Abstract
Aims: Transcatheter mitral valve repair has become a promising alternative treatment option for severe symptomatic mitral regurgitation in patients at high risk for open heart surgery with heart-lung bypass.
Methods and results: We describe the first successful procedure of mitral clipping through a right lateral mini-thoracotomy via the right upper pulmonary vein in a patient with an agenesis of the inferior vena cava. The set-up of the MitraClip system on a separate table located at 70° on the right side of the patient and the fixation of the steerable sheath at the entry into the thorax with constant posterior pressure enabled clip implantation using the usual manoeuvres with marked reduction of the mitral insufficiency.
Conclusions: The access through the right upper pulmonary vein using the usual right mini-thoracotomy enabled a successful mitral clipping even in the absence or occlusion of the inferior vena cava.
Introduction
Percutaneous treatment using the MitraClip® system (Abbott Vascular - Structural Heart, Menlo Park, CA, USA) has become an important treatment option in older patients with severe mitral regurgitation and multiple comorbidities. These patients with extreme operative risk for open heart surgery on cardiopulmonary bypass often represent challenging cases and are in contrast to the intermediate risk population assessed in the EVEREST II trial with the exception of patients included in the High Risk Registries1. Some patients cannot be treated using the regular access through the femoral vein due to an inferior vena cava filter or, as in this case, a congenital absence of the inferior vena cava. The access through the superior vena cava is difficult and dangerous, and has not been performed safely to our knowledge. Frerker et al presented a case with an access through the right atrium earlier this year (2013), but this access required a thoracotomy and a muscular puncture of the right atrium with subsequent transseptal puncture2. In this case report, we describe the first successful MitraClip procedure directly through the pulmonary vein in a high-risk patient with missing inferior vena cava.
Case report
A 71-year-old male presented to an affiliated hospital two months ago with dyspnoea (NYHA Class IV) due to pulmonary oedema. The echocardiogram showed a severe mitral regurgitation with a broad jet between A1/P1 and A2/P2. He had severe pulmonary hypertension with pressures of 80/30 mmHg and moderately reduced left ventricular ejection fraction of 45%. He had three-vessel disease with implantation of three drug-eluting stents in the LAD in June 2012 with a good result documented in a coronary angiography in July 2013. The patient had sinus rhythm with a heart rate of 75/min at admission, the QRS length was 92 msec, and there were no signs of acute ischaemia. He had a congenital agenesis of the inferior vena cava with collateral venous circulation (Figure 1, Moving image 1). Previously, he had had multiple hospitalisations due to recurrent pulmonary oedema and had been treated medically for his dyspnoea due to the mitral regurgitation at different university hospitals. A surgical approach with cardiopulmonary bypass was declined because of the factor V deficiency and the high perioperative risk (EuroSCORE II of 25.8%). Despite intensive medical treatment, the patient continued to have severe shortness of breath with minimal exertion. After discussion of the case in our Heart Team, a MitraClip procedure was recommended through the right upper pulmonary vein.
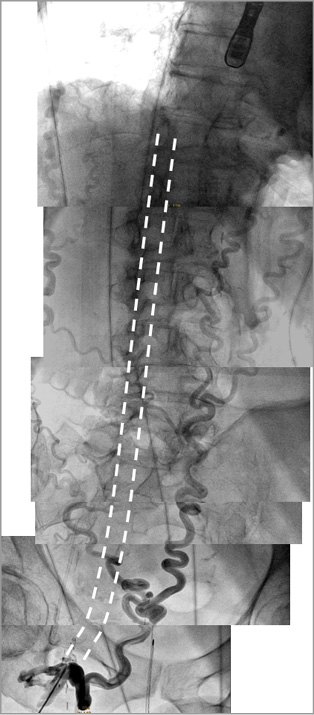
Figure 1. Missing inferior vena cava with development of collaterals in the venous angiogram. The dotted lines depict the usual location of the inferior vena cava.
Current procedure
We performed a right lateral mini-thoracotomy within the sixth intercostal space as used for regular mitral repair and gained access to the right upper pulmonary vein with continuing ventilation of both lungs. The MitraClip system was placed at a 70 degree angle on an extra table to the right side of the patient. After placement of preparatory sutures and puncture of the right pulmonary vein close to the left atrium, we placed an Amplatzer J wire through the mitral valve in the left ventricle and introduced the steerable sheath into the left atrium. Unfortunately, the first clip caught a very prominent ridge at the entry of the left inferior pulmonary vein directly after introduction of the clip device system and before opening of the clip. Within the left lower pulmonary vein, the clip could neither be adequately opened nor retracted. We had to deploy the clip there, which remained stable at this location with good flow in the pulmonary vein. In order to avoid another posterior clip location, we applied posterior pressure on the sheath at the entry into the thorax with an additional 30° anterior (counterclockwise) rotation, thereby moving the sheath tip to an anterior position. Small cranial/caudal or anterior/posterior movements of the sheath just outside the thorax resulted in relevant deflections of the sheath tip to the contralateral direction. The fixation of the sheath in the desired position was therefore necessary: a wet compress within the fixation allowed rotational and small longitudinal movements. We used the Amplatzer wire to position the steerable sheath just above the mitral regurgitation jet (Figure 2) and advanced the second clip through the valve. An additional “M” rotation of the device was not necessary. The position and orientation of the clip were checked as usual. The first grasp with this clip resulted in a marked reduction of the mitral regurgitation from severe to mild with a good tissue bridge (Figure 3-Figure 5, Moving image 2, Moving image 3) and an acceptable transmitral mean gradient of 5-6 mmHg. The overall set-up is displayed in Figure 6.
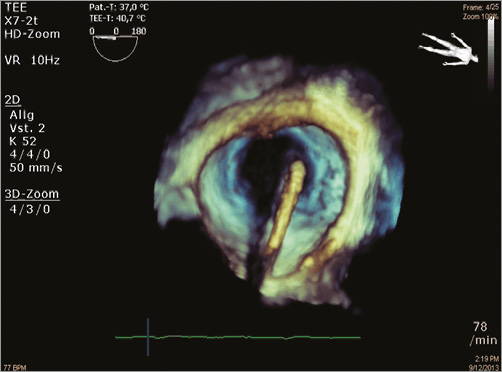
Figure 2. Necessary 3D echo confirmation of the position of the guide tip above the mitral valve before clip advancement.
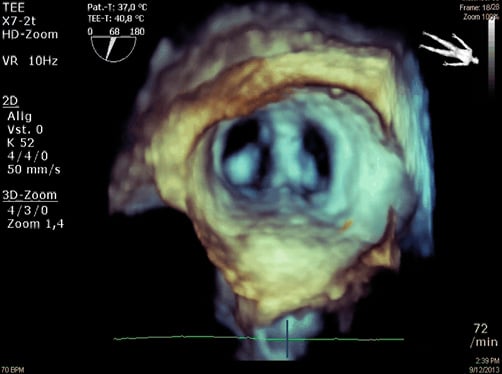
Figure 3. 3D echo showing the good tissue bridge after clip deployment at the origin of the previous regurgitation jet.
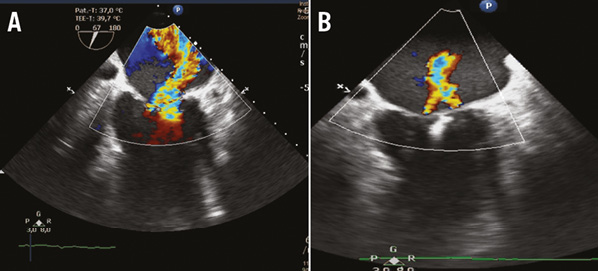
Figure 4. Mitral regurgitation before (A) and after implantation of the MitraClip (B) in the transoesophageal echocardiography.

Figure 5. Fluoroscopy image just before release of the second clip within the valve and the stable previous clip at the ridge of the inferior left pulmonary vein.
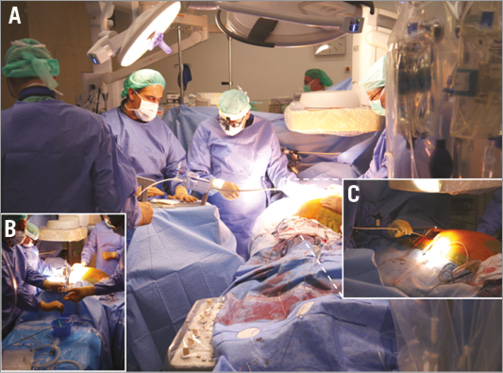
Figure 6. Overall set-up (A) with the MitraClip device on the separate table (previously used for device preparation) (B) placed at 70° to the right side of the patient, allowing sheath and clip insertion through the thoracotomy (C).
The patient was rapidly weaned and mobilised within 24 hours. At discharge, he showed a marked clinical improvement with dyspnoea NYHA Class I.
Discussion
The vast majority of around ten thousand MitraClip procedures were performed in old patients with high risk for open heart surgery and cardiopulmonary bypass. Patients with severe mitral regurgitation and inferior vena cava filters or, as in our case, with missing inferior vena cava, were excluded from interventional treatment using the MitraClip device. One case report earlier this year (2013) described a patient with cardiogenic shock in the presence of severe mitral regurgitation with agenesis of the inferior vena cava. This patient was treated with implantation of two MitraClips after direct puncture of the right atrium through a thoracotomy, but this access required an additional transseptal puncture and may apply higher shear forces on the heart2.
In this case report, we described a MitraClip procedure over the right upper pulmonary vein using the usual right mini-thoracotomy access. A pitfall of this procedure is the high manoeuvrability of the device within the heart, which resulted in the deployment of a clip at the prominent ridge of the inferior vena cava. We learned that constant posterior pressure with fixation of the guide at the entry into the thorax is essential for the correct anterior position of the guide tip over the mitral valve. This position enabled a regular grasp with a good overall procedural result and clinical outcome. The application of this technique will allow the treatment of patients with unavailable access through the inferior vena cava, deemed untreatable to date.
Conclusion
Our procedure presents a novel “first-in-man” MitraClip access through the right upper pulmonary vein using the usual right mini-thoracotomy, enabling successful mitral clipping even in the absence or occlusion of the inferior vena cava.
| Impact on daily practice A missing or blocked inferior vena cava is a rare limitation for the MitraClip procedure, but it represents a major challenge for a successful accomplishment. This first-in-man MitraClip deployment through the usual right mini-thoracotomy demonstrates the advantages with a short distance to the valve, very good accessibility and simple haemostasis of the pulmonary vein puncture, but also the pitfalls of this access, including the high manoeuvrability and need for stabilisation of the guide at the entrance of the thorax. This collaborative Heart Team approach without heart-lung bypass enabled the same-day weaning from ventilation and mobilisation of the patient with a significant reduction in mitral regurgitation. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Missing inferior vena cava with development of collaterals in the venous angiogram.
Moving image 2. Necessary 3D echo confirmation of the position of the guide tip above the mitral valve before clip advancement.
Moving image 3. 3D echo showing the good tissue bridge after clip deployment at the origin of the previous regurgitation jet.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1.
Moving image 2.
Moving image 3.

