An 80-year-old man with severe mitral regurgitation was assessed for MitraClip® (Abbott Vascular, Menlo Park, CA, USA) implantation. Transoesophageal echocardiography showed a dilated cardiomyopathy with a left ventricular ejection fraction of 25% and an isolated cleft in the posterior mitral valve leaflet resembling a trileaflet mitral valve with restrictive severe regurgitation (Figure 1). The patient was turned down for mitral surgery due to severe concomitant comorbidities including coronary artery disease, atrial fibrillation, diabetes and renal insufficiency.
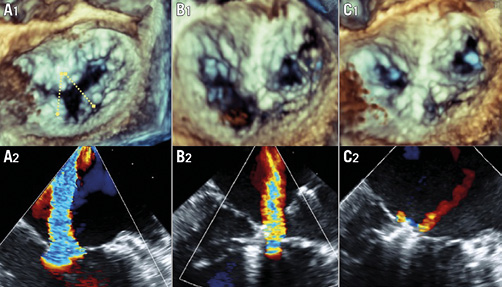
Figure 1. MitraClip repair of a trileaflet mitral valve. 3D-TEE imaging sequence of the trileaflet mitral valve with the projected “inverted V” strategy before treatment (A1), after the first MitraClip (B1) and after the second MitraClip (C1). 2D-TEE colour sequence of the mitral regurgitation showing severe regurgitation before treatment (A2), moderate after the first MitraClip (B2) and trace after the second MitraClip (C2).
Considering the severe functional limitation of the patient and despite the challenging anatomy of the mitral valve, the patient was accepted for percutaneous repair. A two-MitraClip with an “inverted V” strategy was planned as it was considered the most feasible technique for assuring leaflet insertion as well as to create a double-orifice valve. The echocardiographic result was satisfactory as the mitral regurgitation was reduced from severe to trace and transvalvular gradient was 3.4 mmHg. Patient evolution was excellent up to the second day post procedure when he suddenly died as a result of a massive intracranial haemorrhage during warfarin reintroduction while on heparin. Chest x-ray confirmed the absence of device embolisation and dual anticoagulation therapy was felt to be the main cause of the event.
The present case illustrates an uncommon mitral anatomy with an isolated posterior mitral leaflet cleft resembling a trileaflet mitral valve that was successfully repaired using an “inverted V” strategy with two MitraClips. Wyss et al1 found the described anatomy in 0.11% of patients who underwent an echocardiographic study for any reason. In those patients, severe mitral regurgitation was present in 50% of cases1. Although the presence of a posterior cleft is generally considered an anatomical contraindication for MitraClip repair2, the intervention was still performed as the patient presented disabling symptomatology, the procedure was considered technically feasible and cardiac surgery was turned down. A two-MitraClip “inverted V” strategy was preferred over a two-MitraClip “parallel” strategy as we anticipated a smaller central orifice between devices while keeping good leaflet insertion. Since the fatal outcome was unlikely to be directly related to the procedure, the authors believe that the present report is relevant as it may help operators in future procedures with similar anatomies.
Conflict of interest statement
A. Asgar is consultant for Abbott Vascular. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. 3D-TEE imaging of the trileaflet mitral valve.
Moving image 2. 3D-TEE imaging after the first MitraClip.
Moving image 3. 3D-TEE imaging after the second MitraClip.
Moving image 4. 2D-TEE colour imaging of the mitral regurgitation showing severe regurgitation before treatment.
Moving image 5. 2D-TEE colour imaging of the mitral regurgitation showing mild-trace regurgitation after deployment of the second MitraClip.

