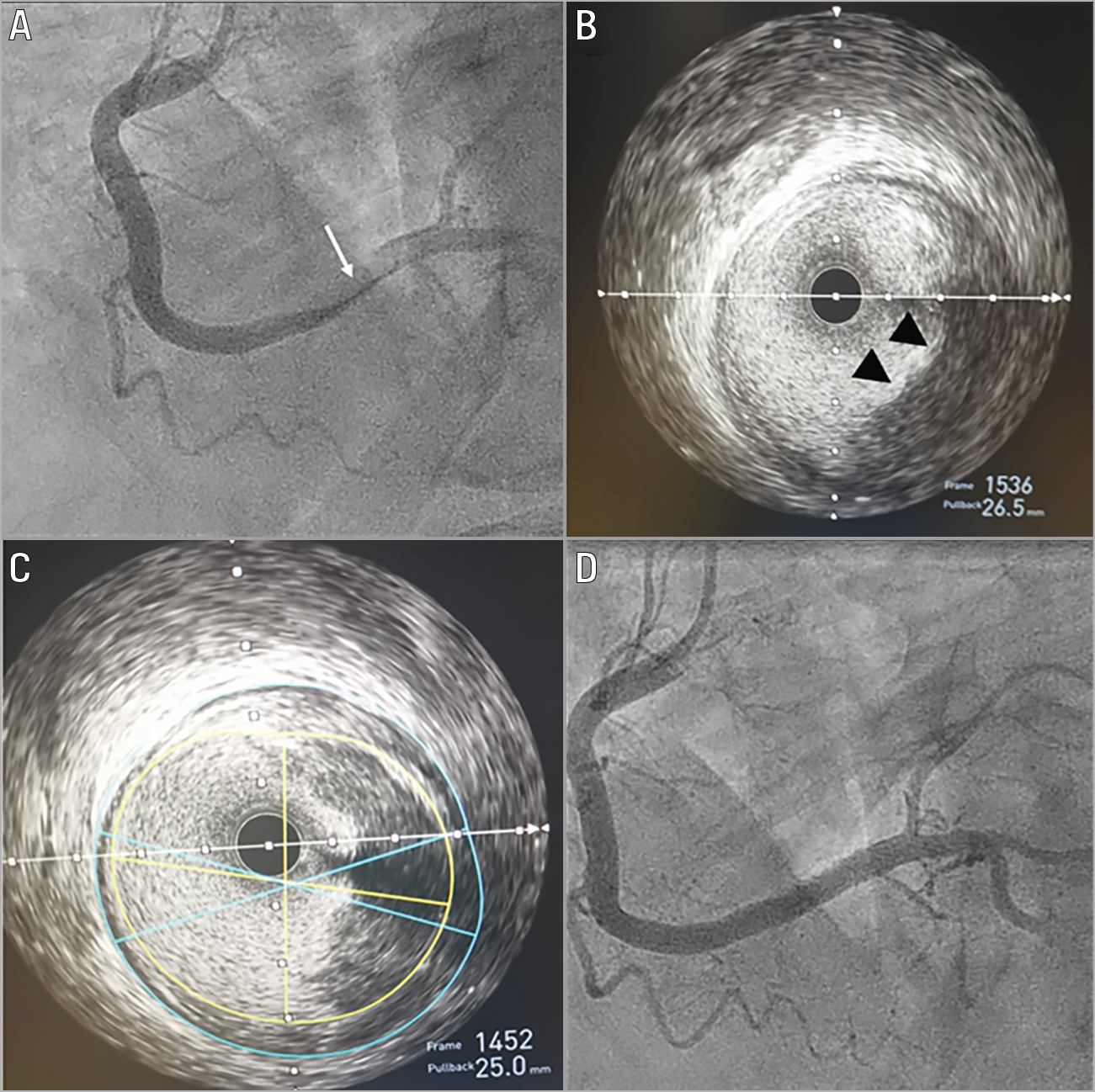
Figure 1. Extensive right coronary artery thrombosis associated with COVID-19. A) Angiogram of the right coronary artery showing large thrombus (arrows) with subtotal occlusion of the distal vessel. B) & C) Intravascular ultrasound of the same vessel showing fresh thrombus (arrowheads) with a minimal lumen area of 21.7 mm2 and only 29% plaque burden (C). D) Coronary angiography following successful PCI to the distal vessel but with distal thrombotic pruning.
A 51-year-old male with hypertension, established type 2 diabetes mellitus and hypercholesterolaemia presented with acute respiratory distress syndrome. A chest radiograph showed bilateral infiltrates, and a real-time polymerase chain reaction nasopharyngeal swab was positive for severe acute respiratory syndrome Coronavirus 2. This was initially complicated by pulmonary embolism, apical pneumothorax and pneumomediastinum as a result of ventilation-induced barotrauma. After a four-day intensive care unit (ICU) stay at a local hospital, he developed chest pain with inferior ST-segment elevation and was transferred for percutaneous coronary intervention (PCI).
Coronary angiography revealed smooth vessels, but the right coronary artery demonstrated large thrombus with subtotal occlusion of the distal vessel (Figure 1A, arrow). Thrombectomy was undertaken extracting white and red thrombus. Intravascular ultrasound (IVUS) confirmed the presence of extensive fresh thrombus with minimal atheroma (minimal lumen area 21.7 mm2) and plaque burden of 29% with no evidence of rupture (Figure 1B, arrowheads, Figure 1C). PCI was performed successfully but with residual thrombotic pruning of the distal vessel (Figure 1D). The post-procedural ICU course was complicated by the development of secondary haemophagocytic lymphohistiocytosis (HLH) (ferritin 42,000 ug/L, AST 18,000 IU/L, fibrinogen 3.6 g/L, platelets 91[109/L]), a hyperinflammatory syndrome characterised by fulminant hypercytokinaemia and multiorgan failure for which he required anti-IL-6 therapy with tocilizumab.
We present a case of COVID-19 with extensive thrombus in a coronary artery with minimal atherosclerotic disease. Although plaque erosion cannot be completely ruled out using IVUS, the association of a prothrombotic and hyperinflammatory state with COVID-19, particularly with concomitant HLH, implicates these processes pathophysiologically. In particular, endothelial dysfunction and Von Willebrand factor activation have been observed with COVID-19 infection and may reflect the underlying mechanism1. To our knowledge, this is the first case of COVID-19-related in situ thrombosis imaged using intravascular imaging techniques.
Funding
This work was part funded by a King’s College Hospital R&D Grant and was supported by the Department of Health via a National Institute for Health Research Biomedical Research Centre award to Guy’s & St Thomas’ NHS Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.