A 58-year-old male with hypertension, diabetes mellitus, and a history of smoking was admitted following a four-week history of oppressive chest pain at rest, with episodes lasting up to 20 minutes. His electrocardiogram and serial cardiac biomarkers were within normal limits. However, transthoracic echocardiography revealed hypokinesia in the basal septal and inferior wall regions. Coronary angiography showed mild atheromatosis in the left coronary artery without significant lesions. The right coronary artery (RCA) (Figure 1A, Moving image 1) demonstrated mild irregularities, along with a moderate lesion in the distal segment. Optical coherence tomography (OCT) revealed a fibrolipidic plaque without evidence of rupture or thrombus formation but with macrophage infiltration and images suggestive of layered plaque (Figure 1B, Figure 1C, Moving image 1). A vasospasm test with acetylcholine was subsequently performed. Following the administration of 20 μg of intracoronary acetylcholine, the patient experienced angina with ST-segment elevation, accompanied by the development of a significant stenosis in the distal RCA and an intermediate stenosis in the proximal segment (Figure 1D,
Join us for free and access thousands of articles from EuroIntervention, as well as presentations, videos, cases from PCRonline.com
Sign up for free!
Flashlight
DOI: 10.4244/EIJ-D-24-01086
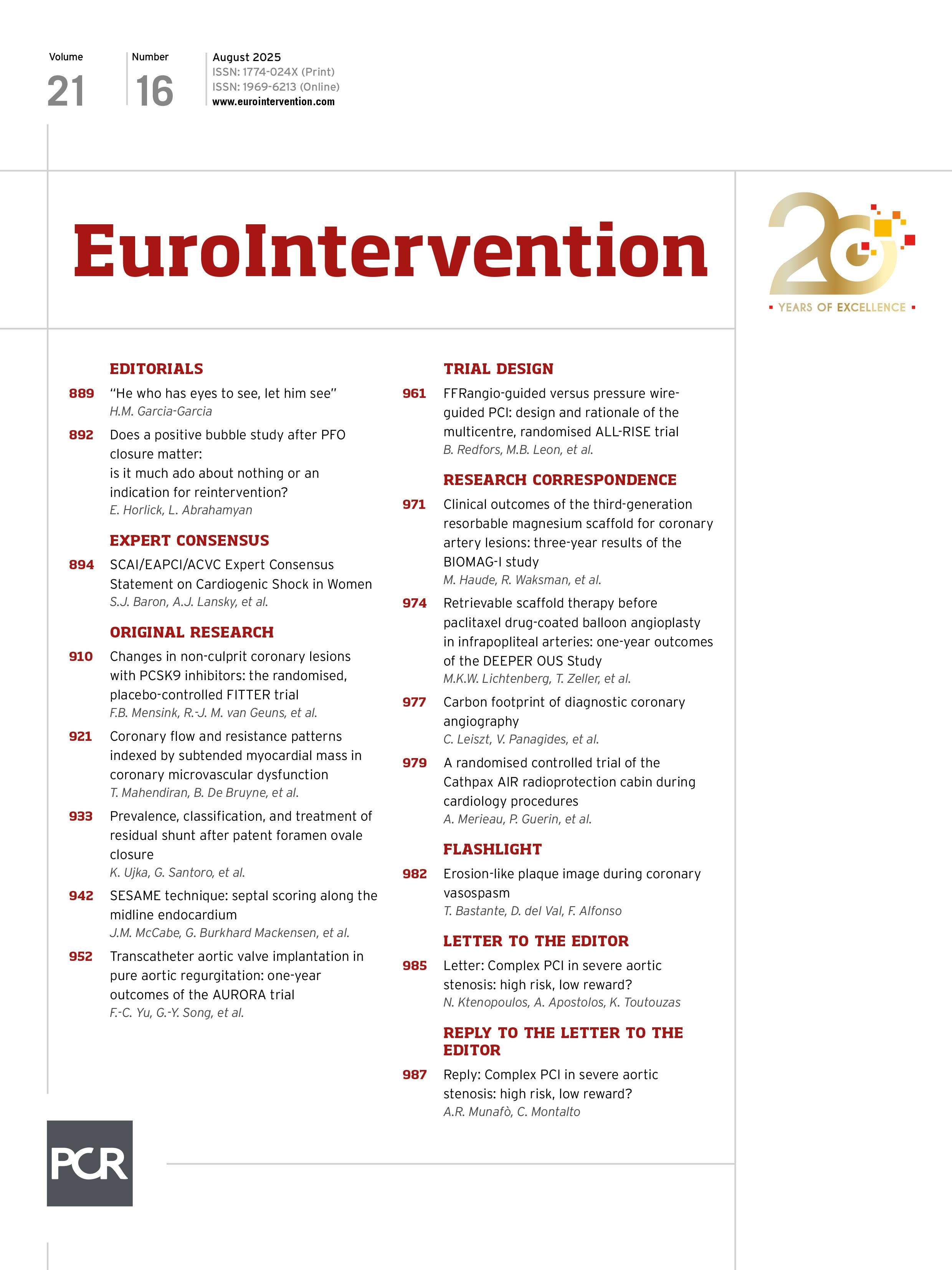
Erosion-like plaque image during coronary vasospasm
No account yet?
You need to subscribe to download this file
×
If you are not yet a subscriber, please subscribe to download this file.
Download citations
×
Select a format
Suggested by Cory
In-stent neoatherosclerosis 10 years after bare metal stent implantation: ruptured vulnerable plaque by optical coherence tomography
A unique feature of thin flat thrombus visualised by optical coherence tomography
Acute myocardial infarction in a young endurance athlete caused by probable plaque erosion
Concertina effect mimicking plaque rupture in a patient presenting with acute coronary syndrome
Near-infrared spectroscopy, optical coherence tomography and angioscopy to unravel the mechanism of very late metallic drug-eluting stent thrombosis
Features of atherosclerosis in patients with angina and no obstructive coronary artery disease
Characteristics and significance of healed plaques in patients with acute coronary syndrome and stable angina: an in vivo OCT and IVUS study
High definition OCT image of sharp calcium spicule
Optical coherence tomography and tailored treatment of in-stent restenosis
IMAGE IN CARDIOLOGY
10.4244/EIJV10I4A83 • Aug 19, 2014
Caixeta A et al
free
10.4244/EIJV9I8A169 • Dec 27, 2013
Kume T et al
free
INTERVENTIONAL FLASHLIGHT
10.4244/EIJ-D-17-00087 • Jun 2, 2017
Colleran R et al
free
Flashlight
10.4244/EIJ-D-25-00333 • Nov 3, 2025
Chandra Mohan N and Johnson T
INTERVENTIONAL FLASHLIGHT
10.4244/EIJ-D-17-00582 • Aug 24, 2018
Ishihara T et al
free
Clinical Research
10.4244/EIJ-D-21-00875 • Aug 5, 2022
Pellegrini D et al
free
Clinical research
10.4244/EIJ-D-18-01175 • Oct 4, 2019
Wang C et al
free
IMAGE IN CARDIOLOGY
10.4244/EIJV10I5A104 • Sep 28, 2014
Garrido E et al
free
Image – Interventional flashlight
10.4244/EIJ-D-20-00507 • Aug 6, 2021
Jia H et al
free