Abstract
Aims: The aim of this study was to assess silent and clinically apparent cerebral embolic events in patients undergoing transcatheter left atrial appendage closure.
Methods and results: In this prospective single-centre study, 28 patients underwent percutaneous closure of the left atrial appendage. In all patients, a diffusion-weighted magnetic resonance imaging (DW-MRI) study was performed before, the day after the procedure, and during routine follow-up after 45 days. All patients underwent neurological assessment at the time of DW-MRI. Additionally, transcranial Doppler ultrasound monitoring (TCD) for the detection of microembolic material during the procedure was performed. The procedure was successfully completed in all patients. New embolic lesions were detected in nine patients (32%) after the procedure, of which three (33%) were detectable as gliotic lesions at follow-up. One (3.6%) new lesion was observed at 45-day follow-up. Neurological assessment showed no neurological deficits. We observed no relationship between the numbers of microembolic signals on TCD monitoring and the occurrence of cerebral infarctions on DW-MRI.
Conclusions: New cerebral embolic events occur after transcatheter closure of the left atrial appendage. However, most of the lesions demonstrate no gliotic transformation at follow-up. In all patients, the cerebral lesions were clinically unapparent.
Abbreviations
DW-MRI: diffusion-weighted magnetic resonance imaging
FLAIR: fluid attenuated inversion recovery
LAA: left atrial appendage
MoCA: Montreal cognitive assessment
NIHSS: National Institutes of Health Stroke Scale
TCD: transcranial Doppler
TEE: transoesophageal echocardiography
Introduction
Transcatheter closure of the left atrial appendage (LAA) for stroke prevention in patients with atrial fibrillation has been developed as an alternative to systemic anticoagulation in patients with atrial fibrillation1.
Since the first reports of transcatheter closure of the LAA in 2002, several devices have been designed specifically for occlusion of the LAA1-4. The WATCHMAN® (Boston Scientific, Marlborough, MA, USA) closure device was compared to standard treatment with chronic warfarin therapy in two prospective randomised, controlled trials. In these trials the WATCHMAN device was non-inferior to warfarin3,5.
In recent years, multiple studies have shown that left heart procedures are associated with an increased occurrence of silent cerebral embolism6. Although the rate of clinically apparent cerebral events after transcatheter closure of the LAA is low (0.1-1.9%), due to the nature of the LAA closure procedure there might be a significant number of unapparent cerebrovascular events3,5,7. In the present prospective study, we examined the frequency and clinical implications of embolic cerebral lesions by using diffusion-weighted magnetic resonance imaging (DW-MRI) following transcatheter closure of the left atrial appendage. Additionally, we tried to correlate cerebral embolism with peri-interventional microembolic signals from transcranial Doppler (TCD) ultrasound monitoring.
Methods
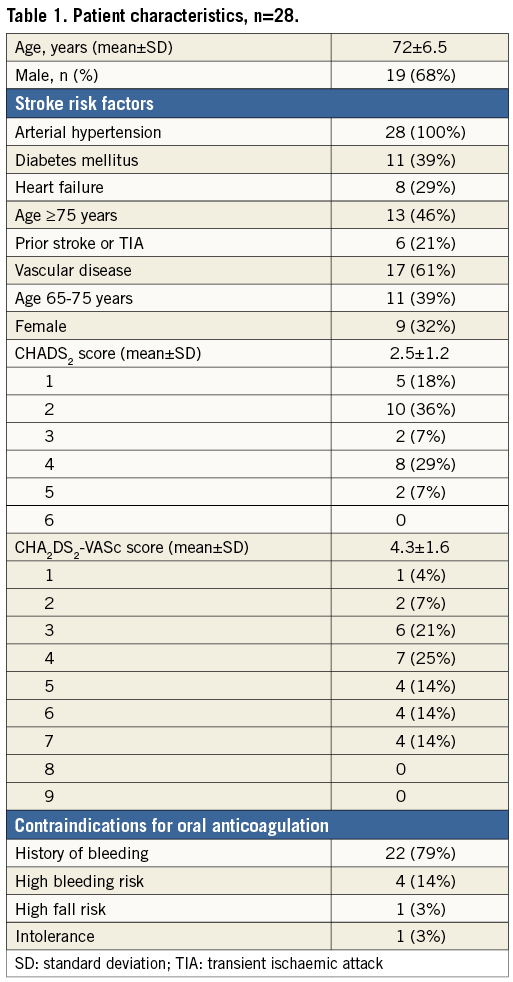
In this prospective single-centre, single-arm study, a total of 28 patients with non-valvular left atrial fibrillation (CHADS2 score ≥1 or CHA2DS2-VASc score ≥1) and contraindications for oral anticoagulation were enrolled. In all patients DW-MRI was performed within 24-48 hours before, 12-24 hours after the procedure, and during routine follow-up (after 45 days) for detection of cerebral ischaemia. Additionally, all patients underwent neurodiagnostic tests at the time of DW-MRI. During the procedure, we performed TCD monitoring for the detection of microembolic material. After approval by the institutional review board and written informed consent, consecutive patients were enrolled if they did not have a contraindication for MRI.
DEVICES, PROCEDURE AND POST-PROCEDURAL ANTITHROMBOTIC REGIMEN
The WATCHMAN closure device has been the most widely used in clinical practice. Characteristics and implantation procedure have been described in detail previously3,4. The device is delivered by endovascular means from the femoral vein via transseptal puncture to the left atrial appendage. Device implantation is performed under analgosedation with midazolam and propofol and transoesophageal echocardiography (TEE) guidance. Oral anticoagulation was stopped at least 24 hours before the intervention to achieve an international normalised ratio (INR) at least >1.5. In case of aspirin intake, patients continued on aspirin.
Heparin was administered routinely after transseptal puncture to achieve an activated clotting time >250 secs during the procedure. Different post-procedural antithrombotic regimens were used at the discretion of the interventionist. All patients received antithrombotic therapy for 45 days.
TRANSCRANIAL DOPPLER STUDY
Multifrequency Doppler (Multi-Dop® T digital, DWL®, QL software version 2.8; Compumedics Germany GmbH, Singen, Germany) was used for TCD monitoring in all patients. TCD monitoring was performed bilaterally. After both middle cerebral arteries were localised via the transtemporal window, transducers were fixated using a helmet-like holder to avoid displacement of the probes during the procedure. Microembolic signals were identified as recommended by the consensus criteria8. TCD monitoring was performed in real time throughout the whole procedure to rule out artefacts. Differentiation between solid versus gaseous microemboli was not possible with this TCD monitoring system. An experienced single reader (N. Majunke) interpreted the number of embolic signals offline unaware of the DW-MRI results.
The left atrial appendage closure procedure was divided into four steps:
– Transseptal puncture (defined as the 30-second period after crossing the interatrial septum with the transseptal needle).
– Positioning of the pigtail catheter in the LAA and LAA angiography (defined as the period from the introduction of the pigtail catheter to final LAA angiography).
– Positioning of the access sheath in the LAA and LAA angiography (defined as the period from the introduction of the access sheath, final positioning of the access sheath in the LAA to final LAA angiography).
– Implantation of the closure device (defined as the period from the introduction of the LAA closure device until the release of the device and removal of the deployment system).
Microemboli signals were evaluated separately during these different phases of the procedure.
MAGNETIC RESONANCE EXAMINATION
In all 28 patients, an MRI scan was performed within 24 hours prior to the intervention, shortly after the intervention (12-24 hrs) and after a period of 45 days. The scan was performed on a 3T-MRI scanner (Siemens MAGNETOM Verio; Siemens Medical Solutions USA, Inc., Malvern, PA, USA ) using a 12-element phased array head coil. The protocol consisted of a T2-fluid attenuated inversion recovery (FLAIR) sequence in an axial and sagittal orientation (TR=8,000 ms, TE=94 ms, slice thickness=5 mm) and a T2-turbo spin echo (TSE) sequence (TR=5,300 ms, TE=91 ms, slice thickness=5 mm), a diffusion weighted imaging (DWI) sequence including apparent diffusion coefficient (ADC) map (TR=6,700 ms, TE=94 ms, slice thickness=5 mm), a T2-gradient echo sequence (TR=693 ms, TE=19.9 ms, slice thickness=5 mm) and a T1-TSE sequence (TR=440 ms, TE=2.84 ms, slice thickness=5 mm), each in axial orientation.
Blinded image analysis regarding the occurrence and extent of acute and subacute ischaemic lesions was performed by an experienced radiologist (F. Eplinius) for each examination. Acute lesions were defined as diffusion restrictions in DWI sequences showing signal reduction in ADC mapping and no corresponding hyperintense lesion in FLAIR imaging. Subacute lesions were defined as diffusion restrictions in DWI imaging which were already demarcated as signal intense lesions in FLAIR. Detected lesions were measured in terms of their maximum extent and affected cerebral artery territory for all three MRI scans in each patient. In the 45-day control scans, additional new lesions on DW-MRI and the demarcation of post-procedural lesions in FLAIR imaging were quantified. Old ischaemic lesions were noted, but not included in further analyses.
NEURODIAGNOSTIC TESTS
All patients underwent neurodiagnostic tests at baseline, after the procedure and at follow-up, using the National Institutes of Health Stroke Scale (NIHSS) and the Montreal cognitive assessment (MoCA) test. The MoCA test has been validated for the assessment of vascular cognitive impairment after stroke9, and the NIHSS is a widely accepted tool to quantify stroke severity.
FOLLOW-UP
All patients were followed up 45 days after device implantation including transoesophageal echocardiography (to verify complete sealing of the LAA and to rule out thrombus), neurodiagnostic tests and DW-MRI.
STATISTICAL ANALYSIS
Data are presented as mean±standard error of the mean. Comparisons between the two groups were made with the Student’s t-test for continuous variables and with the chi-square test or Fisher’s exact test for categorical variables. A p-value of <0.05 was considered as statistically significant.
Results
A total of 28 patients were enrolled. Baseline characteristics of the included patients are shown in Table 1.
PROCEDURAL DETAILS
Procedural details are listed in Table 2. LAA closure was successful in all patients (100%). In three patients (11%), full recapture of the device was necessary due to a suboptimal initial positioning of the occluder. The mean fluoroscopy time was 6.4±3 min. The WATCHMAN device was used in all patients. Procedure-related complications occurred in two patients. One patient suffered from pharyngeal bleeding due to the TEE probe several hours after the procedure. The patient was intubated for safety reasons. After bleeding stopped, the patient was extubated and later discharged without sequelae. The second patient was monitored in the intensive care unit for 24 hours due to a transient bradycardia after implantation. Subsequent Holter ECG excluded relevant bradycardia and the patient was discharged without the need for additional intervention. The different post-procedural antithrombotic regimens used are shown in Table 2.
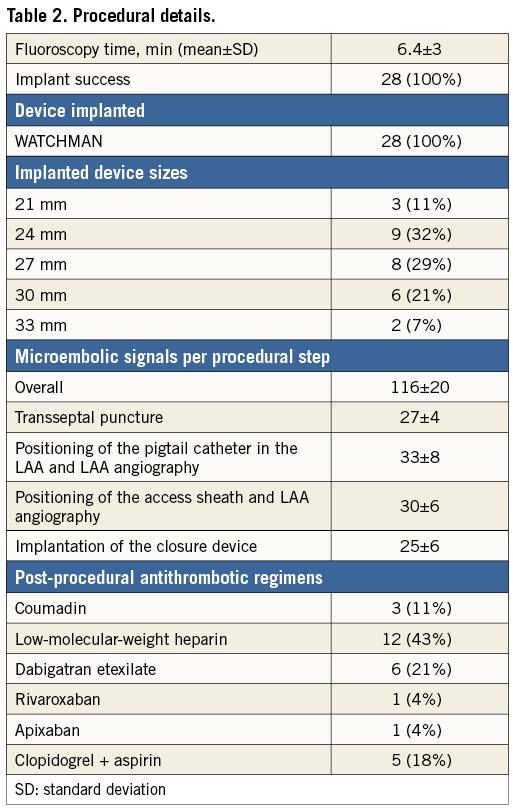
TRANSCRANIAL DOPPLER MONITORING
TCD monitoring was performed successfully in all patients (100%). We observed a mean of 116±20 total microembolic signals during the procedure. The number of microembolic signals per procedural step is shown in Table 2.
POST-PROCEDURAL DW-MRI
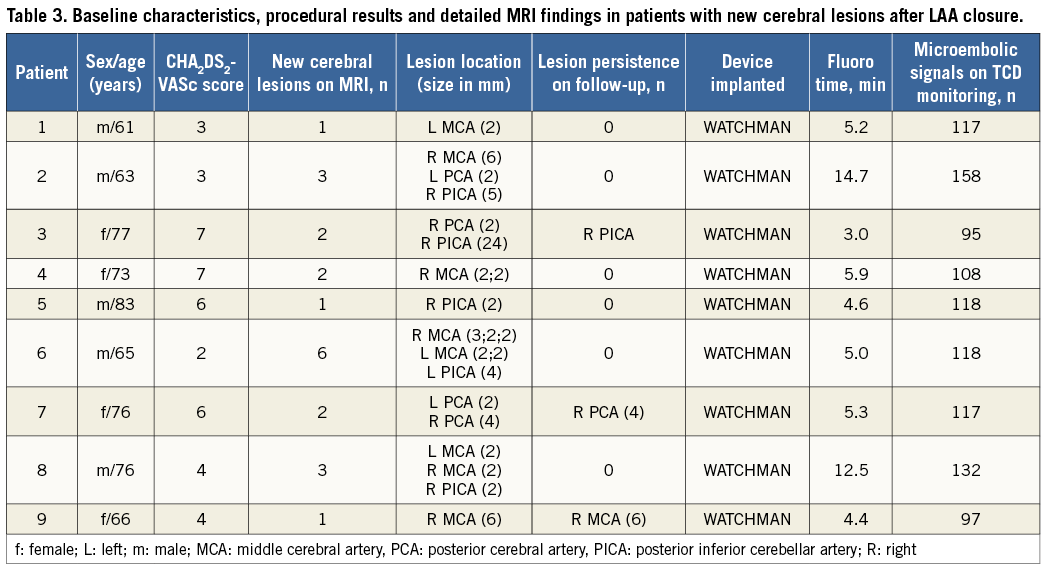
New ischaemic cerebral lesions at DW-MRI were observed in nine patients (32%) after the procedure. The median number of new ischaemic cerebral lesions per patient was 2 (range 1-6). Only one new cerebral lesion (1/28; 3.6%) was observed at 45-day follow-up DW-MRI. Only 33% of the new cerebral lesions after the procedure were still detectable as correlating gliotic lesions at the 45-day follow-up FLAIR sequences (Figure 1) and were not detectable in six of nine patients (66%). In particular, small lesions (between 2 and 4 mm) on DW-MRI showed no correlating lesion on the corresponding FLAIR image (Figure 2). Detailed MRI findings are shown in Table 3.
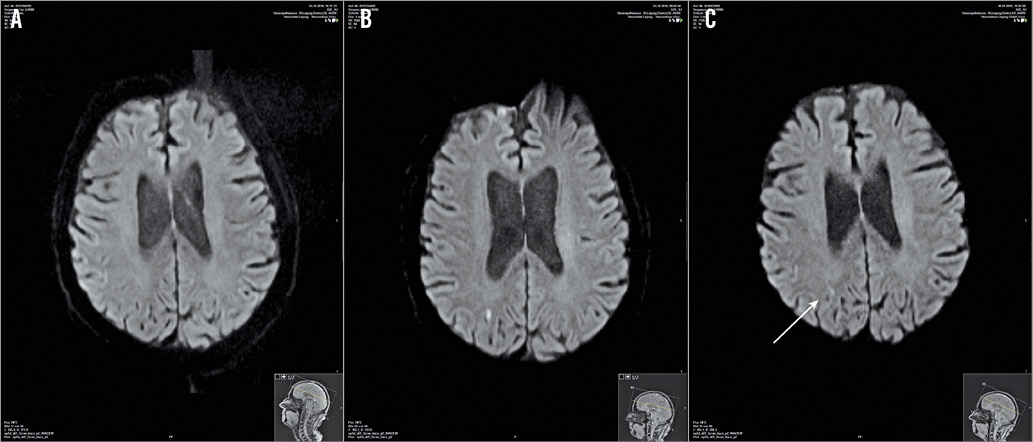
Figure 1. DW-MRI showing new cerebral lesions which persisted on control DW-MRI after 45 days. A) Preprocedural DW-MRI showing no cerebral lesions. B) DW-MRI shows new right-sided cerebral lesion the day after left atrial appendage closure. C) Control T2-FLAIR-MRI shows a small gliotic lesion correlating to the post-procedural lesion seen in panel B (white arrow). DW-MRI: diffusion-weighted magnetic resonance imaging
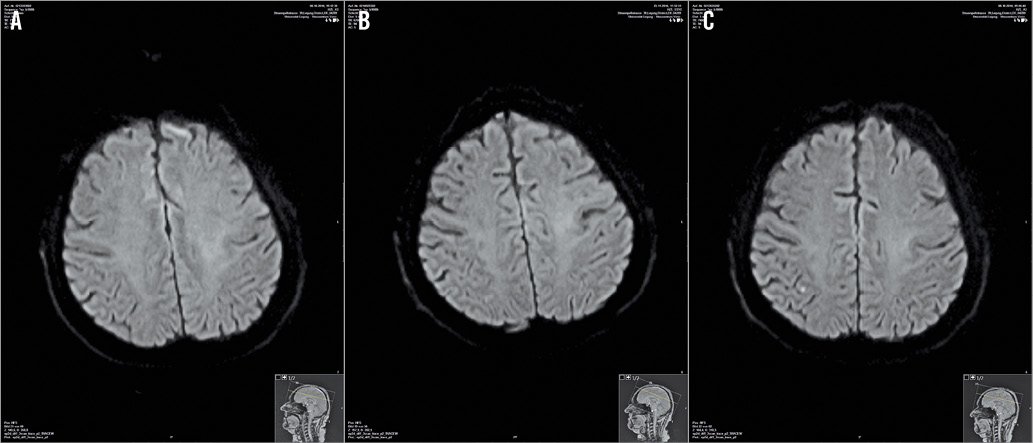
Figure 2. DW-MRI showing new cerebral lesions which disappeared on control DW-MRI after 45 days. A) Preprocedural DW-MRI showing no cerebral lesions. B) DW-MRI shows new right-sided, small cerebral lesion the day after left atrial appendage closure. C) Control T2-FLAIR-MRI shows no correlating lesion. DW-MRI: diffusion-weighted magnetic resonance imaging
Neither the NIHSS nor the MoCA test showed any neurological deficits in patients with or without cerebral lesions (Table 4).
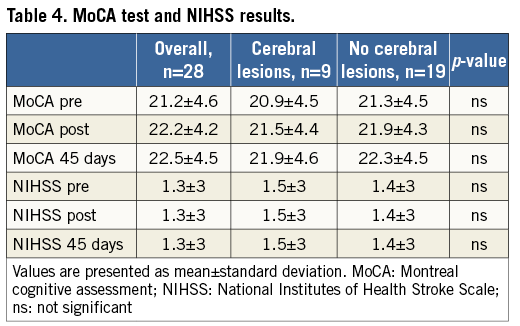
There was no relationship between the numbers of microembolic signals on TCD monitoring and the occurrence of new ischaemic cerebral lesions on DW-MRI (mean 121±20 in patients with new cerebral lesions vs. mean 116±20 in patients without new cerebral lesions, ns).
FOLLOW-UP
All patients (100%) completed the 45-day follow-up visit (mean 45±6 days). TEE showed complete closure of the LAA in all patients (100%) without evidence for new thrombus formation on the device. One patient was re-hospitalised seven days after the procedure due to a femoral artery pseudoaneurysm. The patient underwent surgery, which was uneventful.
Discussion
The finding of silent cerebral infarctions represents a common phenomenon in the general population (up to 20% in healthy elderly people) and is associated with cognitive impairment, dementia, and clinically apparent stroke10.
In recent years, several neuroimaging studies have shown that left heart catheterisation is associated with periprocedural cerebral infarctions; however, the large majority are clinically silent6. Depending on the procedure, the incidence of silent cerebral lesions varies from 72% to 93% after transcatheter aortic valve implantation11,12, 22% after retrograde catheterisation of the aortic valve in patients with aortic stenosis13, and 4% to 41% after pulmonary vein isolation for atrial fibrillation14,15. However, the clinical implications of asymptomatic ischaemic lesions after invasive cardiac interventions remain unclear.
Transcatheter closure of the LAA is an emerging alternative to oral anticoagulation for stroke prevention in patients with atrial fibrillation. Despite the good safety profile of this intervention, procedural complications may occur. The clinically apparent periprocedural stroke rate of WATCHMAN implantation ranges from 0.1%-1.9%3,5,7. Fundamentally, transcatheter closure of the LAA was introduced with the aim of preventing strokes without increasing the bleeding risk. As such, avoidance of periprocedural cerebral embolism is of paramount importance.
Possible mechanisms of cerebral embolism during transcatheter closure of the LAA are: 1) air embolism during contrast dye injection or saline flush due to trapped air, 2) embolism of parts of the interatrial septum after transseptal puncture, 3) embolism of thrombi from catheters or guidewires, and 4) mobilising thrombi from the LAA during catheter manipulation or contrast dye injection.
We observed new ischaemic cerebral lesions as seen on DW-MRI in 32% (9/28) of patients in the early period after transcatheter closure of the LAA. Neither patients with new cerebral lesions nor the remaining patients showed any neurological deficits immediately after the procedure or during follow-up. Partial or full recapture of the device was necessary in three patients but did not result in new cerebral lesions. These results suggest that left atrial appendage closure with the WATCHMAN occluder is a safe procedure regarding periprocedural stroke when performed by experienced interventionalists.
It has been reported that there is an association between the number of solid cerebral microemboli and the occurrence of silent cerebral lesions after left heart catheterisation16. In this study, periprocedural TCD monitoring showed that transcatheter closure of the LAA causes cerebral microemboli, but there was no correlation between microembolic signals on periprocedural TCD monitoring and the occurrence of new cerebral lesions on DW-MRI. Both gaseous and solid material cause microembolic signals on TCD. It is conceivable that many microembolic signals are partially gaseous in origin which rarely causes cerebral lesions on DW-MRI. Nevertheless, due to the lack of differentiation between solid and gaseous emboli in our study, a possible correlation between solid microemboli and silent cerebral lesions cannot be excluded. Further studies may use transcranial Doppler systems which can differentiate between gaseous and solid emboli or even use distal embolic protection devices to differentiate embolic material and sources.
On the second DW-MRI performed 45 days later, new cerebral lesions were detected in only one patient, and post-procedural ischaemic lesions later demarcated in 45-day follow-up FLAIR sequences were found in three patients. All of these lesions demarcated in FLAIR sequences showed an extent of >4 mm. These observations are consistent with a study by Deneke et al, in which >90% of small cerebral lesions (<4 mm) after catheter ablation of atrial fibrillation were not detectable any more during follow-up17. One possible reason why most of the lesions were not detectable in follow-up FLAIR images might be the small extent of the majority of these lesions: they may not be captured in FLAIR sequences with 5 mm slice thickness due to scar shrinkage and remodelling processes. Another reason could be a complete reconvalescence of these microembolic foci without leaving any gliotic scar.
Limitations
This study has some limitations. First, it is a single-centre experience with a small sample size which may be a limitation in the interpretation of the data. Second, one interventional cardiologist skilled in deploying the WATCHMAN closure device performed all procedures, which may have contributed to the favourable results. Hence, the results of the present study require validation in larger studies. Third, the origin of the embolic lesion is unclear. Therefore, further studies may include the use of distal embolic protection devices to clarify the origin of these cerebral lesions.
Conclusions
Our observations suggest that transcatheter LAA closure is associated with asymptomatic cerebral embolism on DW-MRI in the early phase after the procedure. Nevertheless, most of the cerebral lesions are small and may disappear without visible gliotic formation within 45 days. Larger studies are needed for the validation of these preliminary results.
| Impact on daily practice Transcatheter closure of the left atrial appendage using the WATCHMAN device may result in small asymptomatic cerebral embolism on diffusion-weighted magnetic resonance imaging (DW-MRI), when performed by an experienced operator. Most of the lesions are transient and disappear on follow-up DW-MRI. Larger studies are needed to confirm these findings. |
Conflict of interest statement
S. Möbius-Winkler and M. Sandri are working as proctors for WATCHMAN device implantation for Boston Scientific, Germany. The other authors have no conflicts of interest to declare.