
Aortocaval fistula (ACF) as a result of abdominal aortic aneurysm (AAA) rupture is very rare, and associated morbidity and mortality are very high. Open surgical and endovascular treatment, even combined as a hybrid procedure, is also associated with high complication rates. Surgical approaches include ACF ligature and aneurysm resection. An endovascular approach by aortic endograft deployment (endovascular aneurysm repair [EVAR]) may result in acute right heart failure or insufficient AAA and ACF coverage. We present a staged approach for percutaneous ACF treatment by escalating endovascular means.
A 59-year-old patient presented with signs of congestive heart failure and abdominal pain. Auscultation revealed loud periumbilical continuous machine-type bruits with systolic accentuation. Ultrasound depicted volume overload-related right heart insufficiency combined with consecutive congestion-induced liver cirrhosis. Contrast-enhanced computed tomography (CT) showed an underlying AAA (diameter 7.5 cm) associated with a large ACF to the infrarenal vena cava (IVC).
After urgent EVAR (Aorfix™ Endovascular Stent Graft; Lombard Medical, Didcot, United Kingdom), based on an interdisciplinary decision, a large endoleak type 2 (EL2) was obvious and ACF persisted (Moving image 1). Two weeks later, the inferior mesenteric artery was embolised using coils (Nester® Embolization Coil, 0.035”; Cook Medical, Bloomington, IN, USA).
Percutaneous CT-guided glue embolisation (Glubran®2; GEM Srl, Viareggio, Italy) of multiple lumbar arteries potentially feeding the ACF was aborted, because persistent high flow prevented ACF occlusion, resulting in asymptomatic minor pulmonary embolism.
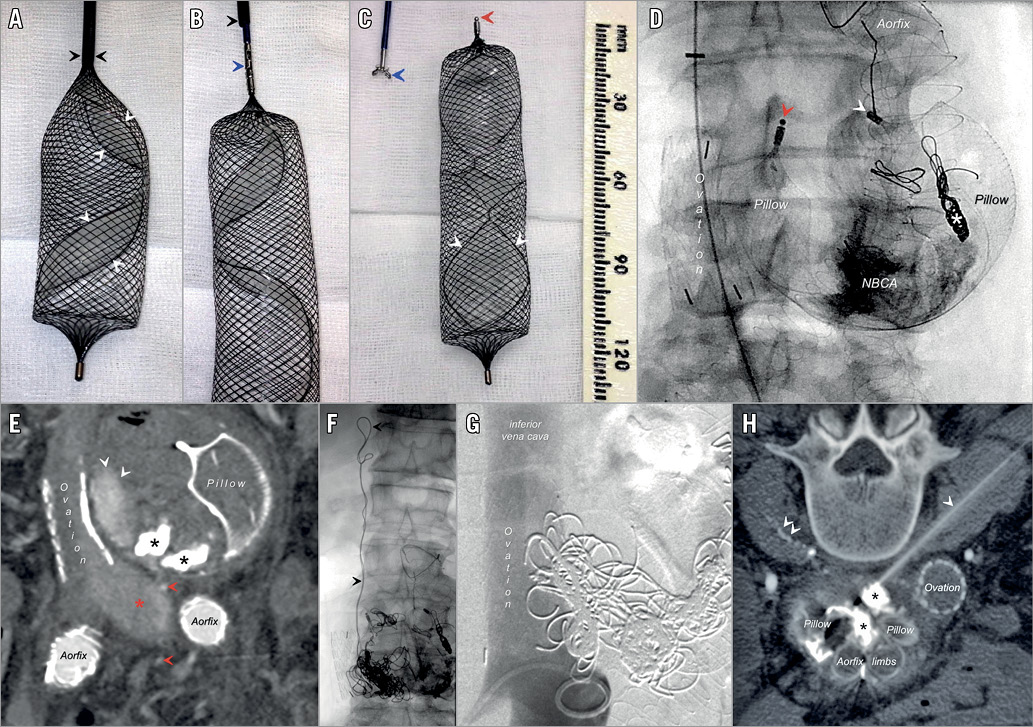
Considerable flow reduction was achieved by transjugular cannulation (Moving image 2) and deployment of a large vascular plug (Pillow AAA Occlusion Device, 25/80 mm, 9 Fr; AndraTec GmbH, Koblenz, Germany) into the aneurysm sac (Panel A-Panel C, Moving image 3). The occluder used was a clinical investigational device. The procedure was performed after informed consent was obtained from the patient. Direct coverage of ACF was achieved by transjugular off-label venous stenting of the IVC (Ovation® Abdominal Stent Graft Platform, iliac extension EX22-22-45; Endologix Inc., Irvine, CA, USA) (Panel D, Panel E, Moving image 4).
Seven months later, persisting EL2 and low-flow ACF (Moving image 5) was treated by CT-guided percutaneous coil embolisation of the aneurysm and lumbar arteries. Coil dislocation into the IVC via the ACF (Panel F) necessitated immediate endovascular transvenous coil retrieval and repositioning (Moving image 6), which was combined with additional coil embolisation of the ACF (22x Ruby® Penumbra Occlusion Device [POD®] detachable coils; Penumbra Inc., Alameda, CA, USA) (Panel G).
Finally, EL2 and ACF were successfully treated by percutaneous glue embolisation of the median sacral artery four months later (Panel H).
Follow-up after another six months showed a completely recovered and asymptomatic patient. Contrast-enhanced ultrasound and CT (Moving image 7) confirmed successful closure of the ACF, EL, AAA shrinkage and improvement of right heart insufficiency with decreasing liver stiffness indicating remodelling. Initial NT-proBNP (383.1 pg/ml) and elastography (2.53 m/s) normalised.
Generally, EVAR aims at instant aneurysm exclusion. In our case, stepwise flow reduction of the ACF was necessary, yielding successive reduction of right heart stress.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Coronal view of contrast-enhanced computed tomography depicts a persisting large aortocaval fistula post EVAR using Lombard’s Aorfix stent graft system.
Moving image 2. Fluoroscopy shows transjugular direct cannulation of the aortocaval fistula with a 4 Fr cobra catheter. The Aorfix stent graft is identified by the typical ring design and its fishmouth-like stent graft endings. Partial opacification of the aneurysm sac results from Lipiodol-mixed glue. The inferior mesenteric artery is occluded by coil embolisation.
Moving image 3. Transjugular deployment of a large vascular occluder (Pillow AAA Occlusion Devicee 25/80 mm) into the aortic aneurysm sac for coverage of the aortocaval fistula.
Moving image 4. Transjugular venous deployment of an aortic stent graft into the inferior vena cava for direct coverage of the aortocaval fistula (Ovation iliac extension EX22-22-45 mm). Transfemoral access was avoided to minimise the risk of infection after previous EVAR.
Moving image 5. Contrast-enhanced ultrasound shows the bifurcated aortic stent graft (Aorfix) and vascular occlusion device (Pillow AAA Occlusion Device). After injection of 1.2 ml SonoVue® (Bracco Imaging, Milan, Italy) persistence of a large endoleak type 2 and aortocaval fistula is proven by intense opacification of the inferior vena cava by contrast bubbles.
Moving image 6. Transvenous repositioning of a coil, which was inserted via percutaneous access to the abdominal aortic aneurysm and dislocated via the patent aortocaval fistula into the inferior vena cava.
Moving image 7. Transvenous repositioning of a coil, which was inserted via percutaneous access to the abdominal aortic aneurysm and dislocated via the patent aortocaval fistula into the inferior vena cava.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Coronal view of contrast-enhanced computed tomography depicts a persisting large aortocaval fistula post EVAR using Lombard’s Aorfix stent graft system.
Moving image 2. Fluoroscopy shows transjugular direct cannulation of the aortocaval fistula with a 4 Fr cobra catheter. The Aorfix stent graft is identified by the typical ring design and its fishmouthlike stent graft endings. Partial opacification of the aneurysm sac results from Lipiodol-mixed glue. The inferior mesenteric artery is occluded by coil embolisation.
Moving image 3. Transjugular deployment of a large vascular occluder (Pillow AAA Occlusion Devicee 25/80 mm) into the aortic aneurysm sac for coverage of the aortocaval fistula.
Moving image 4. Transjugular venous deployment of an aortic stent graft into the inferior vena cava for direct coverage of the aortocaval fistula (Ovation iliac extension EX22-22-45 mm).Transfemoral access was avoided to minimise the risk of infection after previous EVAR.
Moving image 5. Contrast-enhanced ultrasound shows the bifurcated aortic stent graft (Aorfix) and vascular occlusion device (Pillow AAA Occlusion Device). After injection of 1.2 ml SonoVue® (Bracco Imaging, Milan, Italy) persistence of a large endoleak type 2 and aortocaval fistula is proven by intense opacification of the inferior vena cava by contrast bubbles.
Moving image 6. Transvenous repositioning of a coil, which was inserted via percutaneous access to the abdominal aortic aneurysm and dislocated via the patent aortocaval fistula into the inferior vena cava.
Moving image 7. Transvenous repositioning of a coil, which was inserted via percutaneous access to the abdominal aortic aneurysm and dislocated via the patent aortocaval fistula into the inferior vena cava.

