Stent thrombosis (ST) is rare but represents the most dramatic mechanism of coronary stent failure1. In view of the strong association with myocardial infarction (MI) and cardiac death, ST is the primary safety concern of coronary percutaneous coronary interventions (PCI) with stent implantation and represents the key endpoint for the evaluation of the safety profile of coronary stents2.
Evolution of PCI techniques, iterations of stent technologies, and optimisation of medical therapy have markedly reduced the risk of ST1,3. However, a considerable number of patients undergoing PCI with stent implantation still suffer from this life-threatening complication.
The pathophysiology of ST is multifactorial, with a number of possible triggers playing different roles over time after stenting4,5. Several studies have investigated potential mechanisms and predictors of ST, with the ultimate objective of providing informative data to prevent it6. Conversely, limited evidence is available on treatment strategies for patients suffering from ST and their long-term clinical outcomes.
In this issue of EuroIntervention, Tovar Forero and co-authors7 report the findings of a cohort of 695 patients suffering from ST at two large academic hospitals in Bern, Switzerland, and Rotterdam, the Netherlands, between 1996 and 2017. The study aimed to evaluate ST treatment strategies and their impact on outcomes.
The primary findings of this study underscore the terribly unfavourable outcomes of patients suffering from ST, with excessively high event rates during long-term follow-up. At five years, 25.8% of patients had died, 17.9% had had an MI, 24.8% had undergone a target vessel revascularisation, and 12.1% had had a repeat ST. The strongest independent predictors of major adverse cardiac events after ST were related primarily to an adverse clinical presentation of patients at the time of ST (i.e., cardiogenic shock, ST in the left anterior descending artery, and multivessel disease) or to a suboptimal procedural result at the time of the ST treatment (i.e., Thrombolysis In Myocardial Infarction [TIMI] flow <2). Unfortunately, while predictors are clearly identified by the study findings, the mechanisms underlying ST are not fully elucidated since only one out of four patients underwent intracoronary imaging. Among these, the key mechanisms are in line with previously available evidence (i.e., neoatherosclerosis, malapposition, and underexpansion)4,5.
In relation to treatment, approximately 60% of patients underwent repeat stenting and 34% underwent only balloon angioplasty. The latter was frequently used as the treatment strategy (47.9% of cases) in ST events occurring during the first 30 days after PCI, indicating the pivotal role of mechanical triggers of ST in the early phase and the subsequent need to optimise procedural results in these patients. The study also shows a large use of thrombectomy (in 47.9% of patients) and glycoprotein IIb/IIIa inhibitors (57.6% of patients) in the setting of ST, with no apparent benefit on long-term outcomes. The only effective treatment strategy appears to be the use of new-generation P2Y12 inhibitors, which are associated with a risk reduction for MI with borderline statistical significance as compared with clopidogrel (hazard ratio [HR] 0.56, 95% confidence interval [CI]: 0.32-0.99; p=0.049).
The authors should be commended for the exceptional work done in collecting such a granular description of ST cases over two decades. Overall, this study provides valuable findings for the scientific community and for clinical practice. The first and most relevant message is the prognostic relevance of ST. Since ST presents as an acute MI in the majority of cases, in order to put findings into perspective it is reasonable to compare event rates with those observed after primary PCI in patients with acute MI. In Figure 1, event rates observed by Tovar Forero and co-authors are compared with those observed in recent major trials on contemporary drug-eluting stents (DES) in patients with ST-segment elevation myocardial infarction (STEMI) at five-year follow-up, i.e., in the COMFORTABLE AMI8 and EXAMINATION9 trials. It is visually evident how ST is associated with a dramatic prognosis when compared with outcomes after STEMI. Interestingly, 51 out of 118 target vessel revascularisations (43.2%) observed by Tovar Forero and co-authors after a first ST were due to repeat ST. These findings underscore the second key message of the investigators’ experience, which is that currently available treatment for ST is largely ineffective. Future research should, therefore, focus on patients with ST with the aim of developing novel and effective treatment strategies for patients suffering from ST.
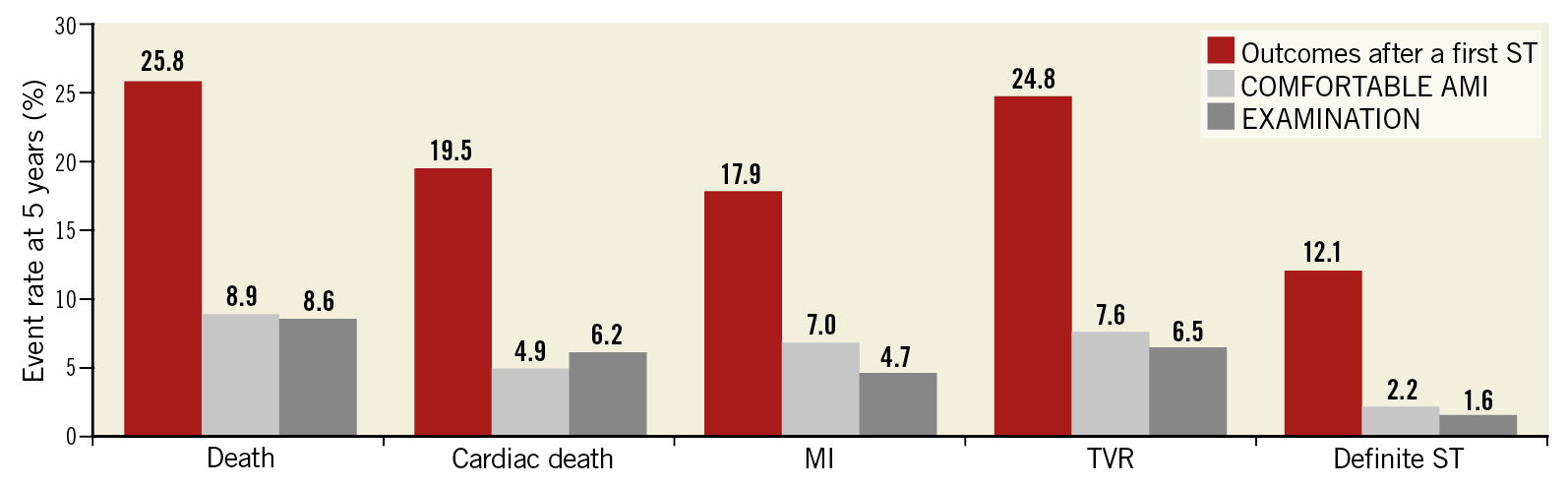
Figure 1. Five-year outcomes after a first ST versus outcomes after a STEMI in contemporary DES trials. Five-year clinical outcomes after a first ST in the Bern-Rotterdam experience as compared to outcomes after a STEMI in selected contemporary trials evaluating drug-eluting stents in patients with STEMI (COMFORTABLE AMI7 and EXAMINATION8 trials). DES: drug-eluting stent; MI: myocardial infarction; ST: stent thrombosis; STEMI: ST-segment elevation myocardial infarction
In summary, the unfortunate victims of ST have limited treatment options and a dramatic long-term prognosis. At this point in time, all efforts should be implemented to prevent ST by optimising procedural outcomes, tailoring antithrombotic therapy to patients’ risk profiles, and intensifying secondary prevention since, in the absence of an effective cure, prevention remains the only effective strategy.
Conflict of interest statement
G.G. Stefanini reports research support (to the institution) from Boston Scientific, and speaker fees from B. Braun, Biosensors, and Boston Scientific. The other author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.