis began just before the bifurcation with the most significant stenosis after the posterior descending (PD) artery, under the implanted tricuspid annuloplasty ring. A workhorse wire (HI-TORQUE BALANCE MIDDLEWEIGHT UNIVERSAL; Abbott Vascular, Santa Clara, USA) was placed in the PD, but the PL branch was wired only after using a Corsair microcatheter and Fielder™ XT-R wire (both Asahi Intecc, Aichi, Japan). After a predilatation with a semi-compliant balloon (2.0×15 mm at 12 atmospheres), optical coherence tomo-graphy (OCT) was performed. It revealed abrupt stenosis, which began just before the PD, without signs of plaque rupture or intimal tear (Figure A1, Figure A2, Moving image 1A1). However, in the most stenotic part (1 mm after the PD), the tissue beyond the adventitia could be seen as if the artery was entrapped. Based on observation, it was hypothesised that the most likely causes were kinking or compression with a surgical stitch1. A 2.75/18 mm open-cell drug-eluting stent was implanted from the right coronary artery to the PL at 14 atmospheres. Additionally, after rewiring of the PD artery, stent struts were opened using kissing balloon and proximal optimisation techniques using a non-compliant balloon 3.0×8 mm at 16 atmospheres. Final angiographic and OCT results revealed appropriate stent expansion with moderate persistent stenosis proximal and distal to the stent, without signs of dissection, and with a smaller amount of the tissue beyond the adventitia visible (Figure 1B1, Figure 1B2, Moving image 1B, Moving image 1B1). However, patient haemodynamics partially improved and a decision was made to repeat the angiography following stabilisation. Over the next two days, the patient was weaned off inotropic and vasopressor support. A control angiography revealed patent coronary arteries. However, due to the underexpansion of the stent diagnosed by OCT, post-dilatation of the stent was performed. The final angiographic result was optimal (Figure 1C, Moving image 1C), as was the one from OCT (Figure 1C1, Figure 1C2), with non-significant edge dissection, most likely caused by stent post-dilatation (Moving image 1C1).
OCT enables precise evaluation of coronary artery patho-logy and is the most helpful tool in the guidance of challenging interventions with an unclear diagnosis2. As presented, the utilisation of OCT provided information regarding the cause of the stenosis by endorsing the clinical suspicion of an iatrogenic injury probably caused by artery kinking or surgical suture entrapment. However, the fact that the lesion was successfully treated with a stent favours kinking as the mechanism of the stenosis1. Finally, OCT provided reassurance in leaving a suboptimal angio-graphic result after the initial intervention, therefore preventing overtreatment.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1A. Initial coronary angiography demonstrating subocclusive stenosis of the posterolateral branch with TIMI 1 flow.
Moving image 1A1. Initial optical coherence tomography demonstrating tight, irregular stenosis without visible intimal injury. Part of the tissue beyond the adventitia can be appreciated after the stenosis.
Moving image 1B. Coronary angiography following stent implantation and stent optimisation. Dynamic stenosis on both sides of the stent can be appreciated.
Moving image 1B1. Optical coherence tomography after stent implantation demonstrating appropriate stent deployment.
Moving image 1C. Control coronary angiography demonstrating optimal final results in all branches.
Moving image 1C1. Control optical coherence tomography demonstrating optimal stent deployment.