Abstract
Aims: We aimed to analyse the impact of pulmonary hypertension (PH) on the in-hospital outcome of either surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR).
Methods and results: Data from all 107,057 patients undergoing isolated SAVR or TAVR in Germany between 2007 and 2014 were provided by the German Federal Bureau of Statistics. About 18% of patients with aortic valve stenosis suffered from PH. Patients with PH had more comorbidities with consequently increased EuroSCORE (TAVR without PH: 12.3%; with PH: 24%). The presence of PH led to an increase of in-hospital strokes, bleedings, acute kidney injuries, and pacemaker implantations in both treatment groups (TAVR and SAVR), but the PH-associated increase of complications and mortality was less pronounced among patients receiving TAVR (mortality after TAVR without PH: 5.4%; with PH: 7.2%). After baseline risk adjustment, the TAVR procedure was associated with a reduced risk of in-hospital stroke (OR 0.81, p=0.011), bleeding (OR 0.22, p<0.001), and mortality (OR 0.70, p=0.005) among PH patients, and in comparison to surgical treatment.
Conclusions: PH is a risk factor for worse outcome of SAVR and TAVR. This fact is less pronounced among TAVR patients. Our data suggest a shift towards the transcatheter approach in patients suffering from PH.
Abbreviations
AVR: aortic valve replacement
CABG: coronary artery bypass graft
CAD: coronary artery disease
COPD: chronic obstructive pulmonary disease
GFR: glomerular filtration rate
NYHA: New York Heart Association
PH: pulmonary hypertension
PPI: permanent pacemaker implantation
SAVR: surgical aortic valve replacement
TAVR: transcatheter aortic valve replacement
Introduction
Various risk factors impair the success of and increase mortality in aortic valve replacement (AVR). Patients with severe aortic valve stenosis display a high prevalence of pulmonary hypertension (PH)1. The causes of PH are manifold: pulmonary hypertension may occur due to an underlying pathology of the heart, the lungs, accompanying concomitant rheumatic disorders, following chronic and recurrent pulmonary embolism, or may be idiopathic or congenital.
Several previous studies have identified PH as a risk factor for long-term survival and postoperative complications in patients undergoing SAVR or TAVR2-4. In patients treated with TAVR, PH limits 30-day mortality along with other factors such as NYHA Class IV heart failure, age >90 years, and active dialysis5,6. Therefore, the perioperative risk tools such as the Society of Thoracic Surgeons (STS) score and the EuroSCORE have included PH as a variable predicting outcome after aortic AVR.
Since the first transcatheter AVR (TAVR) in 2002, this procedure has been increasingly performed and established as the standard of care for high-risk patients with severe aortic valve stenosis6. Several clinical trials have confirmed the value of TAVR as an important therapeutic option for high- and even intermediate-risk patients with severe aortic valve stenosis7. Therefore, guidelines recommend the use of TAVR in high-risk patients8.
The aim of the present study was to determine how PH affects typical and frequent complications, in-hospital course, and the actual mortality rate in large cohorts after TAVR or SAVR9.
Methods
STUDY DESIGN
All isolated SAVR or TAVR in Germany since the launch of TAVR in 2007 were identified by query to the German Institute for Medical Documentation and Information (Deutsches Institut für Medizinische Dokumentation und Information; Cologne, Germany). Baseline characteristics, in-hospital course, and outcome were determined by identification of corresponding diagnosis-related group (DRG) and international classification of diseases (ICD) codes.
DATA ACQUISITION
Only patients with aortic stenosis were included in the analysis (ICD codes I35.0/I06.0). As described previously6, we were able to use the Operationen- und Prozedurenschlüssel (OPS) codes (OPS codes: 5-35a.0 in 2007 and 5-35a.00, 5-35a.01 from 2008) to identify all cases of isolated surgical and transcatheter AVR relevant for our analysis. Redo procedures (previous cardiac surgery or previous CABG) are defined by the codes Z95.1-4. Combined interventions were excluded. Regarding the in-hospital complications, bleeding was defined as requiring more than five units of red blood cells (RBC) for admission (OPS codes 8-800.7* et seqq., since 2010 8-800.c et seqq.). Acute kidney injury was defined by the ICD code 17.* and need for pacemaker implantation by the OPS code 5-377.0 et seqq. The ICD code I27* defined PH, which includes primary and secondary pulmonary hypertension.
CALCULATION OF THE LOGISTIC EUROSCORE
The EuroSCORE was calculated using the ICD codes for chronic obstructive pulmonary disease (COPD) (J43*, J44*), for neurological dysfunction (I69*, G81*, R48*), previous cardiac surgery (Z95.1-Z95.4), creatinine (N18.0, N18.84; since 2010, N18.4, N18.5), active endocarditis (I33*), unstable angina (I20.0), recent myocardial infarction (I25.20), and PH (I27*). Age, sex, and admission status “emergency” were included. Data about preoperative state and left ventricular function were not available and assumed as an inconspicuous state. In order to allow a direct comparison of the baseline risk factor composition, we calculated logistic EuroSCORE values assuming isolated AVR procedures for both TAVR and SAVR patients.
STATISTICAL ANALYSIS
As the first step, a data set was generated based on SAS codes (SAS, Version 9.2; SAS Institute Inc, Cary, NC, USA) supplied to the Research Data Centers of the Federal Bureau of Statistics (Statistisches Bundesamt, DESTATIS) by the authors. Next, this data set was transformed into Stata format (StataCorp, College Station, TX, USA). Differences between groups were calculated using the chi-square test for categorical variables and the Student’s t-test for continuous variables. In order to analyse the impact of PH on stroke, bleeding, and in-hospital mortality in patients treated with SAVR or TAVR, we used a three-step procedure. First, the impact of PH on stroke, bleeding, and in-hospital mortality was analysed using logistic regression. Second, we adjusted in-hospital outcomes for EuroSCORE. As described before, the EuroSCORE was calculated identically for surgical and transcatheter approaches in order to allow the direct comparison of EuroSCORE values between TAVR and SAVR patients. Finally, a fully adjusted regression model was conducted including all comorbidities as potential confounders. Again, logistic regression analyses were applied. All analyses were carried out using Stata 14 (StataCorp).
Results
PATIENTS UNDER 80 WITH PH WERE FREQUENTLY ASSIGNED TO TAVR
In Germany, between 2007 and 2014, 107,057 patients underwent isolated surgical or transcatheter AVR; 18% of these patients were diagnosed with PH. The prevalence of PH was higher in patients receiving TAVR (11.5% receiving SAVR, 28.7% in patients receiving TAVR). The number of TAVR procedures increased in patients with and without PH from the launch of TAVR in 2007 to 2014. In contrast, the number of SAVR procedures declined by 20% (2007: 8,622; 2014: 6,922 procedures) in patients with PH, but overall was stable in patients without PH in the group of patients under the age of 80 years. Patients between 75 and 80 years without PH were mostly assigned to SAVR. However, if a PH was present in this age group, patients were more often treated by TAVR (Figure 1).
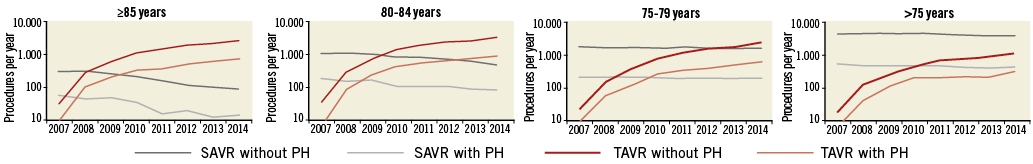
Figure 1. Procedural numbers of SAVR and TAVR from 2007 to 2014 with and without PH. Given are all surgical (grey) and transcatheter (red) aortic valve replacements without (dark grey/red colour) or with (light grey/red colour) PH in different age groups performed per year in Germany.
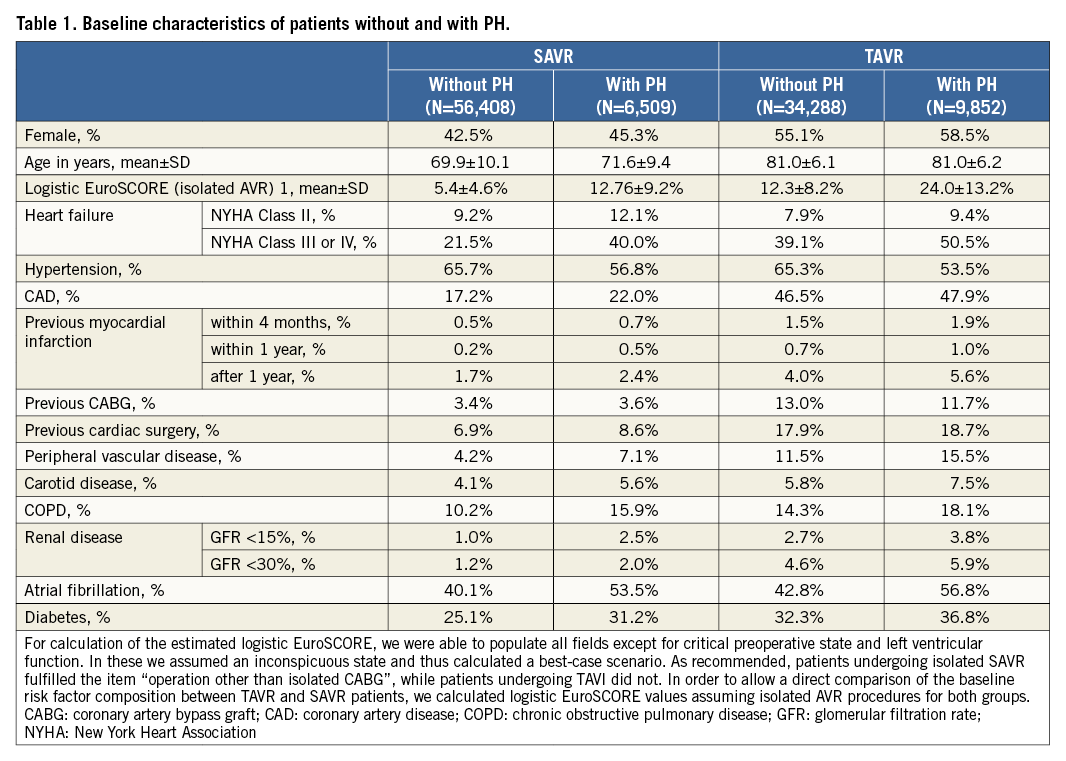
PATIENTS WITH PH DISPLAYED MORE COMORBIDITIES
In both groups, patients with PH were more likely to be women and to suffer from more comorbidities such as COPD, peripheral arterial disease, atrial fibrillation, and renal disease. The age was similar. As expected, patients with PH were more often in NYHA Class III or IV, accounting for nearly 50% of patients with PH receiving TAVR.
Overall, patients receiving SAVR were younger, had a lower calculated operative risk, and displayed fewer comorbidities compared to patients assigned for TAVR. Consequently, patients with PH treated with TAVR were at the highest operative risk as assessed by the EuroSCORE (SAVR without PH: 5.4%, with PH: 12.8%; TAVR without PH: 12.3%, with PH: 24.0%) (Table 1).
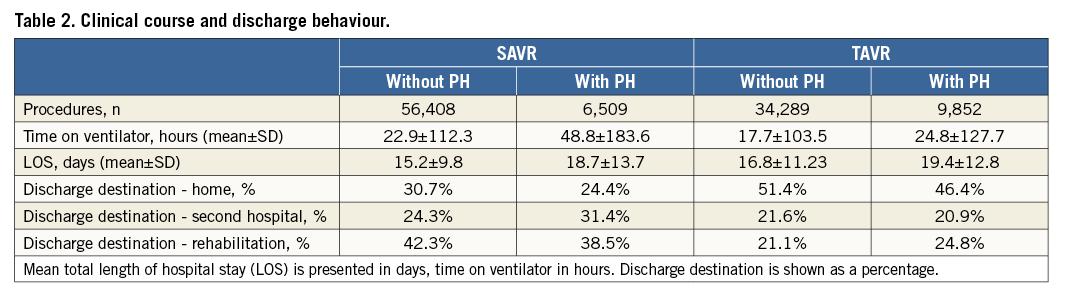
PATIENTS WITH PH SHOWED A WORSE IN-HOSPITAL COURSE
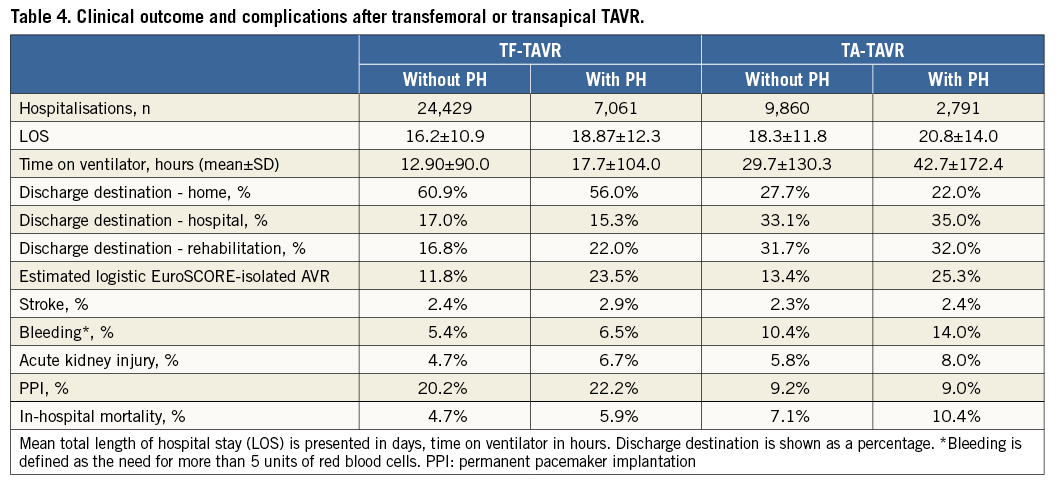
The presence of PH prolonged the time on a ventilator to 49±184 hrs in patients with PH receiving SAVR from 23±112 hrs in those without PH. In patients treated with TAVR, the time on the ventilator increased from 18±104 hrs without PH to 25±128 hrs with PH. Thus, the length of hospital stay was longer in patients with PH (SAVR without/with PH: 15.2±9.8/18.7±13.7 days; p<0.001; TAVR without/with PH: 16.8±11.23/19.4±12.8 days; p<0.001). Furthermore, only one quarter of patients with PH receiving SAVR were discharged home compared to 31% of patients without PH. In particular, transfer to a second hospital was more frequent in patients with PH receiving SAVR. In the TAVR collective, nearly 50% of patients receiving TAVR without PH were discharged home. This percentage decreased to 46% when PH was present. However, PH did not increase the necessity for a transfer to a second hospital in the TAVR group (22% without PH vs. 21% with PH; p=0.150), but led to more discharges to rehabilitation (21% without PH vs. 25% with PH, p=0.002) (Table 2).
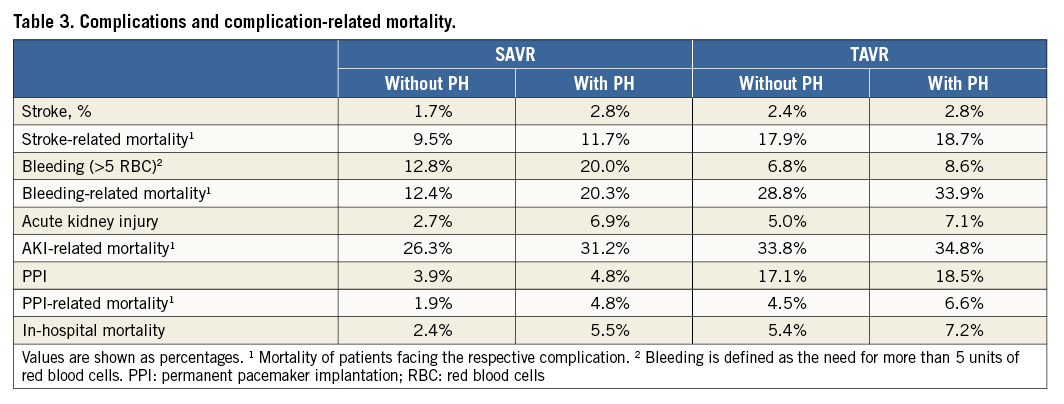
COMPLICATIONS INCREASED IN PATIENTS WITH PH
The rate of post-procedural stroke increased from 1.7% in patients without PH to 2.8% in patients with PH after SAVR (p<0.001). The increase in the number of strokes was less in patients receiving TAVR (2.4% without PH, 2.8% with PH, p=0.140). Furthermore, the need for blood transfusion was 1.6 times higher and acute kidney injuries were 2.6 times higher in patients with PH compared to patients without PH receiving SAVR (both p<0.001). However, the relative increase of complications was less pronounced in patients receiving TAVR: the need for red blood cell transfusion increased by 1.3 times and the rate of acute kidney injuries by 1.4 times in patients with PH compared to patients without PH (both p<0.001). Permanent pacemaker implantations were slightly higher in patients with PH in both groups (Table 3).
PH PATIENTS SHOWED INCREASED OPERATIVE RISK AND IN-HOSPITAL MORTALITY
Operative risk estimation as assessed by the EuroSCORE rose from 5.4% in patients without PH to 12.8% in patients with PH treated with SAVR (p<0.001). The EuroSCORE of patients receiving TAVR was 12.3% in patients without PH and 24.0% in patients with PH (p<0.001).
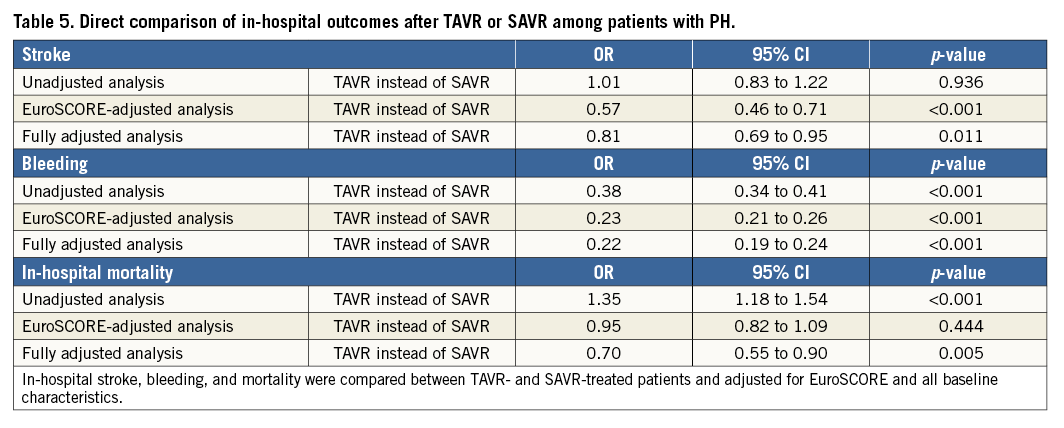
The actual in-hospital mortality was twice as high in patients with PH receiving SAVR (without PH: 2.4%, with PH: 5.5%, p<0.001). In-hospital mortality in TAVR-treated patients was higher overall (reflecting the higher morbidity of this collective), but rose only slightly in patients suffering from PH (without PH: 5.4%, with PH: 7.2%, p<0.001) (Figure 2). Among patients treated with TAVR, a transapical approach was associated with increased in-hospital mortality (Table 4). Due to the differences in baseline characteristics, a direct comparison between the surgical and transcatheter collectives is difficult and should be interpreted with caution. Patients suffering from PH treated with TAVR were at reduced risk for in-hospital stroke, bleeding, and mortality after adjustment for EuroSCORE and all baseline characteristics compared to patients treated with SAVR (after full adjustment - risk for stroke: OR 0.81, p=0.011; risk for bleeding OR 0.22, p<0.001; risk for mortality OR 0.70, p=0.005) (Table 5).
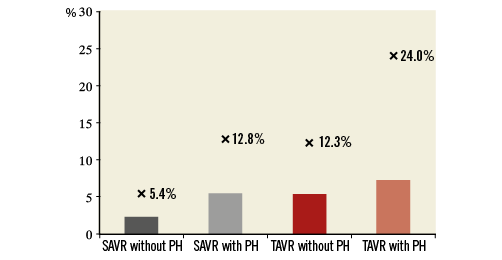
Figure 2. EuroSCORE and in-hospital mortality. In-hospital mortality of surgical (grey) and transcatheter (red) aortic valve replacement without (dark grey/red) or with (light grey/red) PH is shown as bars and percentage. The corresponding estimated EuroSCORE is marked as “x” for each group. The logistic EuroSCORE was calculated. Data about preoperative state and left ventricular function were not available and assumed as an inconspicuous state.
Discussion
TAVR is an evolving treatment strategy for degenerative aortic valve stenosis that has seen widespread adoption over the past decade6,10. However, patients undergoing TAVR show various inhomogeneities in terms of comorbidities11. Here, we analysed prevalence, patient characteristics, and outcomes of patients with PH undergoing AVR in the German healthcare system between 2007 and 2014.
We found a PH prevalence of 18% in all patients treated for aortic valve stenosis between 2007 and 2014, which is in line with data from a general population12. Despite a similar age, patients with PH suffered from more comorbidities affecting outcome post SAVR and TAVR, which probably accounts for the elevated NYHA class observed in patients with PH. The fact that nearly half of the patients with PH were in NYHA Class III or IV illustrates how highly symptomatic these patients are, warranting urgent treatment in most cases. However, due to the high prevalence of comorbidities, patients with PH and the consequently high operative risk estimation as predicted by the EuroSCORE are unfavourable candidates for SAVR.
The EuroSCORE was calculated as highest in patients receiving TAVR with PH. Therefore, it is not surprising that TAVR procedures increased in patients with PH in all age groups. In contrast, in the age group between 75 and 79 years without PH, numbers of SAVR and TAVR were similar in 2013, whilst patients with PH were more frequently assigned to TAVR in this age group. These data clearly indicate a shift towards TAVR in these patients.
PH is a risk factor for extubation failure after cardiac surgery13. Accordingly, patients with PH were ventilated for a longer time compared to patients without PH after SAVR. These data indicate a complicated postoperative course in patients with PH. Beyond that, prolonged ventilation represents a risk factor for further complications such as ventilator-associated pneumonia or need for long-time ventilation14. Whereas patients with PH after SAVR stayed on a ventilator more than twice as long, patients with PH after TAVR were ventilated 1.3 times longer compared to respective controls without PH. Accordingly, length of hospital stay was prolonged in patients with PH in both groups. However, the majority of patients with PH receiving TAVR could be discharged home or to rehabilitation, indicating a fast recovery after the procedure irrespective of PH. This is in line with previous work which showed that patients after TAVR recover faster15.
The procedure-associated complications and the complication-related mortality increased if patients suffered from PH. Strokes, relevant bleedings, acute kidney injuries, and need for pacemaker implantation increased strongly in patients with PH receiving SAVR. This was also the case in patients treated with TAVR, but the increase was less pronounced. The associated comorbidities might have contributed to the rise in procedural complications. Peripheral vascular disease and atrial fibrillation are also found more frequently in patients with PH and may directly contribute to the increased incidence of bleeding observed in these patients16. The higher rates of carotid disease may be causally involved in the documented higher stroke rates17. A relevant renal disease is also found more often in patients with PH and could, at least partially, explain the increased rates of acute renal failure in PH patients.
Mortality is more than twice as high after SAVR in patients with PH compared to patients without PH. Due to the higher EuroSCORE and different baseline characteristics, a direct comparison of mortality is difficult and should be made with caution. However, after full adjustment, PH patients treated with TAVR were at lower risk for stroke, bleeding, and in-hospital mortality compared to patients treated with SAVR. Furthermore, the in-hospital mortality of patients with PH receiving TAVR increased only slightly, demonstrating that patients with PH can be treated safely with TAVR, although a slight increase of in-hospital complications and mortality was also observed in TAVR-treated patients. These data are in line with a previous meta-analysis including data from over 9,000 individuals, which found increased rates of stroke and mortality in patients with PH after TAVR4.
Study limitations
The present analysis is retrospective for the in-hospital course between 2007 and 2014 in Germany; midterm and long-term outcome cannot be determined. Therefore, the results of the most recent transcatheter aortic valve systems are underreported in the present analysis. Administrative data assure a high quality and completeness, since this coding is crucial for health economics. However, we cannot exclude that the prevalence of PH may have been underreported or overreported in our study due to encoding errors. Furthermore, PH definition is based on the ICD code; therefore, stratifying the severity or classification of PH is not possible. Moreover, we cannot provide data as to whether PH was diagnosed by using right heart catheterisation or solely estimated by echocardiography. However, echocardiographic estimation and invasive measurement are known to predict outcome after TAVR3.
A comparison between surgical and transcatheter-treated patients is difficult, since the baseline characteristics of both groups are very different and individual decisions are not traceable. Nevertheless, we present a large data set with clinical outcomes of over 100,000 patients, which is highly relevant and may be useful in estimating achievable outcomes for patients.
Conclusions
In conclusion, our data corroborate the role of PH as a powerful risk factor for worsened outcome after AVR. Our data suggest TAVR as a preferred and safe option in patients suffering from PH.
| Impact on daily practice In-hospital outcome is worse for patients with PH receiving SAVR or TAVR compared to those without. Therefore, the approach to AVR should be considered carefully in patients with TAVR. TAVR is an option for these patients, since the increase of complications is less pronounced in patients receiving TAVR compared to those receiving SAVR. |
Acknowledgements
We wish to thank Angelika Gerlach and Marion Rüdiger for their excellent assistance in data acquisition.
Funding
The study was supported by internal funding from the University Heart Center Freiburg.
Conflict of interest statement
J. Reinöhl works as proctor for Edwards Lifesciences and Direct Flow Medical. The other authors have no conflicts of interest to declare.