Abstract
Aims: Limited data exist on long-term outcomes of patients with stent thrombosis (ST). Our aim was to describe the long-term outcomes after angiographically confirmed ST.
Methods and results: In this multicentre registry, consecutive cases of definite ST were identified between 2005 and 2013. Clinical and procedural characteristics, in-hospital outcomes and long-term survival up to five years were compared between those with and those without adverse cardiovascular and cerebrovascular events (MACCE), defined as all-cause mortality, myocardial infarction and stroke. Two hundred and twenty-one patients with 239 stent thrombosis events were identified. Patients who developed MACCE were older, less likely to be men, and less likely to have hypertension. Angiographic characteristics were similar. Patients who had a MACCE event showed a trend towards a lower likelihood of procedural success (86% vs. 91%, p=0.05). MACCE rates were 22% at one year and 41% at five years. All-cause mortality was 13% at one year and 24% at five years. On multivariable analysis, age, diabetes mellitus, active smoking and ST at a bifurcation were independently associated with the occurrence of MACCE up to five years.
Conclusions: Age, active smoking, diabetes mellitus and bifurcation disease are independently associated with long-term MACCE over a five-year follow-up period.
Introduction
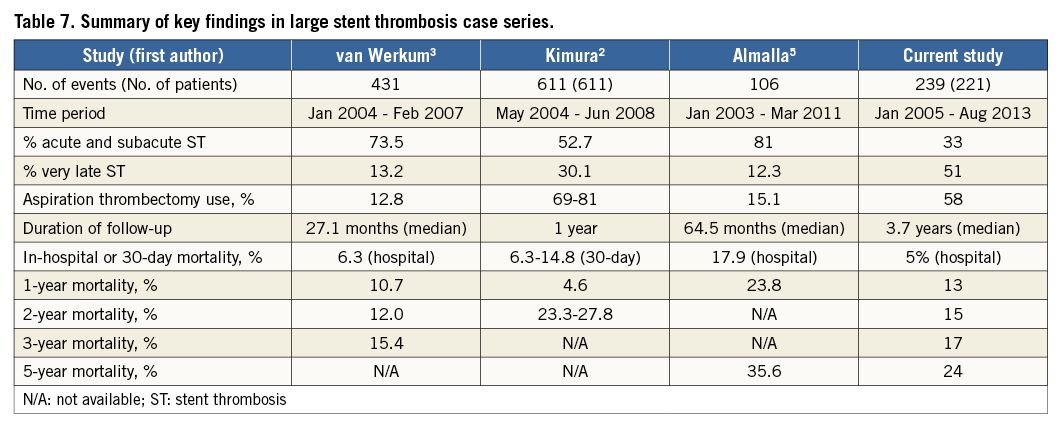
Stent thrombosis (ST) is a rare complication of coronary artery stenting that can result in significant morbidity and mortality. While earlier studies suggested high in-hospital mortality related to ST, more recent reports suggest in-hospital mortality between 5% and 14.8%1-4. In our previously published report based on a large multicentre registry, diabetes mellitus (DM) and bifurcation disease, but not type of percutaneous therapy, were also shown to be independently associated with in-hospital mortality4. Despite these and other data, information on the long-term outcomes of ST remains limited. Among other contemporary series, van Werkum et al3 reported two-year mortality rates of 12%, Kimura and colleagues2 reported two-year mortality rates of 28%, and Almalla et al5 reported five-year mortality rates of 36%. Longer-term outcomes and predictors of adverse long-term outcomes remain unclear. The aim of this study was to describe the long-term clinical outcomes of patients in a large, multicentre cohort of patients with angiographically confirmed ST.
Methods
STUDY DESIGN AND PATIENT SELECTION
The University of California ST registry comprises all cases of angiographic definite ST at five academic medical centres (University of California, Davis; University of California, San Diego; San Francisco Veteran’s Administration Hospital; San Francisco General Hospital; and University of California, San Francisco Moffitt-Long Hospital) from 2005-2013. Institutional review board approval at each site was obtained. The study has been registered at ClinicalTrials.gov with the identifier NCT00931502. Details of the study have been previously published4. Briefly, this study included retrospective review of ST occurring from January 2005 to April 2008, and prospective enrolment of subsequent patients up to 2013. Each case was reviewed by two interventional cardiologists for definite ST. Academic Research Consortium (ARC) criteria were used to determine timing of ST6. Only cases of angiographic definite ST were included in the registry.
Once identified, cases were reviewed for demographic, procedural, angiographic, and in-hospital outcomes4. Briefly, trained abstractors and physicians reviewed each medical chart for details of presentation, medications prior to admission, medication compliance, procedural details of coronary angiography and intervention, and long-term major adverse cardiovascular and cerebrovascular events (MACCE), defined as death, stroke, or repeat myocardial infarction. Discharge medications were assessed for all surviving patients. The study population was divided into two groups: those with and those without a MACCE event at up to five-year follow-up.
LONG-TERM OUTCOMES
Outcomes were identified by retrospective chart review. For prospectively recruited patients, outcomes were also identified by telephone interviews. The primary endpoint of the study, MACCE (defined as all-cause mortality, MI, and stroke) was recorded up to five years after the initial ST event. Secondary endpoints were all-cause death, stroke, MI, definite and probable recurrent ST. Mortality after discharge was collected using the social security death index (SSDI), performed by research coordinators at each institution to verify death in the study population.
STATISTICAL ANALYSES
The study population was divided into those who had a MACCE at up to five years of follow-up, and those who did not. Clinical, anatomical and procedural characteristics were compared between both groups. Median values with interquartile ranges were used to describe continuous variables, and numerical values (percentages) were used for categorical variables. Continuous variables were compared using the Wilcoxon rank-sum test or t-test. Categorical values were compared by the chi-square test. The cumulative hazard of MACCE was plotted as a function of time. Predictors of MACCE were identified using a Cox proportional hazards model which included all predictors with a univariate association of <0.1 followed by stepwise elimination of non-significant predictors in order to avoid overfitting. A sensitivity analysis was also performed to assess predictors of long-term outcomes among patients who survived the initial hospitalisation. In this analysis, patients who had an adverse event in-hospital were excluded from the Cox proportional hazards model. All analyses were performed using Stata Version 11.2 (StataCorp, College Station, TX, USA). A p-value <0.05 was considered significant. All authors have read and agree to the manuscript as written.
Results
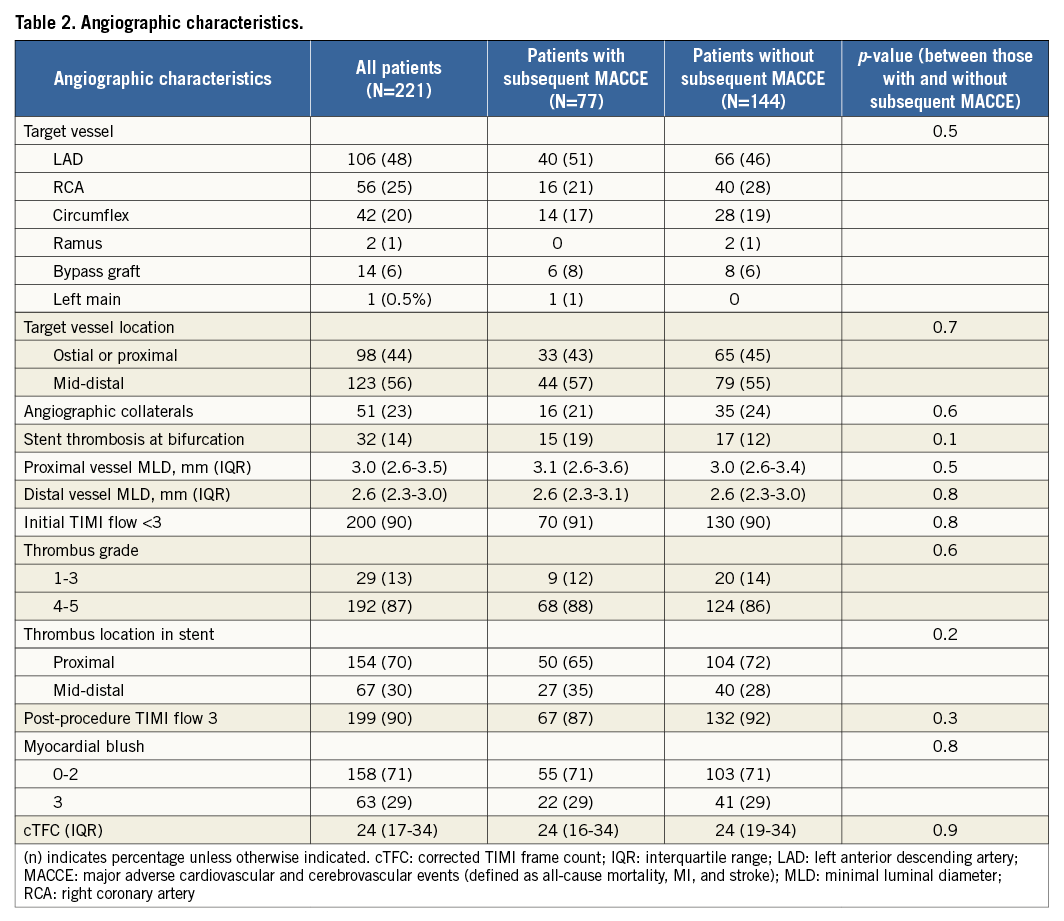
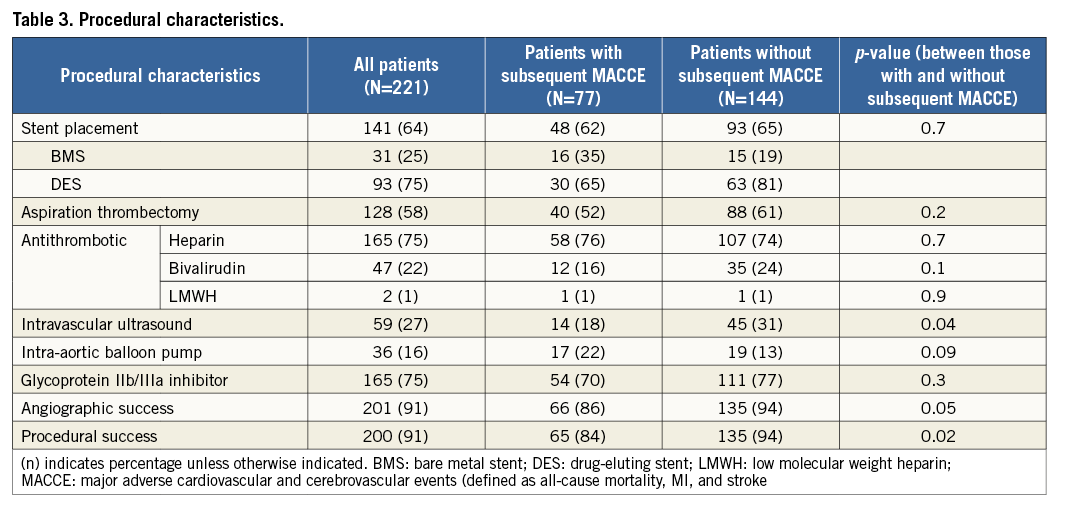
Between January 2005 and August 2013, 221 patients with 239 occurrences of angiographic definite ST were identified. In patients with multiple events, only the first event was included in the primary analysis. Table 1 shows the demographics and clinical characteristics of the entire cohort and for both groups of patients (with and without MACCE). Both groups were largely similar except that patients who subsequently developed MACCE were more likely to be older (65 vs. 60 years, p<0.001), less likely to be men (77% vs. 91%, p=0.003), and less likely to have hypertension (62% vs. 83%, p<0.001). Among 54 patients (24% of 221) not taking aspirin at the time of presentation with stent thrombosis, 44 were not taking aspirin due to medical non-compliance. Eight patients had the aspirin stopped perioperatively for elective or emergency surgery, and two patients had stopped aspirin due to a history of bleeding. In those cases, the patients were not on concomitant coumadin. There were no significant differences in angiographic characteristics at the time of ST between the two groups (Table 2). This included characteristics such as vessel size, location and involvement of a coronary bifurcation. Table 3 shows the procedural characteristics in both groups of patients. There were no significant differences in the use of antithrombotic agents, types of stent (DES vs. BMS), or adjunctive glycoprotein IIb/IIIa antagonists. However, patients who had a subsequent MACCE event were less likely to undergo intravascular ultrasound and were less likely to have procedural success (each 84% vs. 91%, p=0.02).
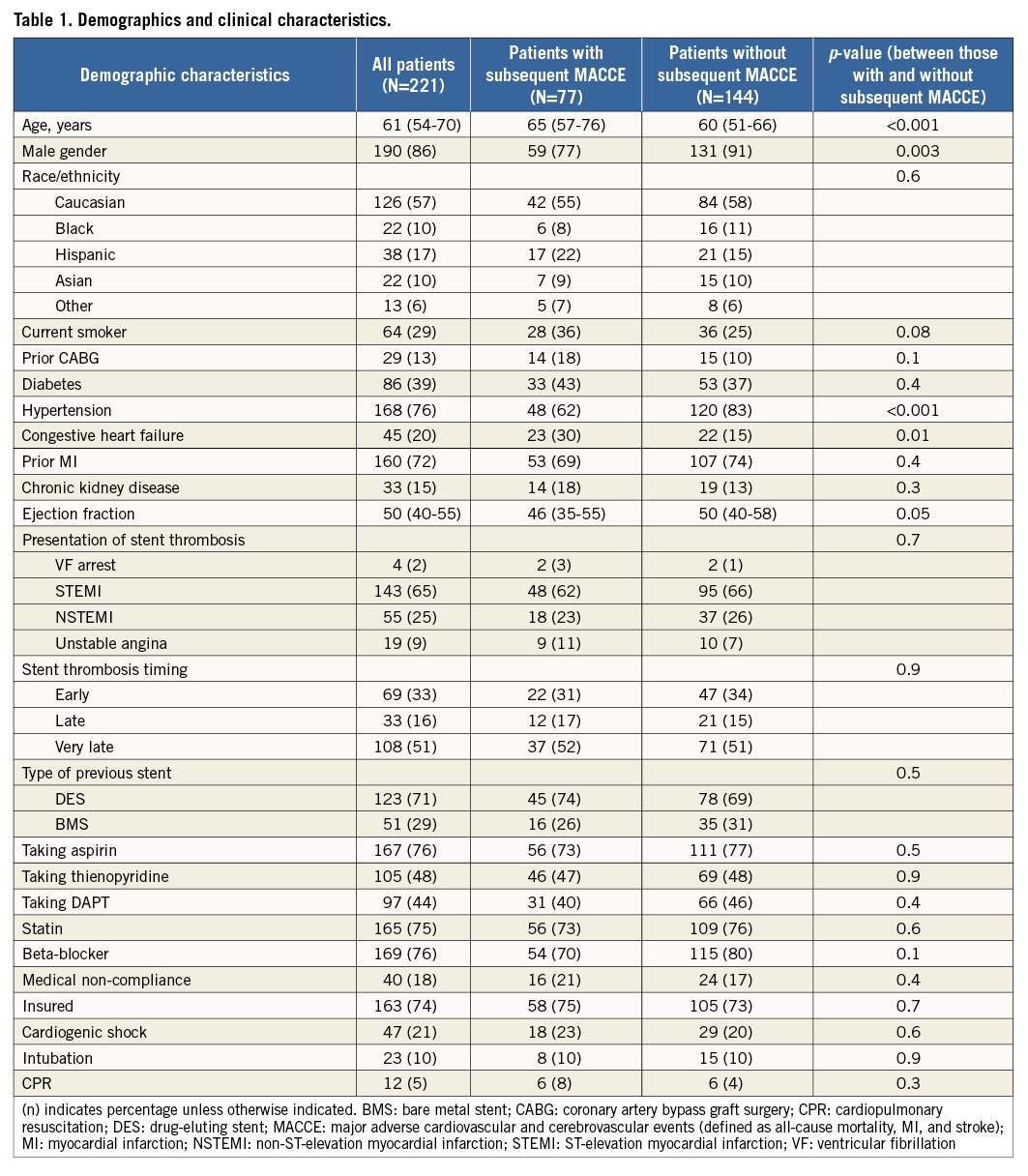
The in-hospital mortality was 5%. Table 4 shows the cumulative incidence of MACCE and its individual components over a five-year period. The median follow-up period was 3.7 years. MACCE rates were 22% at one year and up to 41% at five years. Of these, 13% of patients died by one year and 24% at five years. Definite or probable recurrent stent thrombosis rates were 15% and 23%, respectively.
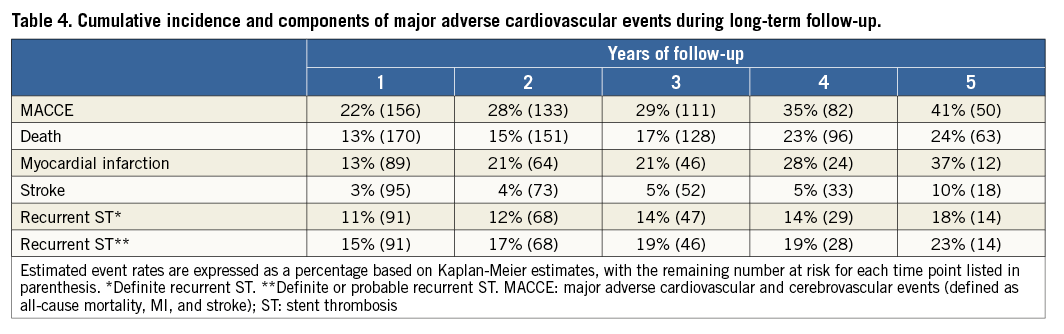
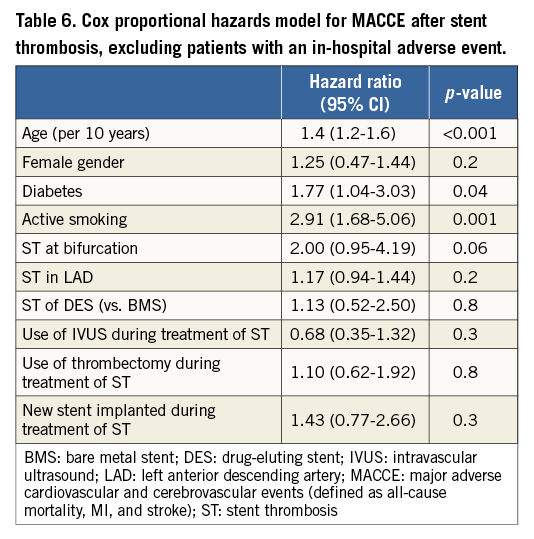
On multivariable analysis using a Cox proportional hazards model, age (per ten years, hazard ratio [HR] 1.5, 95% CI: 1.3-1.7), diabetes mellitus (HR 1.69, 95% CI: 1.04-2.74), active smoking (HR 2.44, 95% CI: 1.47-4.07), and stent thrombosis at a bifurcation (HR 2.67, 95% CI: 1.44-4.07) were independently associated with occurrence of MACCE up to five years from the index event (Table 5). The use of bare metal stents or drug-eluting stents was not independently associated with MACCE events. The timing of occurrence of the index stent thrombosis (i.e., acute, early, late and very late) was not associated with MACCE (Figure 1). Figure 2A and Figure 2B show the respective Kaplan-Meier curves for all-cause mortality and MACCE.
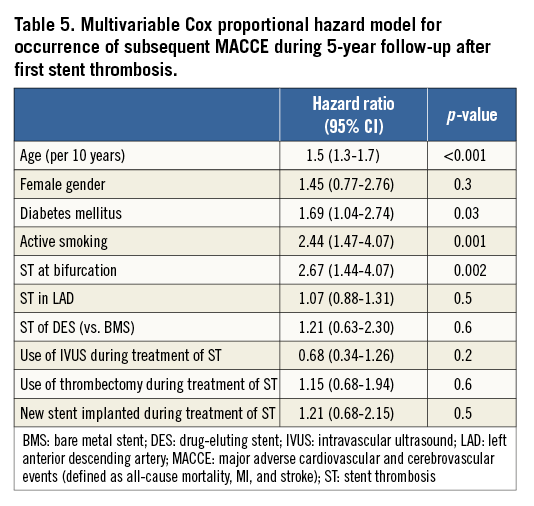
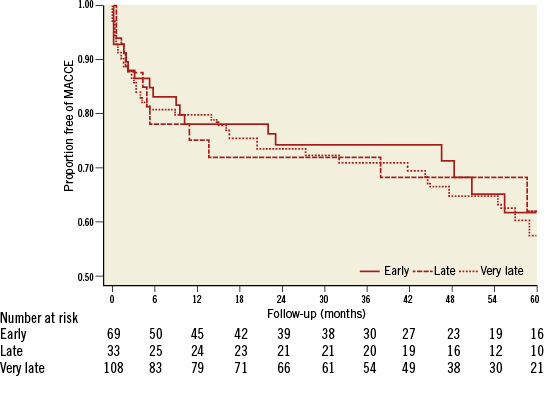
Figure 1. Kaplan-Meier curves showing MACCE events according to timing of stent thrombosis relative to index procedure.
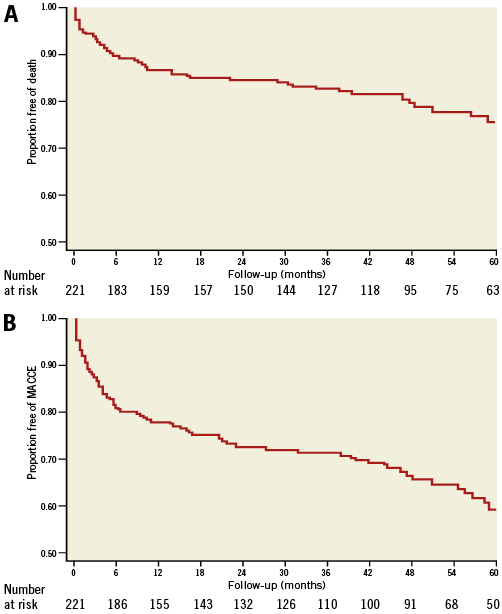
Figure 2. Kaplan-Meier curves showing all-cause mortality (A) and MACCE (B) over time.
Figure 3A and Figure 3B show the estimated hazard functions for all-cause mortality and MACCE over time. Plotting the hazard function over time revealed an early hazard of MACCE during the first two years, a relatively low hazard between two and four years, and a subsequent increased hazard of recurrent events after four years. In a sensitivity analysis excluding patients who had an in-hospital event during treatment of the initial stent thrombosis, the hazard ratios for predictors of long-term outcomes had similar point estimates when compared to the full model (Table 6).
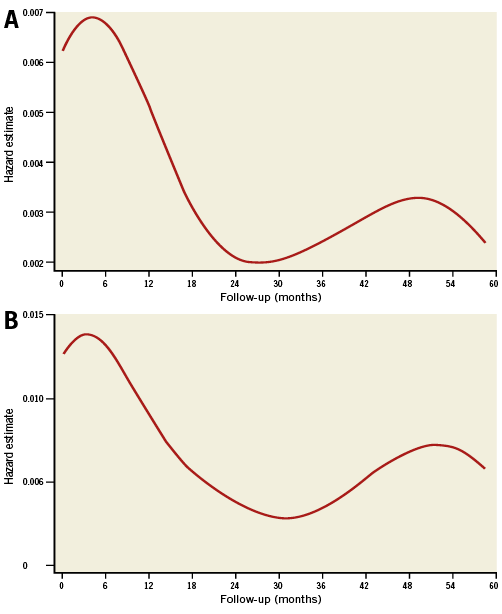
Figure 3. Estimates of hazard plots for all-cause mortality (A) and MACCE (B) over time.
Discussion
This study represents the longest follow-up available for the largest cohort of North American patients presenting with stent thrombosis. In this study of 239 stent thrombosis cases occurring in 221 patients, we showed that: 1) long-term event rates were elevated with 22% MACCE at one year and 41% at five years; 2) one-year mortality (including in-hospital mortality) in patients with ST who survive to coronary angiography is lower than previously reported; 3) definite or probable recurrent ST is not uncommon at 15% at one year and 23% at five years; 4) age, presence of diabetes mellitus, active smoking, and ST at a coronary bifurcation were associated with MACCE; and 5) there appears to be a bimodal temporal pattern associated with MACCE and mortality, with a possible late hazard of recurrent events years after the initial ST.
These findings provide an important perspective in relation to four other large studies on ST outcomes. Table 7 summarises the key findings of this study when compared with other large long-term series in the literature. Most importantly, long-term mortality rates were 15% and 24% at two and five years, respectively, consistent with these published reports: van Werkum reported two-year all-cause mortality of 12%3, while Kimura et al reported mortality ranging from 23.3% to 27.8%2. Almalla et al reported one-year and long-term (mean 65 months) mortality of 23.8% and 35.6%, respectively5. This is despite some differences in the study populations. For example, the study by van Werkum et al included 431 patients in Europe, of whom the vast majority had acute and subacute ST (73.6%), with only 13.2% very late ST3. Similarly, Almalla et al showed that, of the 117 cases in their series from Germany, 80.9% had early ST. Kimura’s paper from the Japanese RESTART registry similarly had a majority of early stent thrombosis (52.7%)2. In contrast to these studies, Armstrong et al showed, in a study of more than 7,000 ST cases from the ACC-NCDR registry, that the majority of ST cases were very late (60%)1 (NB: Armstrong’s study was not included in Table 7 as it only reported in-hospital outcomes). In our study, the majority of cases had very late ST (51%).
Recent trials of acute coronary syndrome (including STEMI) showed one-year mortality rates ranging from 3.5%-4.8% in the HORIZONS-AMI study7, 3.0-3.2% in the TRITON TIMI-38 study8, and 4.5-6.9% in the PLATO trial9. The high rates of late mortality in ST highlight the high-risk nature of ST, perhaps suggesting the deleterious effects of an acute coronary syndrome occurring on a background of pre-existing disease. In addition, it is concerning that there appears to be a second peak in the MACCE events occurring at approximately 48 months (Figure 3A, Figure 3B), giving a bimodal distribution to the occurrence of MACCE events, including mortality, after the index stent thrombosis. This is the first study to report such a finding and may represent the natural history of progressive atherosclerosis and CAD or a function of the sample size. Regardless of this, other investigators should examine their data for this possible late MACCE occurrence, and ongoing follow-up will be important to determine if the trend persists.
Consistent with other investigators, recurrent ST is not uncommon. In our series, 11% and 15% had a recurrent definite or definite/probable ST event, respectively, at one year. At five years, the rates were 18% and 23%, respectively. The reasons for recurrent ST remain unclear but could potentially include thienopyridine or aspirin non-responsiveness, chronic medication non-adherence or other undefined mechanical factors.
The proportion of patients on dual antiplatelet therapy at the time of initial presentation was 44% for the whole cohort and includes those who presented with very late ST. Of note, medication non-compliance was noted in only 18% of the study cohort. This registry included patients from 2005-2013 during which period the AHA and ACC recommended a minimum duration of one year with dual antiplatelet therapy in patients who received DES10. The proportion of those who received DES in our cohort exceeds 70%. This potentially longer duration of dual antiplatelet therapy may have influenced the timing of ST presentation in the present study. Regardless of this, our study shows that the concern regarding very late ST remains valid. Half of the study cohort presented with very late ST at a time when dual antiplatelet therapy was not mandated. These more recent studies were performed using second- and third-generation drug-eluting stents which are composed primarily of cobalt-chromium and other alloys, and use everolimus or zotarolimus instead of stainless steel and paclitaxel or sirolimus.
Although hypertension was less common in patients with MACCE, there is no obvious mechanistic connection between hypertension and stent thrombosis outcomes, unless an increased prevalence of hypertension is collinear with other characteristics. While we did include a description of this in the univariate analysis, hypertension was not a predictor of long-term outcomes on multivariable analysis, primarily because it was collinear with age and diabetes. On the other hand, our study showed that age, diabetes mellitus, active smoking and ST at a coronary bifurcation were independently associated with the occurrence of MACCE up to five years from the index event. In particular, active smoking was associated with an odds ratio of 2.44 while that of occurrence at a bifurcation was 2.67. We have previously reported that ST at a coronary bifurcation is associated with an increased risk of both short and long-term major adverse cardiovascular events11. As shown in these long-term data, these effects persist and perhaps represent the larger area of myocardium affected.
Limitations
This is a retrospective and observational study with its inherent limitations. These include the lack of uniform use of intravascular ultrasound, which could have provided important mechanistic information regarding mechanical causes for ST, including restenosis with superimposed thrombosis, stent malapposition and underexpansion12,13. Second, routine point-of-care testing for aspirin or thienopyridine hypo/non-responsiveness was not performed14-16. Third, the study design only included patients who presented to the cardiac catheterisation laboratory with definite ST. A significant proportion of patients with ST probably suffered sudden cardiac death and hence the study is only applicable to patients who survive to undergo angiography. Fourth, because patients had differential follow-up within the hospital systems, we were unable to determine accurately the duration of dual antiplatelet therapy after percutaneous coronary intervention for ST. This in turn may affect MACCE outcomes. In addition, given the retrospective nature of the study, long-term follow-up is unlikely to be complete. However, we have reported mortality using the SSDI, which would mitigate this limitation.
Conclusions
In this large multicentre California registry, the majority of patients with definite stent thrombosis and acute coronary syndromes presented with very late stent thrombosis. Long-term MACCE and mortality rates are significant at 41% and 24%, respectively. After multivariable analysis, only age, active smoking, diabetes mellitus and bifurcation disease were independently associated with MACCE. There also appears to be a late hazard risk for death and MACCE which will require further investigation.
| Impact on daily practice The majority of patients with definite stent thrombosis and acute coronary syndromes reported in this paper presented with very late stent thrombosis. Definite or probable recurrent stent thrombosis is not uncommon with rates of 15% at one year and 23% at five years. Long-term MACCE and mortality rates, at up to five years, are significant at 41% and 24%, respectively. After multivariable analysis, only age, active smoking, diabetes mellitus and bifurcation disease were independently associated with MACCE. There also appears to be a late hazard risk for death and MACCE which will require further investigation. |
Conflict of interest statement
K.K. Yeo has received research support from Medtronic and is on the speakers bureau for Abbott Vascular. R. Low is on the advisory board of Abbott Vascular and Boston Scientific. K. Shunk receives institutional research support from Abbott Vascular, Gilead, InfraRedx, and Siemens Medical Systems. E. Mahmud is on the speakers bureau for Medtronic and Eli Lilly, is a consultant for Eli Lilly, and has received research support from Boston Scientific, Abbott Vascular, Accumetrics and Sanofi Aventis. J. Rogers is a consultant for Volcano, Medtronic, and Boston Scientific. The other authors have no conflicts of interest to declare.