Abstract
Background: An association between atherosclerosis and coronary vasospasm has previously been suggested. However, to date, no conclusive data on the whole spectrum of these disorders have been published.
Aims: This study aimed to define specific morphological features of atherosclerosis in patients with angina and no obstructive coronary artery disease (ANOCA) due to coronary vasospasm.
Methods: From February 2019 to January 2020, we enrolled 75 patients referred to our laboratory for a coronary function test (CFT) due to ANOCA and suspected coronary vasomotor dysfunction. The CFT consisted of an acetylcholine test and a physiology assessment with hyperaemic indexes using adenosine. Patients were divided into two groups according to the presence or absence of coronary vasospasm triggered by acetylcholine (ACH+ and ACH–, respectively). In addition, optical coherence tomography (OCT) was performed to assess the lipid index (LI), a surrogate for lipid area, and the prevalence of markers of plaque vulnerability.
Results: ACH+ patients had a higher LI than ACH- patients (LI: 819.85 [460.95-2489.03] vs 269.95 [243.50-878.05], respectively, p=0.03), and a higher prevalence of vulnerable plaques (66% vs 38%, p=0.04). Moreover, ACH+ patients showed a higher prevalence of neovascularisation compared to ACH- subjects (37% vs 6%, p=0.02) and a trend towards a higher prevalence of all individual markers, in particular thin-cap fibroatheroma (20% vs 0%, p=0.06). No differences were detected between patterns of coronary vasospasm.
Conclusions: The presence of coronary vasospasm, regardless of its phenotype, is associated with higher lipid burden, plaque vulnerability and neovascularisation.
Introduction
Despite the scientific advancements in the diagnosis and management of coronary artery disease (CAD), progress is limited in the field of angina with non-obstructive CAD (ANOCA), an often neglected condition with a high prevalence1 and a significant impact on prognosis and quality of life234.
Among possible causes of ANOCA, coronary vasomotor disorders are prominent and are associated with an increased risk of adverse cardiovascular events56789. Coronary vasospasm represents one of the most important coronary vasomotor disorders. It is a condition mainly related to endothelium-dependent vascular dysfunction, and it can affect both the epicardial vessels (epicardial spasm) or the microcirculation (microvascular vasospasm).
Despite being traditionally considered a merely functional disorder, epicardial vasospasm has been associated with a variable degree of plaque burden and of markers of plaque vulnerability, suggesting an association between atherosclerosis and coronary function disorder10111213. Optical coherence tomography (OCT) has emerged as the preferred method to assess atherosclerotic morphological characteristics, due to its high spatial resolution1314. However, significant variability has been reported in study results, and to date no study has performed a comprehensive analysis of all the different markers of plaque vulnerability in the different types of coronary vasospasm. A better understanding of the underlying anatomic and physiologic features could potentially allow improved risk stratification and tailored treatments.
The aim of the current study was to assess the atherosclerotic burden and morphological characteristics of coronary vasospasm using OCT in ANOCA.
Methods
Study design and population
This single-centre observational study was conducted at the Radboud University Medical Center (Radboudumc) in Nijmegen, the Netherlands, a large tertiary referral centre specialised in patients with persistent angina in the absence of obstructive CAD. Between February 2019 and January 2020, we enrolled all patients undergoing an invasive coronary function test (CFT) for suspected coronary vasomotor dysfunction and we performed OCT to correlate functional and anatomical findings.
In all patients, obstructive CAD had been ruled out before CFT by previous anatomical imaging (coronary angiography or coronary computerised tomography angiography) or non-invasive ischaemia detection. Absence of significant coronary lesions was confirmed by coronary angiography at the beginning of the CFT. The extent and severity of CAD burden upon angiography was quantified with the Gensini score, which was the scoring system of choice due to its ability to stratify the degree of stenosis15. Exclusion criteria for the OCT study were obstructive CAD, previous coronary revascularisation and severe kidney disease (eGFR <30 mL/min). The study was approved by the local institutional ethical review board of the Radboudumc and complies with the Declaration of Helsinki. All patients gave written informed consent to the study and data collection.
Study procedures
A detailed description of the CFT is reported in the Supplementary Appendix 1. Per protocol, all tests focused on the left anterior descending artery (LAD), in accordance with available recommendations16, due to its prognostic relevance, the large territory of distribution and logistical considerations (procedural time, radiation dose and amount of dye). Briefly, after confirming the absence of significant CAD by angiography, we performed a provocative test with increasing doses of acetylcholine (10, 20, 100, 200 µg) in the left coronary artery to detect signs and symptoms of spasm. After the injection of nitrates, a pressure wire was placed in the distal LAD (PressureWire XTM; Abbott) and measurements of resting full-cycle ratio (RFR), fractional flow reserve (FFR), index of microvascular resistance (IMR) and coronary flow reserve (CFR) were performed using dedicated software (CoroFlow software; Coroventis).
OCT procedure analysis
Detailed OCT protocol and definitions are reported in the Supplementary Appendix 2. After CFT, one high-definition OCT run (54 mm, 20 mm/sec) of the LAD was performed (proximal marker in the LAD ostium) with a frequency-domain OCT catheter (Dragonfly Optis; St. Jude Medical). Offline analysis of each OCT pullback was performed by two independent expert reviewers, blinded to the results of the CFT. Disagreements were resolved by a third reviewer. In-depth analysis of cross-sectional images was performed in one frame per millimetre of longitudinal length. Plaque analysis followed international consensus17.
The main variables of interest were the lipid index (LI) (Figure 1), and the presence of vulnerable plaques, defined as plaques presenting at least one marker of vulnerability (presence of a fibroatheroma, macrophage infiltration, neovascularisation or plaque erosion) (Figure 2), both individually and as a composite endpoint. The LI, a surrogate for lipid pool area, was defined as the mean lipid arc (Figure 1A) multiplied by lipid-core longitudinal length18. It was introduced to provide an index of atherosclerotic burden, as light in OCT cannot penetrate lipid-rich plaques due to significant attenuation, and a thorough assessment of plaque burden such as in intravascular imaging would not be possible. Fibroatheroma was defined as a lipid plaque with a maximum lipid arc >90°. Thin-cap fibroatheroma (TCFA) was defined as a fibroatheroma with a cap thickness ≤65 µm (Figure 1B). The individual morphological atherosclerosis characteristics were analysed both on a patient-level (number of patients with at least one OCT frame showing the variable of interest) and on a frame-level (extension of those variables in terms of number of millimetres indexed per total length of plaque segments) (Figure 1C).
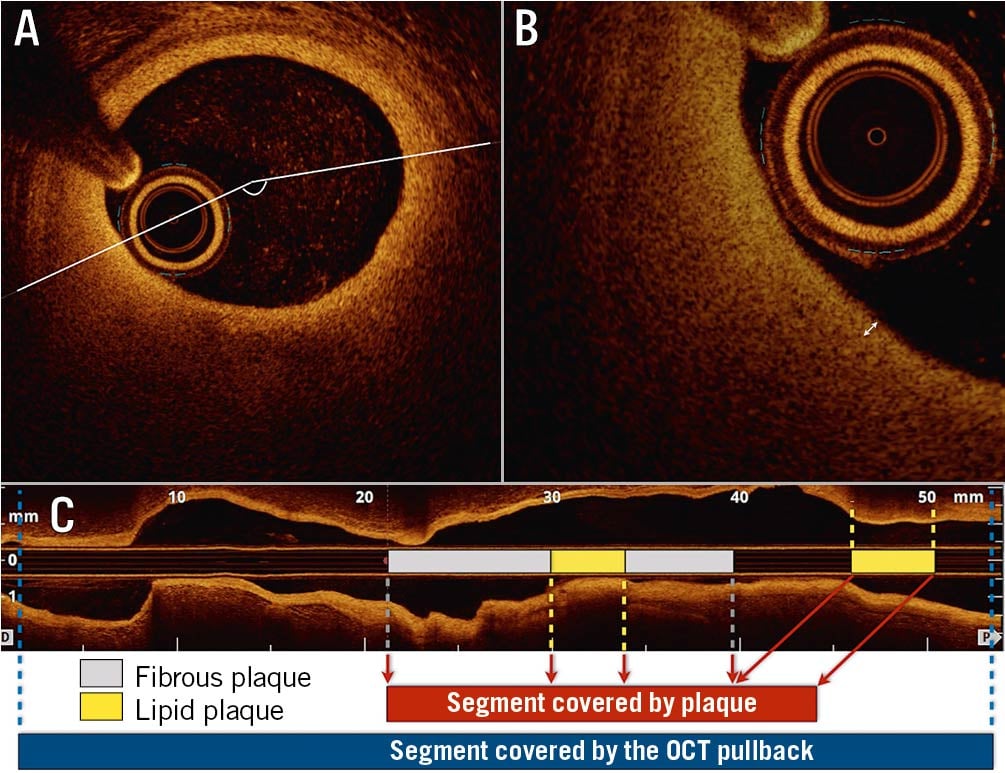
Figure 1. Representation of lipid pool analysis. A) Lipid angle, (B) thickness of the fibrous cap and (C) longitudinal extension. After frame-by-frame analysis, the total amount of plaque along the scanned segment was computed. Then, in the total segment covered by plaque, the extension of each plaque component was calculated. OCT: optical coherence tomography

Figure 2. Examples of plaque vulnerability markers detected with optical coherence tomography (OCT). A) Fibroatheroma (asterisks), shown as a lipid plaque with an angle >90°. The bright fibrous cap at the top of the plaque, when ≤65 µm, defines the presence of a thin-cap fibroatheroma. B) Macrophage infiltration (arrowheads), shown as bright spots with significant attenuation, in the context of a lipid plaque. C) Erosion (asterisks), shown as irregular endothelium with overlying thrombus. D) Neovascularisation (arrowheads), shown as small vascular structure in the context of the plaque, without connections with the lumen.
Definitions
We defined the presence or absence of coronary vasospasm (either epicardial or microvascular spasm) according to an intracoronary acetylcholine (ACH) test result (ACH+ vs ACH-), in line with current guidelines1619. Epicardial spasm was defined as a focal or diffuse epicardial coronary diameter reduction ≥90% in response to ACH, compared to the relaxed state after the intracoronary nitroglycerine infusion, with reproduction of both recognisable symptoms and ischaemic ECG changes. Microvascular spasm was defined as the reproduction of recognisable symptoms and ischaemic ECG changes, in the absence of ≥90% epicardial diameter reduction during ACH infusion. Ischaemic electrocardiogram (ECG) changes were defined as transient ST-segment elevation or depression of ≥0.1 mV, or ischaemic T-wave changes in at least two contiguous leads. Impaired microvascular dilatation was defined by a CFR <2.0, an IMR ≥25, or a combination of both.
Statistical analysis
Continuous variables are presented as mean±standard deviation or as median (interquartile range [IQR]), as specified. After testing for normal distribution, comparisons were performed using the unpaired t-test, and the Mann-Whitney U test or Kruskal-Wallis test, as appropriate. Categorical variables are presented as counts and percentages (%). Comparisons were performed using Pearson’s χ2 or Fisher’s exact test. A two-sided p-value <0.05 was considered statistically significant. All statistical analyses were performed with JMP v.14.0 (SAS Institute).
Results
Baseline characteristics and flow parameters
From February 2019 to January 2020, 83 patients underwent a CFT at our institution. Of these, 75 patients met the eligibility criteria and were enrolled in the study.
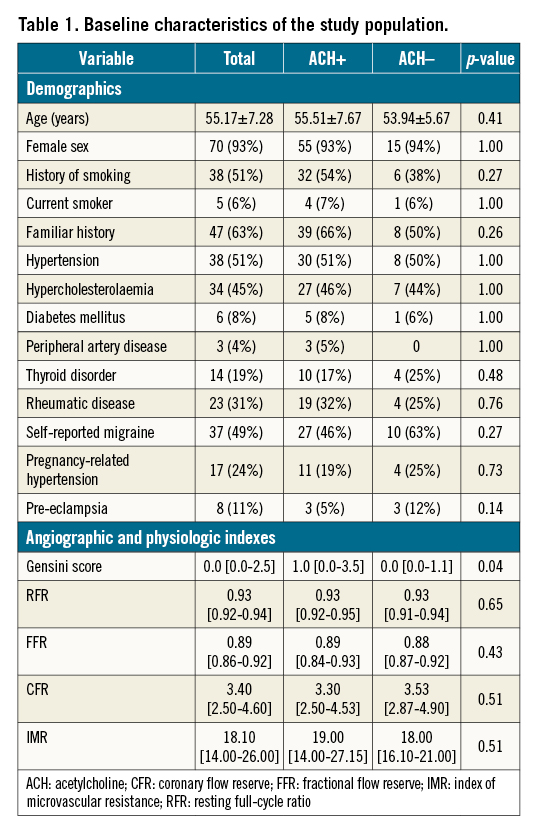
Baseline characteristics are reported in Table 1. The study population was composed almost entirely of women (93%) with a mean age of 55 years and a moderate cardiovascular risk profile. As per protocol, significant CAD had been ruled out either by previous coronary angiography (50 subjects, 67% of the population), coronary computerised tomography angiography (37 subjects, 49%) or non-invasive ischaemia detection test (50 subjects, 67%). Before CFT, coronary angiography confirmed the absence of significant stenoses. No cases of FFR or RFR below the ischaemic threshold were recorded.
Overall, there were no fatal or serious non-fatal complications related to the performance of CFT or OCT.
An abnormal reaction to acetylcholine (ACH+) occurred in 59 patients (79%), with 28 patients having epicardial spasm and 31 patients having microvascular spasm. Baseline clinical characteristics were similar between ACH+ and ACH- patients (Table 1). At angiography, coronary artery disease burden was very low, and ACH+ patients had a significant, yet clinically non-relevant, increase compared to ACH- patients (Gensini score 1 and 0, respectively, p=0.04). Of the patients with vasospasm, 23 (39%) had coexistent impaired microvascular dilatation as measured by adenosine, compared to three subjects in the ACH- group (19%). Twelve individuals (16%) had a negative CFT.
Three patients did not undergo an adenosine test due to drug contraindications (severe asthma) and could not perform a complete physiology evaluation (only resting indexes were measured). Resting and hyperaemic flow indexes were within the normal range, and no differences were detected between the groups (Table 1).
OCT analyses
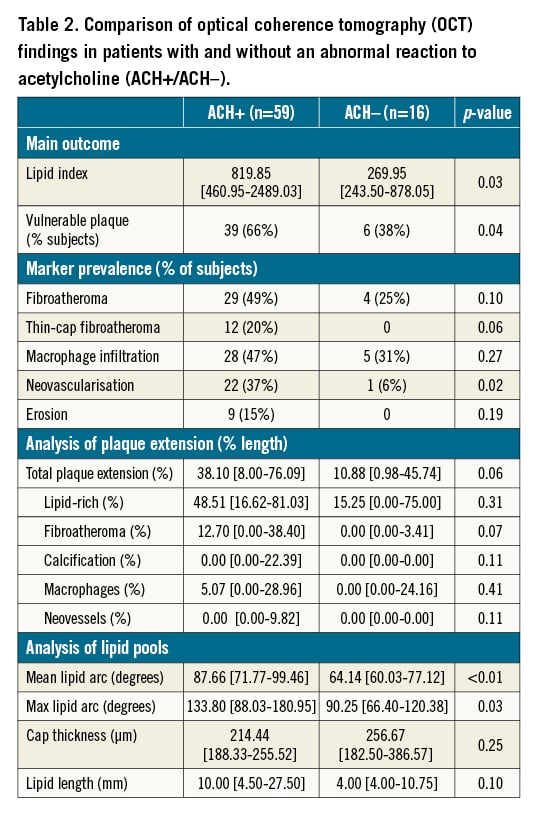
ACH+ patients had a significantly higher LI than ACH- patients (819.85 vs 269.95, respectively, p= 0.03) (Table 2, Central illustration), due to a significant increase in mean lipid angle (87.66° vs 64.14°, respectively, p<0.01). Furthermore, total plaque extension tended to be higher; in ACH+ patients, 38.10% of all frames were covered by plaque, as compared with 10.88% in ACH- patients (p=0.06). In the ACH+ group, the prevalence of vulnerable plaque markers was significantly higher than in the ACH- group (66% vs 38%, p=0.04), led by a higher, yet non-significant, rate of TCFA (20% vs 0%, p=0.06) and a significant increase in neovascularisation (37% vs 6%, p=0.02) No differences were recorded in the prevalence and extension of the other markers of plaque vulnerability. No correlations were identified between the variables of interest and baseline characteristics or flow parameters. In particular, exploratory analyses found no correlations between atherosclerosis and CFR/IMR values.

Central illustration. Graphical representation of the study. Upper row: result of the acetylcholine test, showing either an angiographically normal artery (A) or a diffuse epicardial vasospasm (B). Middle row: optical coherence tomography assessment was performed, to detect normal segments (C) or coronary plaques, and to evaluate the lipid index and the presence of markers of plaque vulnerability. D) an example of a thin-cap fibroatheroma. Lower row: study results. Vessels prone to vasospasm were associated with a higher lipid index (E) and a higher prevalence of vulnerable plaques (F). ACH: acetylcholine; ANOCA: angina with no obstructive coronary artery disease; OCT: optical coherence tomography
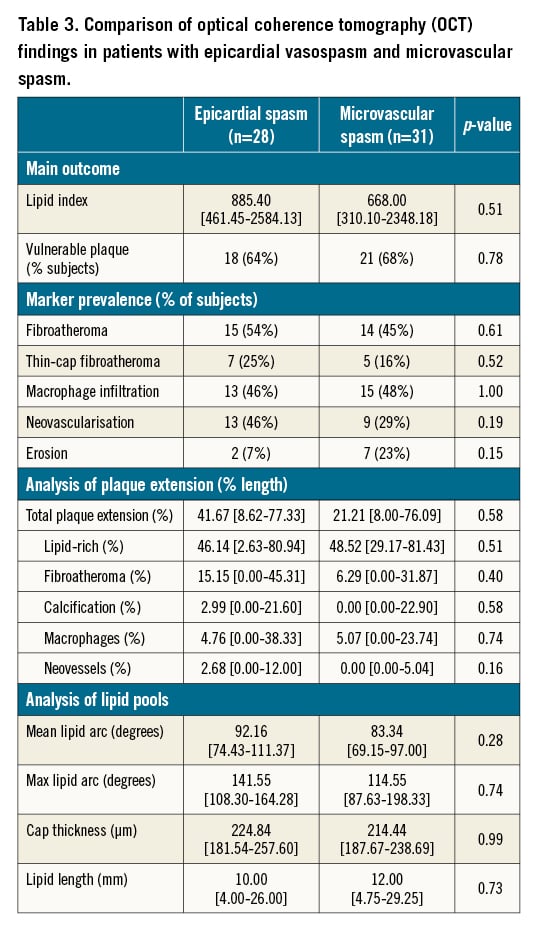
A comparison was performed between patients with microvascular spasm and epicardial spasm (Table 3), also showing no major differences in terms of LI (668.00 [310.10-2348.18] vs 885.40 [461.45-2582.13], respectively, p=0.51) and in terms of markers of plaque vulnerability (overall rate of 64% and 68% in patients with epicardial and microvascular spasm, respectively, p=0.78).
Finally, in an exploratory analysis of the subgroup of patients with epicardial spasm, LI was compared between subjects with focal and diffuse epicardial spasm, yielding non-significant differences (982.25 vs 885.40, respectively, p=0.52).
Discussion
In this study of patients with ANOCA undergoing CFT and OCT we obtained three major findings. First, patients with vasospasm elicited by acetylcholine (either epicardial or microvascular spasm) had more advanced atherosclerosis compared to patients without vasospasm. Second, patients with coronary vasospasm had more characteristics of plaque vulnerability compared to patients without vasospasm. Third, there were no differences in terms of disease extension and morphology between patients with epicardial and microvascular spasm.
Associations between vasomotor dysfunction and atherosclerosis
Patients with coronary vasospasm showed more advanced atherosclerosis compared to those without vasospasm. Although isolated reports have addressed similar hypotheses in specific phenotypes of vasomotor disorders (mainly vasospastic angina), to our knowledge this is the first study to analyse the full spectrum of vasomotor dysfunction. Despite conflicting reports in the last decades, with earlier studies suggesting that spasm may be associated with mild atherosclerosis1220, our data support recent OCT and near-infrared spectroscopy (NIRS) studies1011 demonstrating that epicardial spasm may be associated with more advanced atherosclerosis, even in the absence of obstructive CAD. In our study, in vessels prone to vasospasm, atherosclerotic plaques were both more extensive (38% of the assessed segment was covered by plaque, compared to 11% in ACH- vessels, p=0.06), and more prone to rupture (66% of ACH+ patients had at least one marker of plaque vulnerability, compared to 38% of ACH- group, p=0.04). Considering individual markers, the prevalence of neovascularisation was increased in arteries with vasospasm, in agreement with previous experience2122, and a consistent trend towards a higher rate was identified in all other variables2123, particularly in TCFA (20% vs 0%, p=0.06).
We found no correlations between physiology indexes and markers of plaque vulnerability. This is in contrast with the study by Usui and colleagues24, which reported a positive correlation between IMR and markers of plaque severity, regardless of other indexes. However, this study was performed in the setting of angiographically moderate-severe lesions, and the generalisability of these results in the setting of ANOCA is questionable and needs additional evidence.
Macrophage infiltration, which has been suggested as a risk factor for plaque progression and rupture2125, was similar between those with and without vasospasm. We considered macrophages in the setting of lipid-rich plaques, as suggested by consensus documents, due to lack of validation studies in non-lipidic plaques17.
However, exploratory analyses that also considered bright spots outside lipid-rich plaques led to similar results. Additional data are needed to draw additional conclusions on the role of this marker of plaque inflammation.
Another interesting finding is related to intraplaque neovascularisation. This marker was detected in 37% of ACH+ patients, with a higher prevalence compared to ACH- patients (6%, p=0.02). A possible association between neovessels and spasm has been questioned, as the dysfunctional endothelium of these vessels may trigger the paradoxical reaction to acetylcholine, through an impaired nitric oxide pathway21. We were able to reproduce this finding. However, it is noteworthy that the study by Choi and colleagues considered a combination of intraplaque neovessels and vasa vasorum. We decided to include only intraplaque vessels in the analysis. These develop in reaction to the growth of the lipid pool, triggered by ischaemia and inflammation, and may be a better expression of such a deranged physiology. The role of vasa vasorum in our study is, therefore, not known.
Our results seem to support the theory that coronary vasospasm is not only a functional disorder, but is associated with more advanced atherosclerotic disease. These data may also explain the higher rate of ischaemic adverse events reported by recent studies on this population5678. Indeed, the prognostic value of high-risk plaque characterisation by OCT was confirmed by the recent CLIMA study26, which found cap thickness <75 µm, lipid arc >180° and macrophage infiltration to be associated with a higher risk of adverse cardiovascular events at one year. Interestingly, low cap thickness resulted in the single strongest risk factor. In our study, despite the use of an even stricter cut-off (<65 µm), this marker was found in 20% of subjects with coronary vasospasm.
If confirmed in a larger series, these findings may have an impact on the management and treatment of patients with coronary vasospasm, who usually show a low to moderate cardiovascular risk profile and receive drug therapy only to control symptoms (mainly calcium channel blockers and nitrates), with no significant benefit in terms of prognosis. There is still widespread belief that coronary vasomotor dysfunction is a relatively benign condition, and this evaluation bias (i.e., the false belief that, if there is no angiographic stenosis, there is no significant atherosclerosis) may also lead to an underestimation of future events and, therefore, to a decreased level of awareness and insufficient clinical monitoring over time. CFT proved to be effective at better defining the vasomotor dysfunction phenotype and optimising drug therapy27. The addition of anatomic information might provide additional prognostic value, which would in turn set the goal of treatment on harder outcomes, beyond simple symptom control. Current consensus documents focus on lifestyle factors and behavioural interventions, comparable to patients with CAD. With regard to risk factor management, ACE inhibitors and statins are recommended4. With regard to aspirin and anti-inflammatory therapy directed at atherosclerosis, no clear recommendations are available. We hypothesise that this medication might be beneficial in vasospastic ANOCA patients.
Relationships between microvascular and epicardial spasm
The definition of microvascular spasm is based on the absence of visible severe epicardial spasm in the setting of typical chest pain and ECG changes triggered by acetylcholine28. Currently, the Coronary Vasomotion Disorders International Study Group (COVADIS) lists microvascular spasm in the group of conditions called microvascular angina, along with impaired microvascular dilatation. The latter is considered an endothelium-independent vascular dysfunction and includes impaired vasodilatory capacity and increased microvascular resistance (marked by an abnormal CFR and/or IMR values4). Although all these conditions may cause disturbed functioning of the microcirculation, in our study, microvascular spasm shared significant similarities with epicardial spasm, particularly in terms of plaque distribution and composition. Understanding the mutual relationships between these conditions, either in terms of temporal evolution or spatial distribution, would provide interesting insights. Indeed, microvasculature may present the same features of dysfunctional endothelium and inflammation that were found in the epicardial arteries. Pro-inflammatory mediators produced in the larger vessels may also affect the downstream vasculature. The current diagnostic criteria define epicardial vasospasm as severe dynamic stenosis upon angiography, so all those abnormal reactions to acetylcholine which do not fulfil this strict criterion fall into the group of microvascular spasm, regardless of the degree of epicardial stenosis, if any. As a consequence, the concomitant existence of epicardial and microvascular vasospasm is not considered; so it is not possible to understand whether overlapping syndromes may exist, the evolution of these patterns over time, and whether specific triggers may elicit different spastic reactions in the same individual.
Unfortunately, no comparison with available evidence is possible, as studies focusing on microvascular spasm are lacking, and these results should be considered as hypothesis-generating. Moreover, there is still a lack of evidence in subjects with abnormal CFR/IMR values. Additional data may provide insights on morphological differences and similarities between these conditions, with the potential for further refinements of current classifications and risk stratification.
Limitations
This is a single-centre study, on a small sample of individuals. A larger population may allow additional comparisons, as well as a higher statistical power, especially for the analysis of markers of plaque vulnerability and for additional comparisons with non-vasospastic microvascular dysfunction. The study population included mostly women; although a higher prevalence in the female sex is expected in the field of vasomotor disorders, the generalisability to male sex may be limited.
Finally, we followed standard assessment protocols for the acquisition and interpretation of OCT images, and relied on multiple, independent assessments to limit variability. Nevertheless, a certain degree of inter- and intra-operator variability in the measurements must be taken into account.
Conclusions
Coronary vasospasm triggered by an abnormal reaction to acetylcholine is associated with a higher degree of atherosclerosis, a higher prevalence of vulnerable plaques and a higher rate of neovascularisation. Different patterns of vasospasm (focal, diffuse, or microvascular) are not associated with differences in intracoronary findings.
Impact on daily practice
Coronary vasospasm, regardless of its pattern, is associated with more advanced atherosclerotic disease, both in terms of plaque extension and of plaque vulnerability, compared with non-spastic vessels. Thus, patients with coronary vasospasm may have a higher risk of adverse cardiovascular events compared to the general population. This may allow identification of high-risk groups and improve long-term prognosis through the early adoption of strict management of cardiovascular risk factors and close follow-up.
Conflict of interest statement
P. Damman has received consultancy and lecture fees from Philips and Abbott. R.E. Konst, N. van Royen and S.E. Elias-Smale have received a research grant from Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.