Abstract
Aims: To create awareness of, to summarise and to classify “Slender TRI”: any technique associated with less trauma to the radial artery compared to traditional, established or recommended procedures, predominantly by reduction of French (Fr) size.
Methods and results: A literature search was conducted to identify publications on Slender transradial coronary interventions. Based on this search the following techniques will be described: miniaturisation of materials, sheathless coronary intervention, guideless coronary intervention and back-up-improving techniques. The European perspectives will be discussed.
Conclusions: Slender TRI is a new challenge to maximise patient value by improving outcome and reducing costs during TRI. Materials and techniques are continuously being refined and miniaturised to the highest standards. Whether outcome improves while reducing costs remains to be validated.
Introduction
Accumulating data have resulted in evidence that transradial coronary interventions (TRI) are safer than transfemoral coronary interventions (TFI) because of reduced bleeding complications1. Bleeding after coronary interventions is associated with mortality, and TRI has been shown to improve survival2,3, especially in the setting of primary percutaneous coronary interventions (PPCI) for acute myocardial infarction (AMI)4. In 2013, the European Society of Cardiology (ESC) officially recommended the radial approach as the preferred entry site for coronary interventions5. In the setting of PPCI, the radial approach became a Class IIa, level B recommendation. Later, the Society for Coronary Angiography and Interventions (SCAI) declared in a consensus statement that TRI is preferred over TFI6.
TRI is usually performed with 6 Fr catheters, with an outer diameter of 2 mm and a corresponding sheath outer diameter of 2.7 mm. Radial artery diameters vary widely from 1.5 to 4 mm7. This catheter size is therefore too large for patients with small radial arteries, making this technique painful, cumbersome and sometimes unsafe. In addition, radial artery occlusion (RAO) is more common when guides are large in comparison to the radial artery. This rarely results in ischaemic complications of the hand but limits further radial access in that arm. This mismatch between radial lumen and interventional equipment sizes was first recognised in Asian countries such as Japan, where the transradial access became the default approach at a very early stage and where radial artery diameter, correlated with body surface area, is also smaller7 (Figure 1). This led to the development of equipment and techniques to overcome this problem.
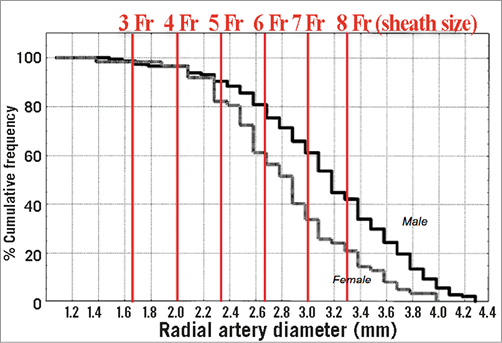
Figure 1. Cumulative frequency of radial artery diameters.
The Japanese use the word “Slender” for this new approach. Actually, any technique can be considered to be “Slender” if associated with less trauma to the radial artery compared to traditional, established or recommended procedures, either by reduction of French size, reduction of vascular access sites or by reduction of haemostatic vascular damage. Usually the term “Slender” is applied when catheters <6 Fr are used.
Slender Club Japan
In order to adapt TRI for Japanese patients, Japanese radialists started to downsize TRI equipment. This has been supported by several studies showing fewer bleeding complications with the use of smaller catheters8-10.
This “movement” in downsizing PCI equipment resulted in the establishment of the Slender Club Japan (SCJ), initiated by Dr Fuminobu Yoshimachi. Ten years later, many new miniaturised materials have been developed and introduced in Japan. Sheathless introduction and the small size of catheters make them more difficult to manipulate. Lack of back-up support can lead to failure to deliver intracoronary therapy. To overcome these difficulties, techniques such as creating loops, deep intubation, use of extra wires and anchoring techniques have been developed. The whole range of these extra manoeuvres is called “Slender TRI”. By organising frequent regional workshops and national meetings, the slender techniques became popular in Japan.
Slender Club Europe
The benefits of Slender TRI apply to all patients, not only to Asian patients. The smallest available catheters in Japan are 3 Fr for coronary angiography, and 4 Fr for TRI. Smaller guides require smaller balloons, stents and wires, which are also available exclusively on the Japanese market. In Europe, these materials have not been CE-marked as yet, but that needs to change, since even with downsized material complex coronary pathology can be addressed when proper techniques and manoeuvres are applied.
The Slender Club Europe (SCE) aims to translate and adapt the Japanese experience to the European situation. In addition, SCE can be a platform for training, education and research.
Slender techniques
We searched Pubmed, ISI Web of Knowledge, and the Cochrane Library with combinations of the search terms “slender”, “radial”, “transradial”, “coronary”, “intervention” and “virtual”. Relevant manuscripts were reviewed and references were searched for relevant articles. Based on this information, slender techniques can be classified into:
I. Miniaturisation of materials
a. Sheaths
b. Catheters
i. Guides
ii. Diagnostic catheters
c. Wires and balloon catheters
II. Sheathless coronary intervention
a. Sheathless systems
b. Long dilators
c. Balloon-assisted tracking
III. Guideless coronary intervention
IV. Back-up-improving techniques
a. Loops
b. Anchor wire
c. Anchor balloon
d. Parallel wire
e. Mother and child
f. Special techniques for CTO
Miniaturised coronary intervention
SHEATHS
Recently, a sheath with an outer diameter close to a 5 Fr sheath, but compatible with a 6 Fr guiding catheter, was developed (Glidesheath Slender® [GSS]; Terumo Corp., Tokyo, Japan). The sheath thickness has been reduced from 0.20 to 0.12 mm. Aminian et al reported on a series of 114 consecutive TRI patients11. Procedural success was obtained in 99.1% of cases with symptomatic radial spasm (RAS) occurring in 4.4%. At one-month follow-up, one case of radial artery occlusion (RAO) was identified.
DIAGNOSTIC CATHETERS
3 FR CORONARY ANGIOGRAPHY
Exclusively in Japan, 3 Fr diagnostic catheters have been developed by two manufacturers (Fukuda Denshi Co., Ltd, Tokyo, Japan, and Medikit Co., Ltd, Tokyo, Japan). The catheters from Medikit are actually 3.3 Fr. They can be inserted via a 3 Fr sheath. These 3 Fr catheters are compatible with a 0.025 inch guidewire. In order to obtain good images, a pressure injector is required. To avoid disengagement of the catheter during injection and to increase safety, the tip of the catheter has side holes. Currently, 2.8 Fr diagnostic catheters are being developed in Japan. In Europe, BALT (Montmorency, France) is developing 3 Fr catheters with side holes.
GUIDE CATHETERS
5 FR VERSUS 6 FR TRI
Although focus has been placed on the reduction of the outer diameter of catheters, it is important to realise that the inner diameter (ID) of 6 Fr guides has increased from 0.06 inch in the mid 1990s to 0.072 inch today (which was the inner diameter of the old 8 Fr catheters). Similarly, current 5 Fr guiding catheters have the same ID as the first 6 Fr guides.
In the late 1990s, due to continued miniaturisation, stents could also be implanted via 6 Fr guides instead of the standard 8 Fr guides. Later, further downsizing of equipment made it possible to perform PCI via 5 Fr and even 4 Fr guides. The earliest publications on TRI comparing small-size catheters were published in 2004 and 200612,13. In the first study, 213 patients undergoing TRI were randomised to either 5 Fr or 6 Fr sheaths and guiding catheters. Procedural success was similar (5 Fr 90% vs. 6 Fr 95%, p=0.025). Crossover to the 6 Fr group occurred in 6.8% of cases while one patient (0.9%) crossed over from the 6 Fr to the 5 Fr group due to a small radial artery12. In the second study, 200 patients were randomised to 6 Fr or 5 Fr TRI. Procedural success rates and the incidence of local complications were similar. The authors reported lower wound pain scores with 5 Fr TRI13. Uhlemann et al reported fewer access-site complications, defined as RAO, haemorrhage, pseudoaneurysm, or arteriovenous fistula, with 5 Fr sheaths in 455 patients undergoing TRI (5 Fr n=153, 6 Fr n=302)14.
Recently, a retrospective study comparing 493 patients undergoing small Fr coronary interventions (defined as <6 Fr sheaths or sheathless guide catheters up to 7.5 Fr) with 6,248 patients undergoing large Fr PCI, reported lower contrast use with small Fr PCI15.
4 FR TRI
A 4 Fr guiding catheter (KIWAMI, Heartrail® II; Terumo Corp.) has been developed to facilitate TRI16. One study has reported procedural characteristics and outcomes of 62 patients undergoing 4 Fr PCI17. In this registry, 76% of cases were performed transradially. Cases were divided into two groups, an early phase (first 26 patients performed in 2007), and a late phase (36 patients performed later). Although procedural success rates were similar (94% vs. 95%, p=NS), a learning curve was observed with reductions in fluoroscopy time (17±15 vs. 8±6 min, p<0.05) and contrast dye volume (90±46 vs. 64±33 ml, p<0.05) over time.
WIRES AND BALLOON CATHETERS
TRI USING A 0.010 INCH GUIDEWIRE
To reduce the invasiveness of TRI further, 0.010 inch guidewires and compatible balloon catheters have been developed. Matsukage et al reported on 133 patients who underwent PCI using this 0.010 inch system18. Transradial access was used in 79.7% of cases with an average guiding catheter size of 5.1 Fr. This registry included complex lesions, with 60.2% type B2/C lesions, 22.3% bifurcation lesions, 16.9% CTO lesions, and 8.1% ostial lesions. The lesions were successfully passed with a 0.010 inch guidewire and successfully dilated with a 0.010 inch compatible balloon in 99.2% of lesions. However, the stent delivery success rate was 93.9% because of failure to deliver the stent in eight lesions.
The feasibility of using the 0.010 inch system in CTO lesions was reported in a registry of 141 patients19. TRI was used in 76.6% of cases with an average guiding catheter size of 5.8 Fr with a success rate of 88.7%. The 0.010 inch system can also be used to perform kissing balloon technique (KBT) using a 5 Fr guiding catheter20, or even simultaneous triple balloon inflation using a 6 Fr guide21.
Sheathless coronary intervention
An alternative method for reducing the invasiveness of PCI is to perform sheathless interventions. By eliminating the use of an arterial sheath, arterial injury at the access site can be minimised, as the outer diameter (OD) of a sheath is approximately 2 Fr larger than the corresponding catheter. The concept of “Virtual TRI” is related to sheathless procedures.
THE “VIRTUAL TRI” CONCEPT
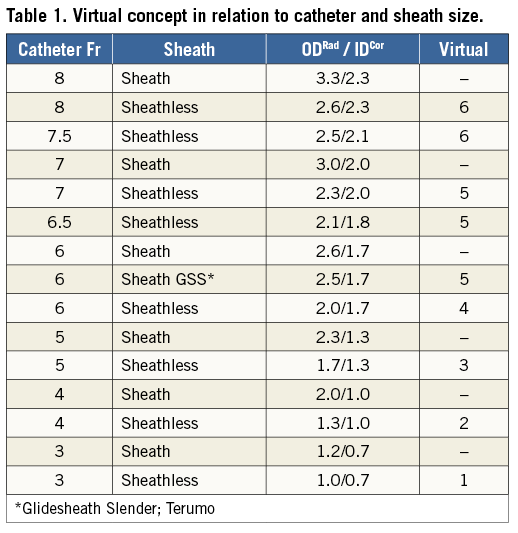
Based on the assumption that the sheath of a catheter is 2 Fr larger than the corresponding catheter, S. Saito has introduced the term “virtual” for sheathless procedures. For example, a sheathless 6 Fr procedure is called “virtual 4 Fr” and a sheathless 5 Fr procedure “virtual 3 Fr”, and so on. Although easy to understand among radialists familiar with slender techniques, it may be confusing for others and is sometimes ambiguous.
French size refers to OD of a guide, but for a sheath it is the maximum guide size that it can accommodate. Consequently, the OD of a sheath depends on its wall thickness, which varies among manufacturers and is not always 2 Fr larger than the corresponding guide. For instance, a 6 Fr GSS is 0.5 Fr thinner walled than a standard 6 Fr Glidesheath, so is this a virtual 5.5 Fr, or a virtual 5 Fr system? Similarly, 3 Fr and 4 Fr sheaths are often only 1 Fr or 1.5 Fr thicker than the corresponding guides, so it is not correct to refer to “virtual 1 Fr” if a 3 Fr catheter is used without a sheath. Similarly, the ID of a guide also depends on its wall thickness, so a 6.5 Fr Eaucath sheathless guide (ASAHI Intecc, Aichi, Japan) has the same ID as a conventional 6 Fr guide (0.070”). Finally, the sheathless 6.5 Fr and 7.5 Fr systems from ASAHI and Medikit should be referred to as virtual 4.5 Fr and 5.5 Fr respectively, but these sheaths do not exist.
A NEW DESCRIPTION OF THE SLENDER TECHNIQUE
Since “virtual” has become a common term for unsheathed TRIs or for sheath modification, and since papers using this term have already been published22, it seems better not to abandon this concept, but to extend it with the actual sizes of materials used. The major target of slender procedures is to use the smallest possible sheath or catheter in contact with the radial artery wall, making the OD of the sheath or catheter the most relevant factor determining the “slenderness” of the procedure. On the other hand, the major target of the coronary intervention itself is to cure the coronary lesion, with the ID of the catheter the factor that determines the size of materials and techniques which can be advanced.
Thus, Slender TRI is characterised by two factors: first, the OD of the device in contact with the radial artery wall (sheath or catheter’s ODRad in mm) and, second, the ID of the catheter which facilitates the crossing of intracoronary devices (catheter’s IDCor in mm). In general, the catheter’s ID corresponds with its OD minus 1 Fr (0.33 mm). Preferably the actual sizes (in mm) should be used, not the calculated sizes from Fr to millimetres, since many different companies refer to a certain Fr size while the size in mm may show relevant variation. Using this nomenclature, we propose describing slender systems in terms of ODRad (mm), IDCor (mm) and equivalent OD in terms of (virtual) Fr size (Table 1).
Sheathless techniques
SHEATHLESS SYSTEMS
Specialised systems for sheathless PCI have been developed by two Japanese companies. The 5 Fr sheathless guiding catheter (Medikit Co., Ltd) is advanced using a specialised insertion system. Use for treatment of complex coronary artery disease has been described in detail23. Successful treatment of CTO lesions has been shown to be possible with this system24, and a recent case report showed that a 4 Fr guiding catheter (KIWAMI, Heartrail; Terumo Corp.) can be inserted into the 5 Fr guiding catheter to improve stent delivery25.
Recently, Tonomura et al reported on 132 consecutive patients who underwent PCI using this system23. The procedural success rate was 95%. Six patients required conversion to a conventional 5 Fr or 6 Fr sheath; no RAO was observed. Medikit has also developed a 6.5 Fr sheathless system with a larger ID than a conventional 6 Fr guide (release awaited).
ASAHI Intecc has introduced 6.5 Fr and 7.5 Fr sheathless Eaucath guide systems. The 7.5 Fr system has the same ID as a conventional 7 Fr guide (0.081”), and an OD slightly smaller than a 6 Fr sheath. This system allows for complex TRI, as demonstrated by an observational study in 120 patients including 68% type B2/C lesions and nine patients undergoing primary PCI. The angiographic success rate was 97.5%26 and RAO occurred in 2.3%. A smaller series of 16 patients undergoing complex TRI, including rotablation, crush stent bifurcation lesions, proximal protection and thrombectomy devices, had previously demonstrated the feasibility of this system27. Transradial simultaneous kissing stenting of bifurcation lesions has also been reported28.
The 6.5 Fr sheathless Eaucath system has an ID equivalent to a 6 Fr guide (0.070”) and an OD less than a 5 Fr sheath. This has been shown to be feasible for both routine TRI, in 100 consecutive patients, and in 148 selected patients with more complex lesions29.
LONG DILATORS
Conventional catheters can be inserted directly into the radial artery following predilation of the subcutaneous tissue. Sheathless TRI using standard guides has been reported to be feasible and safe in a small 10-patient case series30. However, since the guide is not tapered down onto the wire, it may cause a razor effect between the guide and the arterial wall. To avoid this, special long dilators, compatible with 5 Fr guides from several manufacturers, have been developed by Terumo and by Medikit. These long dilators are not available on the European market. As an alternative, Vascular Solutions (Minneapolis, MN, USA) have developed a “Flip” dilator (FDA approved, CE mark imminent). This dilator incorporates a sleeve at the tip which covers and protects the tip of the guide during insertion through the skin. This sleeve then inverts when pulled to allow subsequent withdrawal of the dilator.
BALLOON-ASSISTED TRACKING
Another technique for atraumatic sheathless guide insertion is BAT (balloon-assisted tracking)31-33. This involves a 6 Fr or 5 Fr guide, loaded respectively with a 2.0 or 1.5 mm compliant balloon over a 0.014” coronary wire. The balloon is kept partially outside the distal end of the guiding catheter, followed by soft inflation of four bars to ensure fixation of the guiding catheter onto the coronary wire. As such, the guide catheter tapers perfectly over the soft balloon and the balloon over the guidewire. This results in smooth engagement of the assembly into the ascending aorta.
Guideless coronary intervention
A recent case report described guideless IVUS-guided PCI using a technique called “the emperor’s new clothes technique” because TRI was performed as if an invisible guiding catheter was employed34,35. After coronary angiography using a 4 Fr diagnostic catheter through a 4 Fr sheath, a guidewire was advanced through the diagnostic catheter which was subsequently removed, leaving the guidewire in place. An IVUS catheter was used to determine the vessel diameter and lesion length. After predilation, a 3.0×18 mm DES was implanted. The IVUS catheter, predilation balloon, and stent were all advanced over the guidewire without the use of a guiding catheter. In this case, the need for a guide catheter for visualisation was obviated by application of IVUS, for blood pressure registration by the side arm of the sheath and for back-up support by the support qualities of the guidewire.
Back-up-improving techniques
Slender catheters are not strong enough to provide good back-up support, but they have excellent flexibility. This allows the following back-up techniques.
LOOPS
Loops are created by excessive push on the guide while giving clockwise or counterclockwise rotation, resulting in extra back-up force from the opposite aortic wall and coaxialisation of the catheter. Three different loops are practised: the α (alpha)-loop is used for LAD lesions (Figure 2), the γ (gamma)-loop is used for CX lesions (Figure 3), and the ε (epsilon)-loop is used for RCA lesions (Figure 4).

Figure 2. Alpha loop.
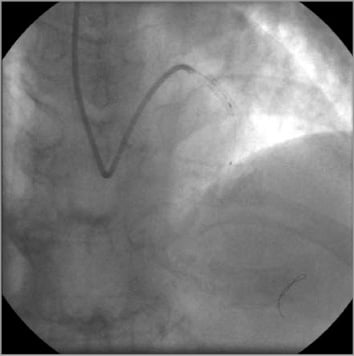
Figure 3. Gamma loop.
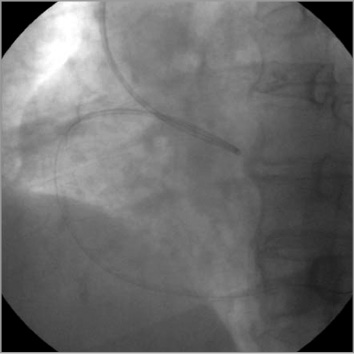
Figure 4. Epsilon loop.
ANCHOR WIRE
The anchor wire (dummy wire) technique36 means that a second guidewire is inserted into the non-target coronary artery, to improve back-up support. This technique is very useful when using a 4 Fr guide. In terms of compatibility, two 0.014” guidewires with a 3.0 mm stent can pass through a 5 Fr guide and, with some resistance, two 0.014” guidewires and the most recent generation 3.5 mm stents can pass through a 5 Fr guide. Two 0.014” guidewires and a 3.0 mm balloon can pass through a 4 Fr guide. However, two 0.014” wires and a stent cannot pass a 4 Fr guide.
ANCHOR BALLOON
Using this technique, a balloon is inflated distally in the target coronary artery to engage a 4 Fr or 5 Fr guide very deeply. After retrieving the balloon, a stent can be delivered directly into the target lesion. The original anchor balloon technique37, in which a balloon remains inflated on one wire whilst a stent is advanced on a second wire, requires 6 Fr or 7 Fr guides.
PARALLEL WIRE
The parallel wire technique is effective in treating complex lesions, including CTOs38,39. This technique helps to increase back-up support and stability of the guide catheter by advancing two wires over the target lesion.
MOTHER AND CHILD
The mother and child technique refers to the introduction of a smaller bore catheter into the guide catheter in order to increase back-up support. It is an effective and commonly used strategy during Slender PCI40.
SPECIAL TECHNIQUES FOR CTO
Over 60% of CTOs can be treated by tapered soft or stiff guidewires19. When the wire cannot cross the CTO by the antegrade approach, a special technique can be used called “SATAI” (Stiff And Tapered guide wire penetration technique on Antegrade Intervention). A stiff tapered guidewire is manipulated intentionally into the subintimal layer of the target artery. The result is: i) improved stability and back-up force of the guide catheter, ii) improved orientation just as with the parallel guidewire technique, and iii) lesion modification41. The small dissection made by the 0.014” guidewire will be sealed after stenting the CTO.
Slender procedures in Europe: current situation and future perspectives
Full adoption of slender techniques in Europe is at present limited by the equipment available. To develop and manufacture Slender PCI products requires higher quality standards than conventional equipment, and the volume of sales would initially be limited. This makes commercialisation of such equipment challenging, and has until now discouraged European manufacturers from investing in the development of slender products. Similarly, international companies seem either not interested in these types of products (North American companies) or reluctant to take on the costs and efforts of European registration (Japanese companies). Slender PCI materials currently available in Europe include 4 Fr diagnostic catheters (Terumo Corp., and Cordis, Johnson & Johnson, Warren, NJ, USA), 5 Fr guiding catheters (many manufacturers), 6.5 Fr and 7.5 Fr sheathless guiding catheters (ASAHI Intecc), the 6 Fr Glidesheath Slender introducer (Terumo Corp) and the Svelte™ Integrated Delivery System (IDS) stent (Svelte Medical Systems, New Providence, NJ, USA). 5 Fr sheathless guiding catheters (Medikit) are likely to be available soon, with CE mark approval pending. This will allow European operators to perform “virtual” 3 Fr PCI procedures, as described above. There are already some seminal European experiences with this guiding catheter (OLVG, Amsterdam, The Netherlands), as well as with the use of a 4 Fr diagnostic coronary catheter (Pilsen, Czech Republic) for implantation of the Svelte IDS stent. A first generation of 3 Fr diagnostic coronary catheters (BALT) is available and being used at Tergooi, Blaricum, The Netherlands. The use of sheathless (6.5 Fr and 7.5 Fr) coronary guiding catheters has predominantly been second-line, either for complex PCI when a large lumen is required (7.5 Fr - rotablator, CTOs, left main PCI) or for routine PCI with a small radial artery (6.5 Fr). However, due to differences in the performance of these catheters and with a learning curve required for use, uptake has been concentrated in certain experienced centres. The thinner walled 6 Fr GSS has only recently been introduced, but its use is increasing rapidly, combining the diameter and convenience of a 5 Fr sheath with the familiarity of using conventional 6 Fr guides.
Currently, however, 5 Fr conventional TR-PCI can still be considered the mainstay of Slender PCI in Europe. Some European centres perform 5 Fr PCI procedures as standard, and many centres perform 5 Fr procedures in a substantial proportion of patients42. There are many 5 Fr-compatible devices, including all coronary balloons, most stents (all current balloon-expandable DES, BVS, up to 3.0 mm), protection devices (SpiderFX™; ev3 Inc., Plymouth, MN, USA) and imaging catheters (FastView OFDI; Terumo Corp., Eagle Eye® IVUS; Volcano Corp., Rancho Cordova, CA, USA). Single-layer 5 Fr-compatible covered stents (Biotronik, Berlin, Germany) are also available on the European market. Looking towards the future, the availability of 0.010”-compatible balloons (already CE marked) and 5 Fr-compatible manual aspiration catheters (being developed) will allow European operators to treat bifurcations and primary angioplasty routinely through a 5 Fr guiding catheter. This will be a major step forward, allowing the majority of procedures to be compatible with 5 Fr. Furthermore, with the introduction of 5 Fr sheathless guides and the prospect of 5 Fr thin-walled sheaths (already planned), truly Slender PCI will become a reality.
The advantages of downsizing to 5 Fr are well established, including proven reductions of bleeding complications, radial occlusion, contrast use and haemostasis time, thereby facilitating same-day discharge, completing the Slender logistic (Figure 5).

Figure 5. Same-day discharge department (PCI Lounge) at OLVG, Amsterdam, The Netherlands.
Limitations
Although these developments are pushing the technical refinement of PCI material to the limit and there are clear theoretical benefits, the true value of Slender TRI still has to be validated in larger randomised studies. The thin-walled catheters, for example, are more prone to damage and are more difficult to position and to handle. Poor back-up support can result in procedural difficulties. As 5 Fr guiding catheters are not compatible with some angioplasty equipment such as rotational IVUS imaging catheters, ≥1.5 mm rotablator burrs, thrombus aspiration catheters, BVS >3 mm, or ≥3.0 mm cutting balloons, this approach is not suitable for all lesion types, and careful patient selection is necessary. The lumen of 4 Fr and 3 Fr catheters can impair adequate visualisation and interpretation of the coronary pathology, and care needs to be taken to avoid air embolism. Without experience and careful patient selection, these factors may result in suboptimal treatment success, and prolonged procedural and fluoroscopy times. Procedural costs may rise, not only due to the greater cost of slender catheters but also due to the greater use of mother and child catheters and the additional wires and balloons needed for anchoring techniques. Slender TRI is certainly associated with a learning curve17 and, as the availability of slender equipment improves and experience worldwide is gained and shared, success will undoubtedly continue to rise. It will then be important to test if all the presumed advantages of Slender TRI, including prevention of RAO, contrast-induced nephropathy and improved patient comfort, outweigh these technical challenges. The point at which further miniaturisation impacts adversely on clinical efficacy and/or financial sustainability (“the law of diminishing returns”) is unknown.
| Impact on daily practice Miniaturisation of materials dedicated to transradial coronary access might result in increased patient value by improving outcome and by reducing costs. However, improved patient value of so-called “Slender TRI”, although promising, still needs to be validated. Use of downsized equipment requires special skills and manoeuvres and is certainly associated with a learning curve. |
Conflict of interest statement
D. Fraser is a medical advisor to Vascular Solutions, Minneapolis, MN, USA. The other authors have no conflicts of interest to declare.

