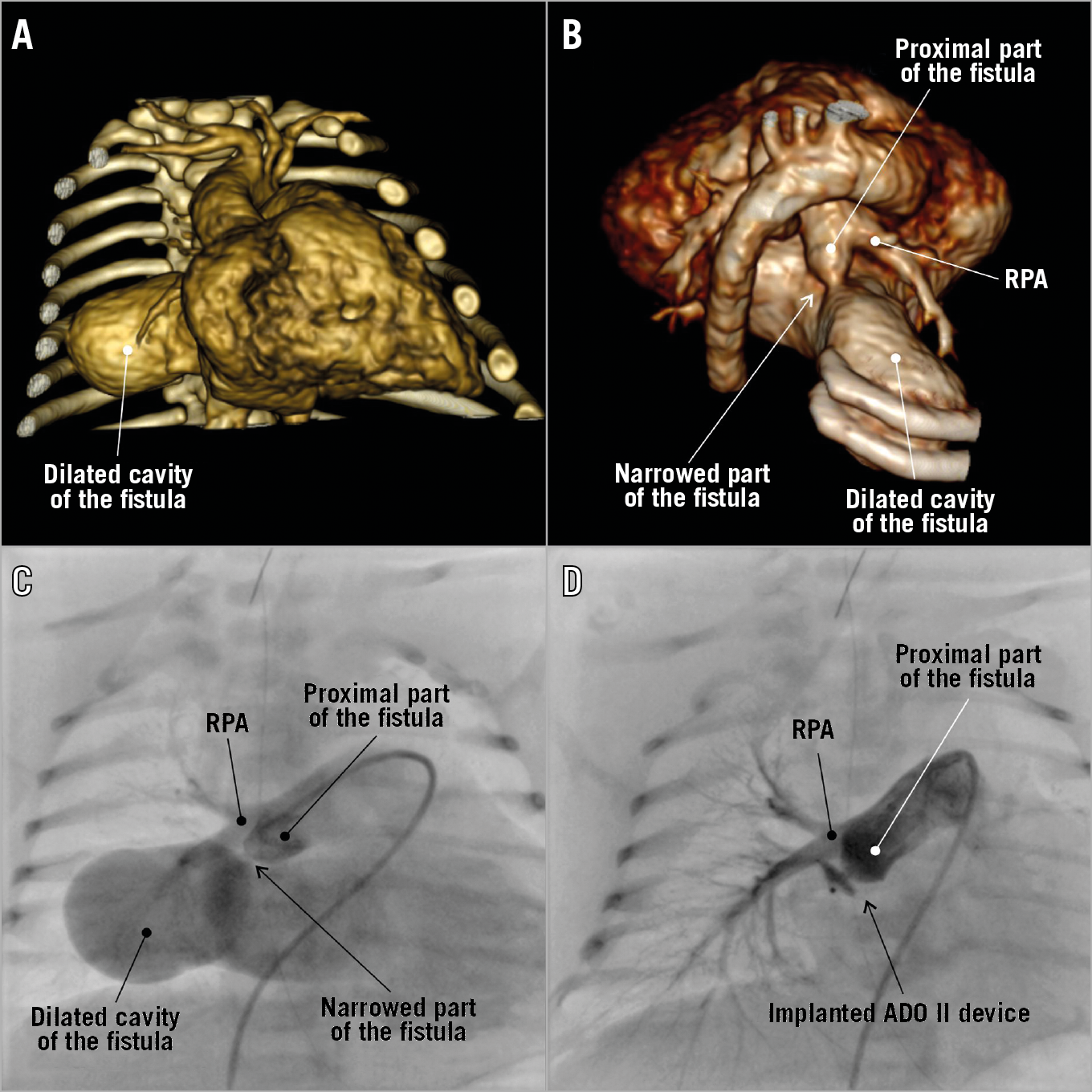
Figure 1. A fistula between the right pulmonary artery and the left atrium presented on 3D volume-rendered computed tomography reconstructions (A & B). Angiography performed before (C) and after implantation (D) of an AMPLATZER Duct Occluder II device.
A huge fistula between the right pulmonary artery and the left atrium was found prenatally in the 27th week of gestation and associated with cardiomegaly related to left heart enlargement (Moving image 1). The fistula presented proximal narrowing close to the right pulmonary artery and partially limited the inflow. The maximum pressure gradient was initially 36 mmHg and gradually increased to 49 mmHg during pregnancy. The small and tortuous ductus arteriosus resulted in abnormal limited retrograde flow from the aorta to the pulmonary arteries. During pregnancy, the foetus received transplacental treatment with digoxin. After birth (37 weeks of gestation, Caesarean section, body weight 4,000 g), the child was initially in good condition but within hours deteriorated rapidly; because of respiratory failure and increasing cyanosis, the child was given continuous positive airway pressure support and eventually mechanical ventilation. Post-natal echocardiography confirmed the presence and anatomy of a fistula that exhibited mildly restricted inflow through its narrowest region, with a maximum pressure gradient of 28 mmHg (Moving image 2). In addition to these findings, enlargement of the left atrium and the left ventricle was observed, and mildly impaired left ventricle systolic function was noted. All four pulmonary veins were properly connected with the left atrium. Because of the patient’s severe clinical condition, we performed an urgent diagnostic computed tomography (CT) scan on the first day of life. This scan showed the precise anatomy of the proximal fistula, which had a minimum diameter of 3 mm and an aneurysmal cavity (32×27×20 mm) widely connected to the left atrium (Figure 1A, Figure 1B, Supplementary Figure 1, Moving image 3). In this type of case, despite good surgical results, less invasive percutaneous treatment is currently the preferred method of treatment even in neonates1,2,3,4. In our patient, the narrowed region was assessed as suitable for interventional treatment, and the patient was deemed qualified for urgent cardiac catheterisation because of rapid clinical deterioration. During the procedure, a 4 Fr AMPLATZER™ TorqVue™ sheath (Abbott Vascular, Santa Clara, CA, USA) was introduced from the major pulmonary artery through the narrowed region of the fistula, and a 4/4 mm AMPLATZER™ Duct Occluder II device (Abbott Vascular) was successfully implanted in this position (Figure 1C, Figure 1D, Moving image 4, Moving image 5). Very minor residual flow and contrast retention in the dilated cavity of the fistula were observed on control angiography, while flow into the right pulmonary artery and pulmonary venous return remained unobstructed. The child remained in good condition throughout the 15-month follow-up period, during which antiplatelet therapy was initially given. The size of the left atrium and fistula decreased continuously on transthoracic echocardiography repeated every three months, with the residual shunt close to the detection limit, leading to the consensus that no further imaging studies are currently necessary.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Fistula between the right pulmonary artery and the left atrium on prenatal echocardiography.
Moving image 2. Fistula between the right pulmonary artery and the left atrium on echocardiography after birth showing a high left parasternal short axis.
Moving image 3. 3D volume-rendered reconstruction of the fistula between the right pulmonary artery and the left atrium.
Moving image 4. Angiography performed on the pulmonary trunk before the interventional procedure.
Moving image 5. Angiography of the right pulmonary artery performed after percutaneous implantation of the AMPLATZER Duct Occluder II device into the narrowed region of the fistula.