Stent implantation for pulmonary artery (PA) stenosis was first reported in 1988 by Mullins et al and over time has become the treatment of choice for the majority of these lesions1. Stents work because they provide the only effective solution to the Achilles’ heel of other treatment modalities – elastic recoil. This is achieved by forcing and then holding the vessel outwards; by definition, in a limited space this has to be at the expense of adjacent structures. Whilst in the majority of cases altering thoracic cavity relationships will not result in a problem, in some settings there can be issues. This is particularly true after a Damus-Kaye-Stansel or Norwood type palliation where the reconstructed systemic outflow tract can be large and, as a result, space within the thorax is at a premium. In this situation, the left pulmonary artery (LPA) appears to be particularly vulnerable to compression between the neo-aorta and the left bronchus. This is reflected in the high prevalence of LPA stenosis2. Obstructive pulmonary arterial lesions are unwelcome in this vulnerable group. As a result, most successful congenital cardiac programmes have tended to be aggressive in identifying and tackling PA stenoses along the path to Fontan completion. However, over recent years evidence has begun to accumulate that, in a “battle” between the LPA and the left bronchus, within a limited space, when PA stents are brought in as “reinforcements”, it is the airway that most often pays a price with up to 30% of post-stent computed tomography (CT) scans demonstrating a stent-related mass effect affecting the bronchus3. Clinical sequelae are variable and not necessarily predictable but in bronchial compression there is an undoubted clinical burden including the requirement for longer-term ventilation and in some cases death attributed to respiratory-related illness3. Even if a patient is relatively asymptomatic, bronchial compression is concerning because the same counsel of perfection that drives elimination of pulmonary arterial stenoses in patients on a Fontan pathway would also advocate elimination of all airway and respiratory issues where possible, the ultimate goal being to achieve a perfect ventilation-perfusion match.
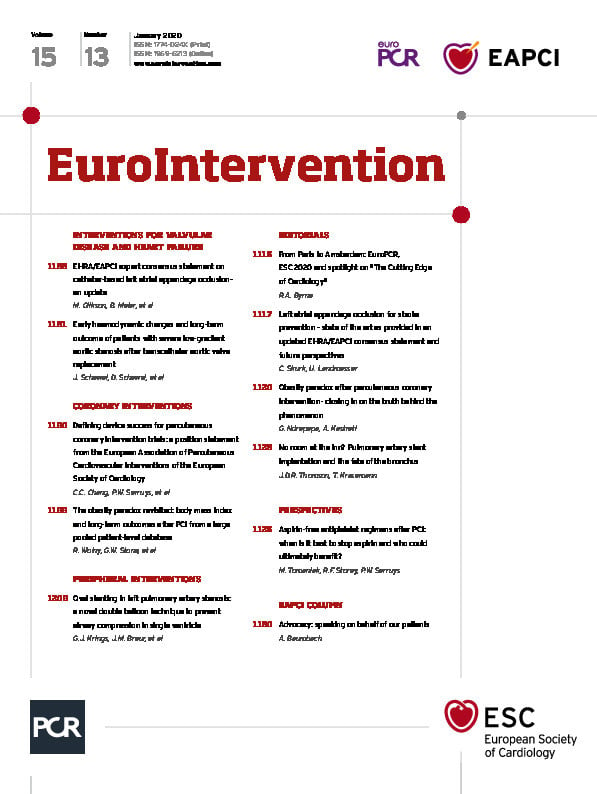
Since the recognition of stent-related bronchial compression, several authors have described techniques aimed at tackling or limiting the problem. These range from the use of concomitant bronchoscopy to guide the degree of stent dilation at implantation4 to planned procedural external cardiac compression to alter the geometry of the stents within the chest, thereby freeing up thoracic space for the airway5. In this issue of EuroIntervention, Krings and co-workers contribute to this body of knowledge by describing a novel method for “ovalising” LPA stents either at implant or post previous deployment where the airway is potentially compromised6.
The series is small – only 11 patients – but even so makes a reasonably convincing argument that with multiple balloons stents can be altered from a traditional circular shape to adopt oval or even trapezoid shapes within the artery, with the result being more thoracic space for the adjacent airway. The key is to ensure that the “elongation” takes place in the superior-inferior vector to shorten the stent in its anterior-posterior line, thereby maximising space for the airway. This is clearly quite a technical undertaking requiring not only multiple sheaths and wires but in some instances the use of a steerable sheath to ensure correct balloon orientation within the stent. This sort of venous access may not be possible in very small children and as a result a concern is, as the authors themselves point out, that there may be an age window beyond which bronchial remodelling may not occur and as a result a procedure of this complexity, when it becomes technically possible, might be too late. It should be noted that nearly all of the stents deployed were of an open or semi-open cell construction which are well suited to this sort of moulding – whether the technique can be consistently applied to the more traditional closed cell designs is uncertain.
In this series the anatomy (both vascular and airway) was delineated at the time of the procedure using rotational angiography. The unit in Utrecht have been long-standing advocates of this approach to catheter procedural planning. Whilst rotational angiography undoubtedly has the ability to identify key vascular/airway relationships, it has one overwhelming weakness, namely that the anatomy is only explored at the time of the procedure itself and not before, making planning a procedural rather than a preprocedural endeavour. For such a complex intervention this may be considered a suboptimal approach; for most units high-quality preprocedural computerised tomography (or possibly magnetic resonance imaging [MRI], although this is less reliable in airway delineation) would seem a worthwhile investment, even accepting the additional radiation dose. Next-generation catheter laboratory technology is already moving to high-level image integration. It is probable that information from preoperative 3D imaging could be integrated into the catheter procedure itself and used to guide elements of the procedure, thereby saving both on contrast and on radiation dose.
Several additional questions arise from this work. Although naturally the pulmonary arteries are oval not circular structures, might a rigid non-circular stent have deleterious effects on passive flow in a venous circuit7? Are there issues with re-dilation of oval or trapezoid stents in line with somatic growth? Will the technique work in other settings, e.g., post repair of complex pulmonary atresia where sometimes airway compression can be an issue but flow is pulsatile and under higher pressure? And, probably most important of all, why in this series did some patients’ airways not respond to these decompression exercises even when the procedure (on the face of it) was successful? Is this really an age or developmental phenomenon or are there other more complex issues at play?
Whatever the answers to these questions the authors should be congratulated on an important contribution to a particularly difficult problem.
Conflict of interest statement
J. Thomson is a proctor/consultant for Edwards Medical and Gore Medical. T. Krasemann has no conflicts of interest to declare.