A 56-year-old male was admitted with NSTEMI and underwent percutaneous coronary intervention with bare metal (cobalt-chromium) stent implantation (3.0×24 mm, 16 atm, post-dilated with 3.0×20 mm non-compliant balloon, 20 atm) in the mid segment of an anomalous circumflex artery (retroaortic course from the right sinus of Valsalva). The patient remained asymptomatic for five years post-procedure, when he presented with mild atypical chest pain. Myocardial stress perfusion scintigraphy detected no transient ischaemia; however, due to his persisting symptoms, a coronary computed tomography angiography was performed. This revealed restenosis and chronic recoil in the implanted stent (Online Figure 1). On follow-up angiography prominent hinge motion at the restenotic part of the stent was also demonstrated (Moving image 1). Optical coherence tomography (OCT) examination was performed (Moving image 2). This identified the segment with chronic recoil apart from neointimal hyperplasia (Figure 1). Within this segment we detected different abnormalities of the structure of struts, which points to possible mechanical limitations of current metallic rigid stent designs. In order to alleviate his symptoms, repeat PCI with a drug-eluting balloon was performed with angiographic success.
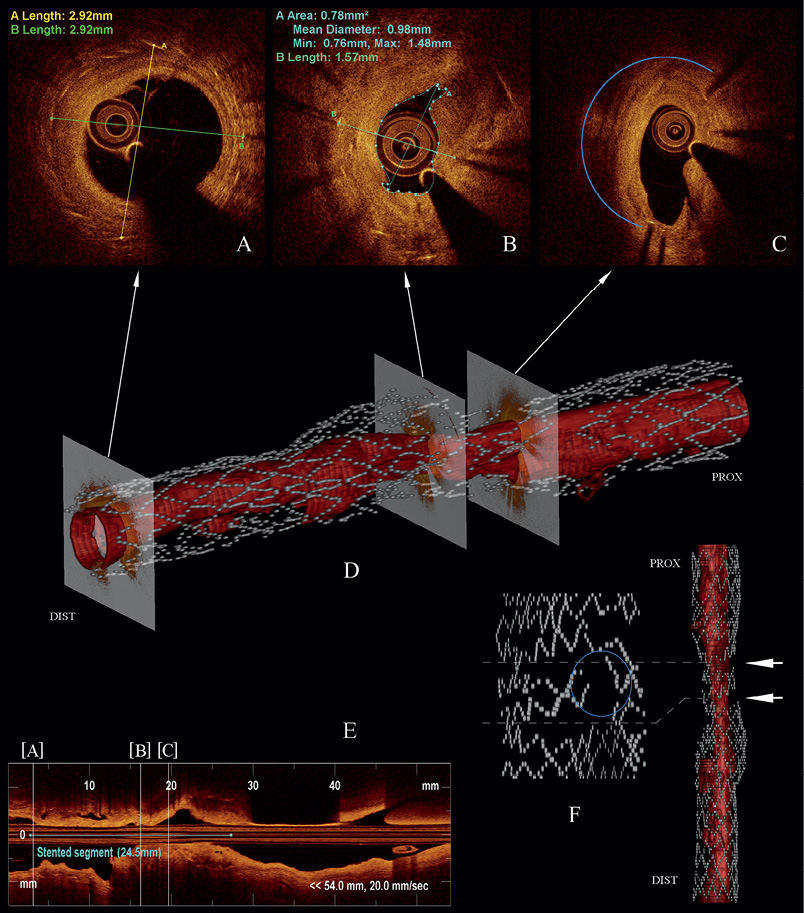
Figure 1. Optical coherence tomography at follow-up. OCT (C7-XR Fourier domain; St. Jude Medical, St. Paul, MN, USA) of the stented anomalous circumflex was performed (20 mm/s, 100 frames/s; longitudinal view of the pullback (E) after a predilatation with a 2.0×15 mm balloon (8 atm). At distal edge (A) the stent structure seems to be intact. The cross-section at minimal lumen area (B) shows marked concentric neointimal hyperplasia and is suggestive of chronic recoil. At the cross-section 3.6 mm more proximal (C) uneven circumferential distribution of struts can be seen. 3-D reconstruction of the pullback with delineation of struts and lumen border (D). Maximum intensity projection of polar transformation (F) (methodology based on Wang et al1) shows stent pseudo-fracture (strut separation related to open-cell stent design; similar to that found by Bartorelli et al2) at cross-sections marked with arrows; the upper location corresponds with uneven strut distribution shown on (C). However, real disruption of strut integrity was also visualised (blue circle) confirming stent fracture.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Follow-up angiography of the anomalous LCx (AP view).
Moving image 2. OCT pullback.
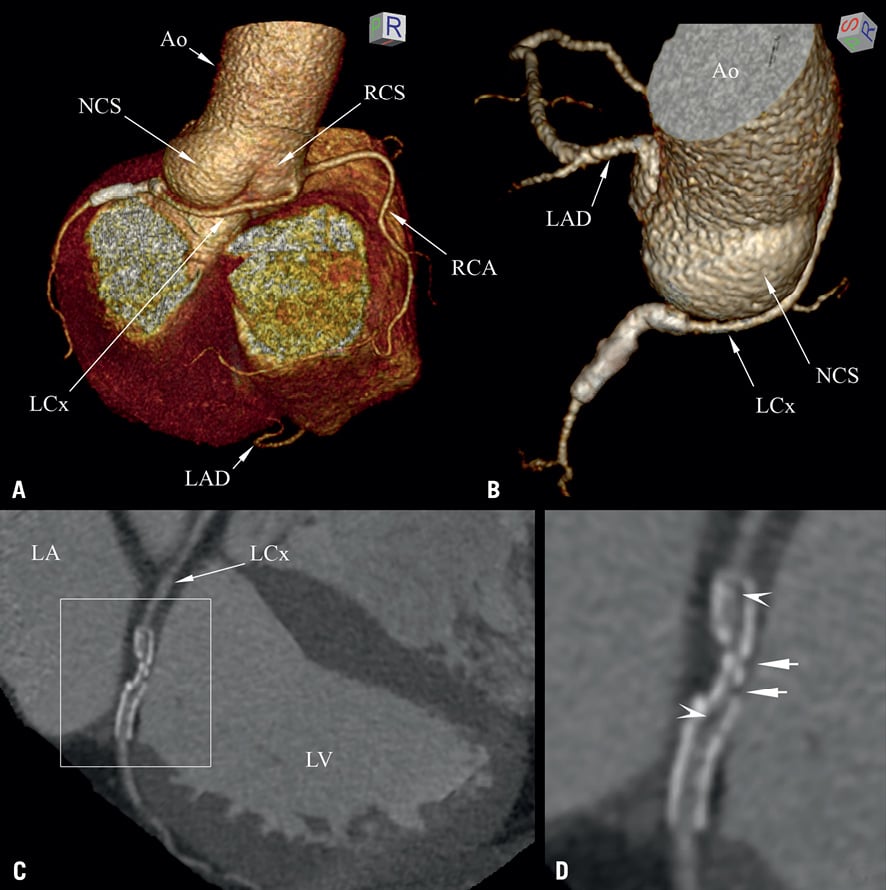
Online Figure 1. Coronary computed tomography angiography at follow-up. 3-D reconstructed view of epicardial arteries. A) Volume-rendered 3-D image clearly shows the anomalous origin of the LCx artery from the right coronary sinus (RCS) near the ostium of the right coronary artery (RCA). The LCx takes a retroaortic course (NCS: non-coronary sinus); its mid-proximal part was stented at index procedure. B) The stent appears bent. C) The stented segment shows apparent restenosis on curved multiplanar reconstruction of LCx. D) The enlarged image is suggestive of chronic recoil of the restenotic part of the stent, black spots inside the stent (arrowheads) suggestive of neointimal hyperplasia, whereas gaps are also detected (arrows).

