Current drug-eluting stents lead to excellent long-term clinical outcomes, with small differences between the most popular products1. This indicates a dominant impact of the drug, and it is therefore not surprising that the design of the stent platforms received less attention during the last few years. Of course, there are a few exceptions here, like the bioabsorbable stents, where the use of unconventional materials requires innovative stent designs, or the dedicated bifurcation stents, designed to fit the complex bifurcation anatomy.
The paper of Hanratty and Walsh2, however, puts the design of standard metallic stents back in the spotlight. They report three interesting complication cases during which longitudinal compression of a previously delivered stent occurred. In each case, this complication was resolved by postdilating the distorted stent region and by deploying an additional stent if needed. The authors consider this longitudinal stent compression as a “new” complication and attribute it to the fact that more challenging lesions are being treated, as well as to general evolutions of the stent designs.
There have indeed been a few general design trends during the last decade. The strut thickness of the most used platforms is now below 100 microns and the flexibility and deliverability of the stents has been increased, often by reducing the number of connecting or bridging members between the adjacent expandable ring elements. It should be emphasised, however, that there are still important differences between the available platforms as illustrated in Figure 1. Some stent designs consist of multiple circumferential ring elements, while others have a helical strut pattern. The number of bridging members still varies from stent to stent, and their design ranges from simple connections between two peaks to longer elements with a more complex shape. Furthermore, stent deployment can result in a peak-to-peak or a peak-to-valley strut architecture which will also affect resistance against longitudinal compression. All these design differences will undoubtedly lead to a significant variation between the longitudinal stiffness and strength of the available devices. Of course, longitudinal compression can occur with any design, as long as the axial force is high enough, but it is highly likely that the occurrence of this complication will be design dependent.
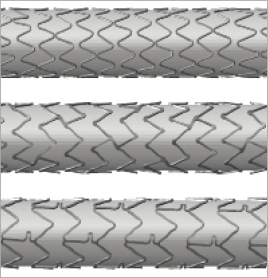
Figure 1. Illustration of the design variations between some of the currently used drug-eluting stents (top: Integrity Resolute stent [Medtronic, Minneapolis, MN, USA]; middle: Promus Element [Boston Scientific, Natick, MA, USA], bottom: Xience Prime [Abbott Vascular, Redwood City, CA, USA]). These expanded stent geometries were obtained through finite element analyses.
Two of the three reported cases involve stent deployment within the distal left main. This typically requires stenting across the left main bifurcation, and leads thus to a stent within two vessel segments with a substantially different diameter. According to the consensus document of the European Bifurcation Club3, this stent should be sized according to the distal vessel diameter, which will inherently lead to serious malapposition in the proximal main branch after initial stent deployment4. At this stage, the proximal stent segment is floating within the lumen, making it more vulnerable to longitudinal compression. This is again an argument in favour of dedicated (left main) bifurcation stents with a tapered balloon that immediately leads to good stent strut apposition in both the distal and the proximal segment. When using standard stents, care should be taken as long as the stent is underexpanded.
Hanratty and Walsh suggest that stent manufacturers should report longitudinal strength using a standardised assessment procedure. This would certainly be useful, as these data could, for example, be employed to select a stiffer stent to treat aorta-ostial disease. Maybe it is time to leave the idea of one design fits all behind us.
Conflict of interest
Peter Mortier and Matthieu De Beule are shareholders of FEops, an engineering consultancy spin-off from Ghent University, and have served as consultants for several medical device companies.
References

