Introduction
Endovascular therapy (EVT) for chronic total occlusion (CTO) in peripheral arteries is technically challenging. The success rate of antegrade approaches is significantly diminished when the ostium (the entry point) of the occluded vessel is ambiguous or cannot be well visualised1. In the present study, we attempted direct visualisation of the CTO ostium and wire manipulation by angioscopy-guided EVT under continuous infusion of saline (AGECIS). We have already demonstrated the role of angioscopy as a diagnostic tool in EVT2; however, few reports have shown the utility of angioscopy as a therapeutic guiding tool. Here we demonstrate the efficacy and safety of AGECIS in peripheral arteries and the impact of angioscopy as a therapeutic guiding tool.
Methods
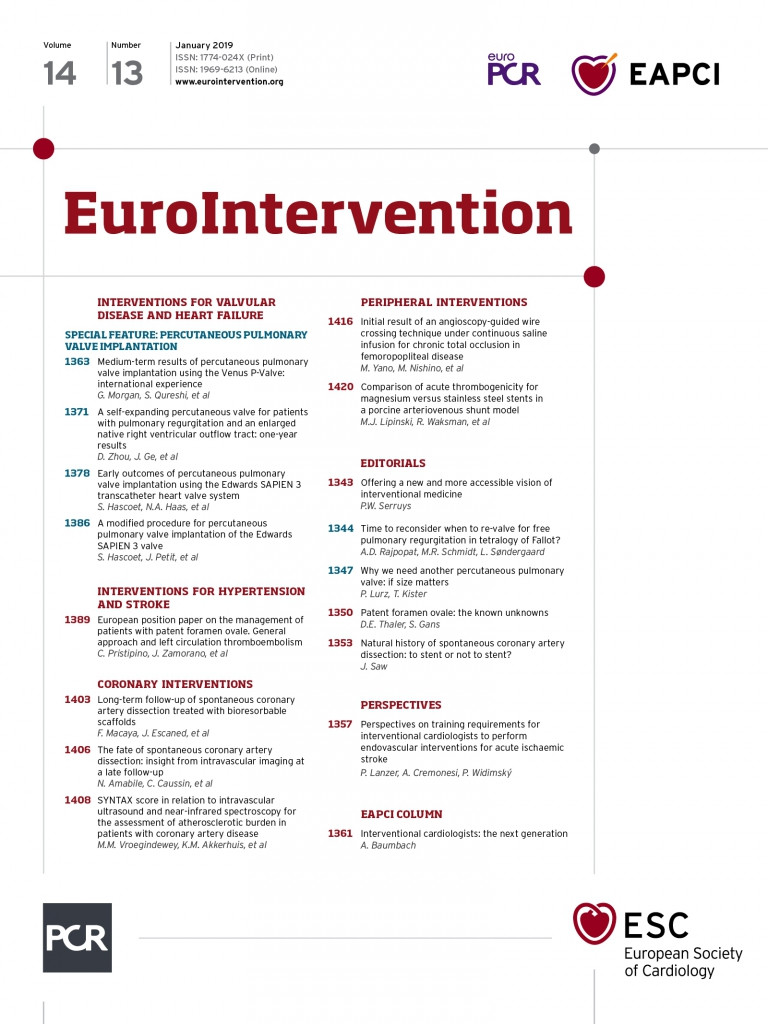
We enrolled 13 patients with CTO or severe stenosis (99% stenosis) in the femoropopliteal area. A 6 Fr guide catheter was inserted into the superficial femoral artery or popliteal artery via the antegrade approach and deployed close to the lesions. We tried to pass a guidewire into the lesion under angioscopic guidance. We used blood flow preserved angioscopy (Visible; FiberTech, Chiba, Japan) in which direct visualisation is commonly achieved only by a manual flush injection of saline from the Y-connector through a 4 Fr guiding catheter for an angioscopy (probing catheter). In AGECIS, our novel technique, we used the usual manual flush injection of saline from the Y-connector combined with a continuous infusion of saline from the pressurised bag into the sheath flush lumen to remove the blood flow in front of the ostium of the lesion completely and continuously (Figure 1A). With direct visualisation of the wire manipulation, we tried to insert the wire into possible entry points in the CTO, which frequently showed dimples or small holes (Figure 1B, Moving image 1, and case 11 in Supplementary Table 1). After wire crossing was achieved, we performed intravascular ultrasonography (IVUS) and evaluated whether the wire had entered into the true lumen or not (Figure 1B, Figure 1C, Moving image 1, Moving image 2, and cases 11 and 9 in Supplementary Table 1, respectively). In addition, we analysed clinical and procedural characteristics in a matched control group of patients who underwent EVT for femoropopliteal CTO during the same period without AGECIS. All study patients gave written informed consent for the procedure which was approved by the institutional review board of Osaka Rosai Hospital.
Figure 1. Angioscopy-guided endovascular therapy under continuous infusion of saline (AGECIS) system and representative angioscopy/IVUS imaging in true lumen and subintima. A) Saline infusion from the pressurised bag into the sheath flush lumen (white arrow). The AGECIS system usually uses a manual flush injection of saline from a Y-connector combined with continuous infusion of saline from the pressurised bag into the sheath flush lumen to visualise a clear front view of the lesion and the wire. B) & C) Angioscopy and intravascular ultrasound (IVUS) views of the guidewire crossing into the lesions. B) Case 11: angioscopy showed accurate wire crossing into the ostial site of the true lumen in chronic total occlusion (CTO). Angioscopy also demonstrated moderate calcified plaque around the CTO ostium. IVUS demonstrated that the guidewire was in the CTO true lumen. C) Case 9: angioscopy showed that the guidewire was inserted into the subintima of the CTO lesion. IVUS also demonstrated that the guidewire was inserted into the subintima of the CTO lesion.
Results
The clinical and lesion characteristics of the AGECIS and control groups are listed in Supplementary Table 1. We performed AGECIS in 13 patients with no complications. The characteristics of the procedure are shown in Supplementary Table 2. We could obtain direct visualisation of the lesion ostium by AGECIS in 11 lesions (84.6%), but in two cases (severe stenotic lesions) direct visualisation could not be obtained. We could not accurately insert the wire into the true lumen in only one CTO patient among all of the patients in whom AGECIS was able to visualise the ostium of the lesions. Moreover, we were able to confirm the lesion characteristics such as thrombus and severe calcification by AGECIS (case 3 and case 13). The average procedure time and total amount of contrast medium in the AGECIS group and in the control group (10 patients) was 266.5±96.9 min, 129.2±72.0 ml and 324.0±130.5 min, 154.0±47.9 ml, respectively (Supplementary Table 1).
Discussion and limitations
We focused on angioscopy as an imaging guide to achieve wire crossing into the CTO ostium and demonstrated that AGECIS for CTO was safe and useful. However, we could not observe the CTO ostium using angioscopy in two cases (Figure 2A, Figure 2B, Supplementary Table 1) because large discrepancies caused good antegrade blood flow and the blood could not be washed out by the saline injected from the sheath flush lumen; as a result, we could not obtain direct visualisation of the lesion ostium. Therefore, AGECIS is suitable for lesions in which the vessel and sheath dimensions are similar. We believe that AGECIS has many advantages. It provides information on the actual points of entry into the true lumen or subintima. AGECIS involves lower radiation exposure for the patient and requires a smaller amount of contrast medium because the operators can perform the wire crossing technique while watching via angioscopy (Supplementary Table 1). Moreover, angioscopy in the peripheral arteries provides some pathological findings of peripheral artery lesions such as a large calcified plaque in the CTO ostium (case 13, Figure 2C, Moving image 3) or a white thrombus (case 3, Figure 2D, Moving image 4). In case 13, the antegrade approach will be difficult and the guidewire crossing can instead be performed by the retrograde approach. In case 3, aspiration of the thrombus and distal protection might be effective. In this way, our novel method, AGECIS, not only provides imaging of real-time guidewire crossing into the CTO ostium using information of vessel anatomy and pathology but can also help in the selection of a therapeutic method. A major limitation of this study is the small number of patients. More cases performed using angioscopy-guided EVT are needed to ascertain the value of our study.
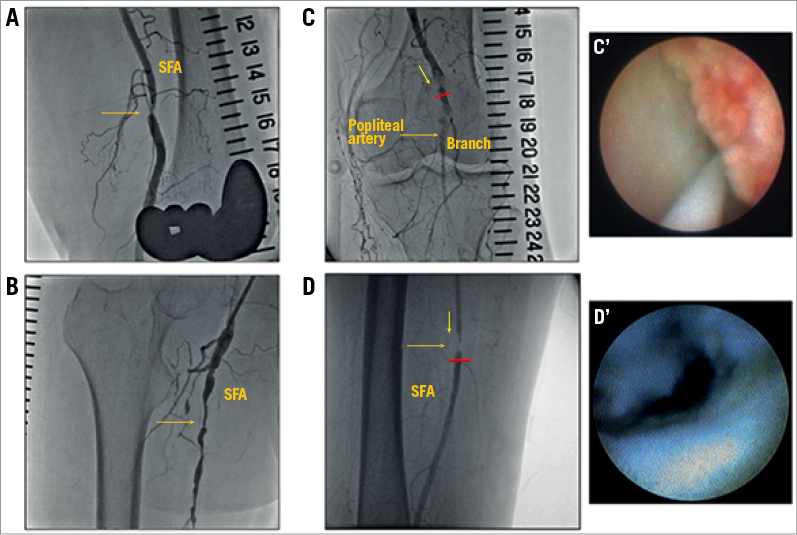
Figure 2. Representative cases with CTO and severely stenotic lesions. A) & B) In these two cases (cases 4 and 7) with severely stenotic lesions in the superficial femoral artery, we could not observe the lesion ostium using AGECIS. C, C’) Case 13 showing a large calcified plaque in the CTO ostium of the curved vessel. C) The CTO lesion of the popliteal artery in angiography. The filling defect that presented in the CTO lesion distal to the popliteal artery flow was enhanced by collateral flow. C’) Angioscopic view of the branch vessel bifurcation (red arrow in panel C). A large calcified plaque occluded the ostial site of the popliteal artery. The guidewire was inserted into the branch vessel of the popliteal artery. Based on these findings, we decided to switch from the antegrade approach to the retrograde approach. D, D’) Case 3 showing a white thrombus around the lesion. D) Severely stenotic lesion of the superficial femoral artery on angiography. D’) Angioscopic view of severely stenotic lesion in the superficial femoral artery. The white thrombus was confirmed around the severely stenotic lesion.
Conclusion
Angioscopy-guided EVT under continuous infusion of saline (AGECIS) is safe and useful. AGECIS allows accurate wire crossing into the true lumen of a lesion, provides anatomical and pathological information on lesions and leads to the use of optimal therapeutic methods. This novel technique may increase the success rate of the treatment of CTO in peripheral arteries.
| Impact on daily practice Angioscopy-guided endovascular therapy under continuous infusion of saline (AGECIS) could directly visualise wire crossing into the ostial sites of culprit lesions during endovascular therapy (EVT). AGECIS is safe (no complications) and useful (success rate 90.9%). This novel technique may increase the success rate of EVT for CTO in femoropopliteal disease. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1. Clinical and lesion characteristics.
Supplementary Table 2. Procedure characteristics.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Case 11.
Moving image 2. Case 9.
Moving image 3. Case 13.
Moving image 4. Case 3.