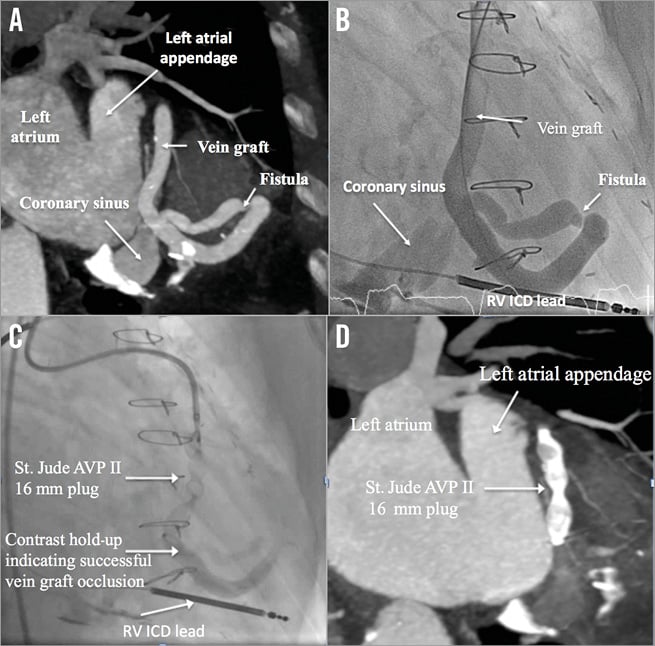
The patient was a 76-year-old male under regular cardiology follow-up for progressive shortness of breath secondary to an iatrogenic aortocoronary venous fistula following coronary artery bypass surgery in 2002. He also had an ICD implanted in 2012. Computerised tomographic (CT) and invasive diagnostic angiography are shown in Panel A and Panel B, respectively. The patient was discussed in our joint cardiology and cardiothoracic team meeting, which concluded that the risks of surgery outweighed any benefit. Therefore, a percutaneous option for closure of the fistula was chosen. The procedure was performed via the right femoral artery, initially with a 6 Fr sheath exchanged for a 9 Fr short sheath. A 6 Fr AL-1 guide was used to cannulate the vein graft and an ASAHI® SION™ blue 180 cm guidewire (ASAHI INTECC, Aichi, Japan) passed allowing a 6 Fr GuideLiner® catheter (Vascular Solutions, Inc., Minneapolis, MN, USA) to provide additional support to deliver a 260 cm J-tipped Amplatzer stiff wire (Cook Medical, Bloomington, IN, USA) to the distal vein graft. The 6 Fr AL-1 guide and GuideLiner were carefully withdrawn under radiographic guidance and replaced with a 90 cm long 7 Fr Pinnacle® Destination® guiding sheath (Terumo Corp., Tokyo, Japan) passed on the 260 cm Amplatz stiff wire. A 16 mm AMPLATZER™ Vascular Plug II (AVP II) (St. Jude Medical, St. Paul, MN, USA) was then positioned and deployed with subsequent contrast hold-up indicating occlusion of the vein graft (Panel C). The patient reported an improvement in symptoms on subsequent follow-up and had a repeat CT scan (Panel D) six months post procedure demonstrating no contrast, therefore suggesting a completely occluded vein graft.
Conflict of interest statement
The authors have no conflicts of interest to declare.