Abstract
Background: Intracoronary provocation testing with acetylcholine (ACh) is crucial for the diagnosis of functional coronary alterations in patients with suspected myocardial ischaemia and non-obstructive coronary arteries.
Aims: Our intention was to assess the safety and predictive value for major adverse cardiovascular and cerebrovascular events (MACCE) in patients presenting with ischaemia with non-obstructive coronary arteries (INOCA) or with myocardial infarction with non-obstructive coronary arteries (MINOCA).
Methods: We prospectively enrolled consecutive INOCA or MINOCA patients undergoing intracoronary ACh provocation testing.
Results: A total of 317 patients were enrolled: 174 (54.9%) with INOCA and 143 (45.1%) with MINOCA. Of these, 185 patients (58.4%) had a positive response to the ACh test. Complications during ACh provocative testing were all mild and transient and occurred in 29 (9.1%) patients, with no difference between patients with positive or negative responses to ACh testing, nor between INOCA and MINOCA patients. A history of paroxysmal atrial fibrillation, moderate/severe diastolic dysfunction and a higher QT dispersion at baseline electrocardiogram were independent predictors of complications. MACCE occurred in 30 patients (9.5%) during a median follow-up of 22 months. The incidence of MACCE was higher among patients with a positive ACh test (24 [13.0%] vs 6 [4.5%], p=0.017), and a positive ACh test was an independent predictor of MACCE.
Conclusions: ACh provocation testing is associated with a low risk of mild and transient complications, with a similar prevalence in both INOCA and MINOCA patients. Importantly, ACh provocation testing can help to identify patients at higher risk of future clinical events, suggesting a net clinical benefit derived from its use in this clinical setting.
Introduction
Coronary vasomotor disorders, both at the microvascular and epicardial level, have been shown to be responsible for myocardial ischaemia in a sizeable group of patients undergoing coronary angiography (CAG). The clinical manifestations range from ischaemia with non-obstructive coronary arteries (INOCA) to myocardial infarction with non-obstructive coronary arteries (MINOCA), or life-threatening arrhythmias and sudden cardiac death1234. Intracoronary provocation testing with administration of acetylcholine (ACh) at the time of CAG may elicit epicardial coronary spasm or microvascular spasm in susceptible individuals and, therefore, is of paramount importance in the diagnosis of functional coronary alterations in patients with suspected myocardial ischaemia and non-obstructive coronary artery disease (CAD)567. However, these studies were mainly focused on patients with INOCA, whilst MINOCA patients were often underrepresented89. Indeed, intracoronary provocation testing is still underused in clinical practice10, probably because of concerns about the risk of complications, especially in an acute clinical setting11. Therefore, there is a paucity of studies that evaluate both the safety and the prognostic value of this test in a large study population. Consequently, the net clinical benefit deriving from the use of this test in clinical practice remains unknown. Furthermore, there are no studies assessing the safety and the prognostic relevance of this test according to acute (MINOCA) or stable (INOCA) clinical presentations.
Thus, in our study, we aimed to assess the safety of ACh provocation testing, evaluating the prevalence, predictors and the prognostic role of complications that occur during this test across the entire clinical spectrum of patients with myocardial ischaemia and non-obstructive CAD. At the same time, we also aimed to assess the role of intracoronary ACh provocation testing in stratifying the prognosis of these patients.
Methods
Study population
We prospectively enrolled consecutive patients admitted to the Department of Cardiovascular Sciences of Fondazione Policlinico Universitario A. Gemelli IRCCS in Rome, Italy, undergoing clinically indicated CAG for suspected myocardial ischaemia with angiographic evidence of non-obstructive CAD (angiographically normal coronary arteries or diffuse atherosclerosis with stenosis <50% and/or fractional flow reserve [FFR] >0.80) and undergoing an intracoronary provocation test with ACh from September 2015 to December 2019.
We enrolled patients admitted with both suspected INOCA and MINOCA, diagnosed according to the most recent European Society of Cardiology (ESC) guidelines51213. Among patients presenting with suspected MINOCA, we excluded those with obvious causes of myocardial infarction (MI) other than suspected coronary vasomotor abnormalities (Supplementary Appendix 1).
Clinical, laboratory and echocardiographic characteristics of all included patients were collected at admission (Supplementary Appendix 2, Supplementary Appendix 3). The study protocol complied with the Declaration of Helsinki, and the study was approved by our Institutional Review Committee. All patients gave written informed consent to CAG and provocation tests.
Coronary angiography and invasive provocation test protocol
CAG was performed through the radial or femoral artery approach. Intracoronary ACh provocation testing was performed immediately after CAG as previously described4, with a slow rate of manual infusion over a period of 3 minutes, and a “stepwise approach” with a 2-3 minute interval between injections (20-50-100 mcg in the left coronary artery [LCA] and 20-50 mcg in the right coronary artery). The decision to further proceed with testing the LCA with a 200 mcg dose was left to the operator’s discretion. CAG was performed 1 minute after each injection and/or when chest pain and/or ischaemic electrocardiogram (ECG) shifts were observed.
The test was considered positive for epicardial coronary spasm in the presence of 1) focal or diffuse epicardial coronary diameter reduction ≥90% in comparison to the relaxed state following intracoronary nitroglycerine administration given to relieve the spasm; 2) reproduction of the patient’s symptoms; and 3) ischaemic ECG shifts14. Microvascular spasm was diagnosed when typical ischaemic ST-segment changes and angina developed in the absence of epicardial coronary constriction (<90% diameter reduction)15 (Supplementary Appendix 4)1415.
Assessment of complications during intracoronary provocation tests
Complications occurring during intracoronary provocation testing with ACh were defined as the composite of bradyarrhythmia (asystole or second/third-degree atrioventricular [AV] block lasting more than 3 s), paroxysmal/persistent atrial fibrillation (AF)/supraventricular tachycardia (SVT), ventricular tachycardia (VT), ventricular fibrillation (VF), and all-cause death. In addition, the individual incidence of each complication was recorded.
Clinical outcomes and follow-up
Major adverse cardiovascular and cerebrovascular events (MACCE) were defined as the composite of cardiovascular (CV) death, non-fatal MI, hospitalisation due to unstable angina (UA), and stroke/transient ischaemic attack (TIA). We only counted the first occurrence of MACCE during the follow-up period (Supplementary Appendix 5).
All patients underwent a 24-hour ECG recording after discharge (median 11 months, interquartile range [IQR] 10-12). Occurrence of arrhythmic events was defined as the composite of non-sustained/sustained VT, persistent/permanent AF or any grade of AV block requiring pacemaker implantation. In addition, the individual occurrence of each arrhythmic event was also recorded.
We also recorded any episodes of angina (requiring hospitalisation or not) during the follow-up period and collected the Seattle Angina Questionnaires (SAQ) summary score at 12 months16. All patients received clinical follow-ups by telephone interview and/or clinical visits at 6, 12, 24, 36, 48 and 60 months.
Statistical analysis
Data distribution was assessed according to the Kolgormonov-Smirnov test. Continuous variables were compared using the unpaired Student’s t-test or Mann–Whitney U-test, as appropriate, and data were expressed as mean±standard deviation (SD) or as median IQR. Categorical data were evaluated using the X2 test or Fisher's exact test as appropriate. A value of p<0.05 was considered significant. A multivariable logistic regression analysis for the occurrence of complications during intracoronary positive test was performed including all variables with a p-value<0.05 at univariate analysis. Univariable Cox regression analysis was applied to assess the relation of individual variables with MACCE. Cox regression was then applied to identify variables independently associated with MACCE; to this end, we included in the multivariable model only variables showing p≤0.05 at univariable analysis. All analyses were performed using SPSS version 21 (IBM Inc.).
Results
Baseline characteristics of study population
We enrolled 317 patients (mean age 60.5±11.9 years; 177 [55.8%] women) with myocardial ischaemia and non-obstructive coronary arteries undergoing ACh provocation testing. Among them, 174 (54.9%) patients presented with INOCA and 143 (45.1%) with MINOCA.
A positive response to ACh testing was observed in 185 (58.4%). Among the patients with a positive ACh test, 119 (64.3%) developed an epicardial spasm, whereas 66 (35.7%) developed a microvascular spasm. Patients with a positive provocation test, compared to patients with a negative test, had a higher prevalence of grade II or III diastolic dysfunction (29 [15.7%] vs 7 [5.3%], respectively; p=0.004), a lower maximal dose of ACh administered during the test as well as a lower percentage of patients who received a high ACh dose ≥100 mcg (103 [55.7%] vs 92 [69.7%]; p=0.011). Of note, patients with a positive ACh test, compared to those with a negative response, received calcium channel blockers (CCBs) more frequently (174 [94.1%] vs 50 [37.9%], p<0.001) and statins (153 [82.7%] vs 66 [50.0%], p<0.001) as therapy at discharge (Supplementary Table 1).
OCCURRENCE OF COMPLICATIONS DURING ACh INTRACORONARY PROVOCATION TESTING
Complications during ACh testing occurred in 29 (9.1%) patients: 20 (6.3%) patients developed a transient bradyarrhythmia, 8 (2.5%) had paroxysmal/persistent AF/SVT, 1 (0.03%) sustained VT and 1 (0.03%) VF treated with prompt defibrillation. One patient experienced both transient bradyarrhthmias and paroxysmal AF. No deaths were observed.
Patients who developed complications during ACh testing, compared with those who didn’t, more frequently had a previous history of paroxysmal AF (11 [37.9%] vs 17 [5.9%], p<0.001) and a higher prevalence of left ventricle (LV) diastolic dysfunction (24 [82.8%] vs 171 [59.4%]; p=0.014), in particular, grade II or III diastolic dysfunction (9 [31.0%] vs 27 [9.4%], p<0.001). Of note, there were no significant differences between the two groups regarding therapy on admission, the maximal dose of ACh administered during the test, as well as the percentage of patients who received a high ACh dose (≥100 mcg) (all p>0.05). Of interest, there were no differences in the rate of complications between patients with a positive response to ACh testing and patients with a negative response to testing (18 [9.7%] vs 11 [8.3%]; p=0.671), nor between MINOCA and INOCA patients (13 [9.1%] vs 16 [9.2%]; p=0.974) (Supplementary Figure 1) or the dose of ACh administered (18.4% at 20 mcg, 8.3% at 50 mcg, 7.5% at 100 mcg, 11.1% at 200 mcg; p=0.201) (Supplementary Figure 2).
Moreover, at baseline ECG, patients who developed complications had a higher QT dispersion (40.5 msec [35-53.75] vs 31.0 msec [25-41], p<0.001) compared with those who didn’t. Clinical, electrocardiographic, echocardiographic and angiographic features of the overall study population and the occurrence of complications during the provocation test are shown in Table 1.
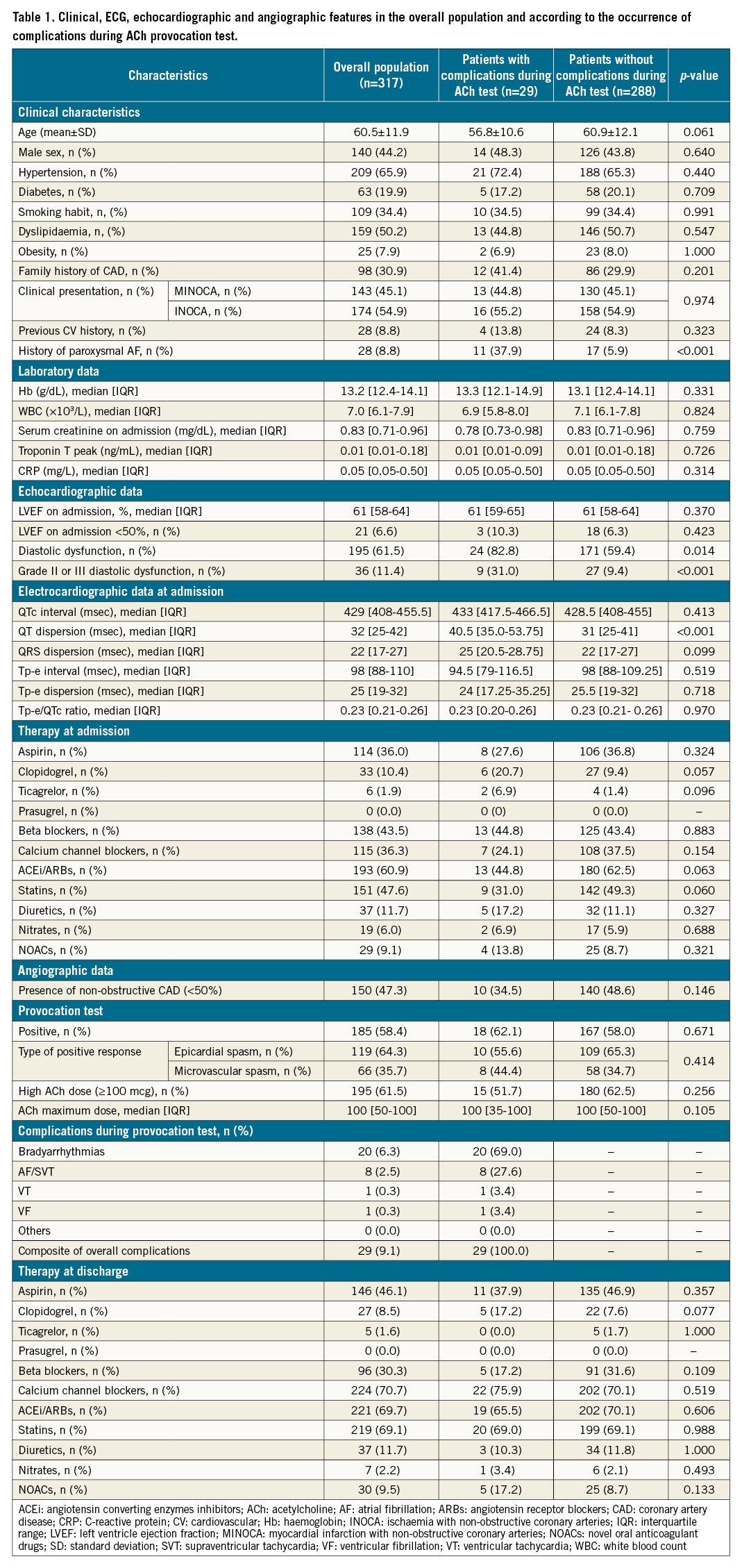
PREDICTORS OF COMPLICATIONS DURING ACh PROVOCATION TESTING
In the univariate logistic regression analysis, a previous history of paroxysmal AF (odds ratio [OR] 9.74, 95% confidence interval [CI]: 3.98-23.86, p<0.001), diastolic dysfunction (OR 3.28, 95% CI: 1.22-8.85; p=0.019), in particular grade II-III diastolic dysfunction (OR 4.35, 95% CI: 1.80-10.50; p=0.001), and QT dispersion at baseline ECG (OR 1.01, 95% CI: 1.00-1.03; p=0.034) were predictors of complications during ACh provocation testing. In the multivariate logistic regression analysis, only a previous history of paroxysmal AF (OR 11.56, 95% CI: 4.32-30.91, p<0.001), grade II-III diastolic dysfunction (OR 3.50, 95% CI: 1.20-10.24; p=0.022), and a higher QT dispersion at baseline ECG (OR 1.02, 95% CI: 1.01-1.03; p=0.021) were independent predictors of complications during intracoronary provocation testing (Table 2).
CLINICAL OUTCOMES ASSOCIATED TO THE OCCURRENCE OF COMPLICATIONS DURING ACh PROVOCATION TESTING
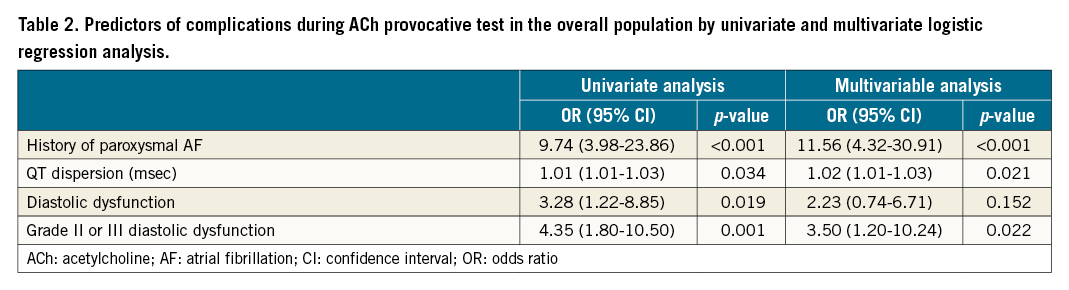
At a median follow-up of 22 months (IQR 13-32 months), MACCE occurred in 30 (9.5%) patients. Of note, there were no differences in the rate of MACCE whether or not there were complications during ACh testing (4 [13.8%] vs 26 [9.0%]; p=0.488, respectively), with no difference in the individual endpoints of CV death, non-fatal MI, hospitalisation for angina or cerebrovascular events (Supplementary Table 2). Moreover, there were no significant differences in the incidence of arrhythmic events detected during the 24-hour ECG recording at 12-month follow-up (6 [20.7%] vs 57 [19.8%]; p=0.695, respectively) as well as for the individual incidence of non-sustained/sustained VT, permanent AF and any grade AV block requiring pacemaker implantation (Figure 1).
Figure 1. Clinical outcomes according to the occurrence of complications during ACh provocation test. A. Incidence of composite of MACCE and individual components of MACCE at follow-up according to the occurrence of complications during an ACh provocation test. B. Incidence of composite of arrhythmic events and individual components of arrhythmic events at follow-up according to the occurrence of complications during an ACh provocation test. C. SAQ summary score at follow-up according to the occurrence of complications during an ACh provocation test. ACh: acetylcholine; AF: atrial fibrillation; AV: atrioventricular; CV: cardiovascular; IQR: interquartile range; MACCE: major adverse cardiovascular and cerebrovascular event; MI: myocardial infarction; SAQ: Seattle Angina Questionnaire; TIA: transient ischaemic attack; UA: unstable angina; VT: ventricular tachycardia
In addition, no significant differences were found between the 2 groups regarding the recurrence of angina (9 [31.0%] vs 63 [21.9%]; p=0.418) and SAQ summary score at 12-month follow-up (84 [IQR 74; 88] vs 82 [IQR 78; 88]; p=0.571) (Supplementary Table 2).
Finally, comparisons of the Kaplan–Meier curves by log-rank test showed no differences between the 2 groups regarding MACCE-free survival (p=0.488) (Figure 2A).
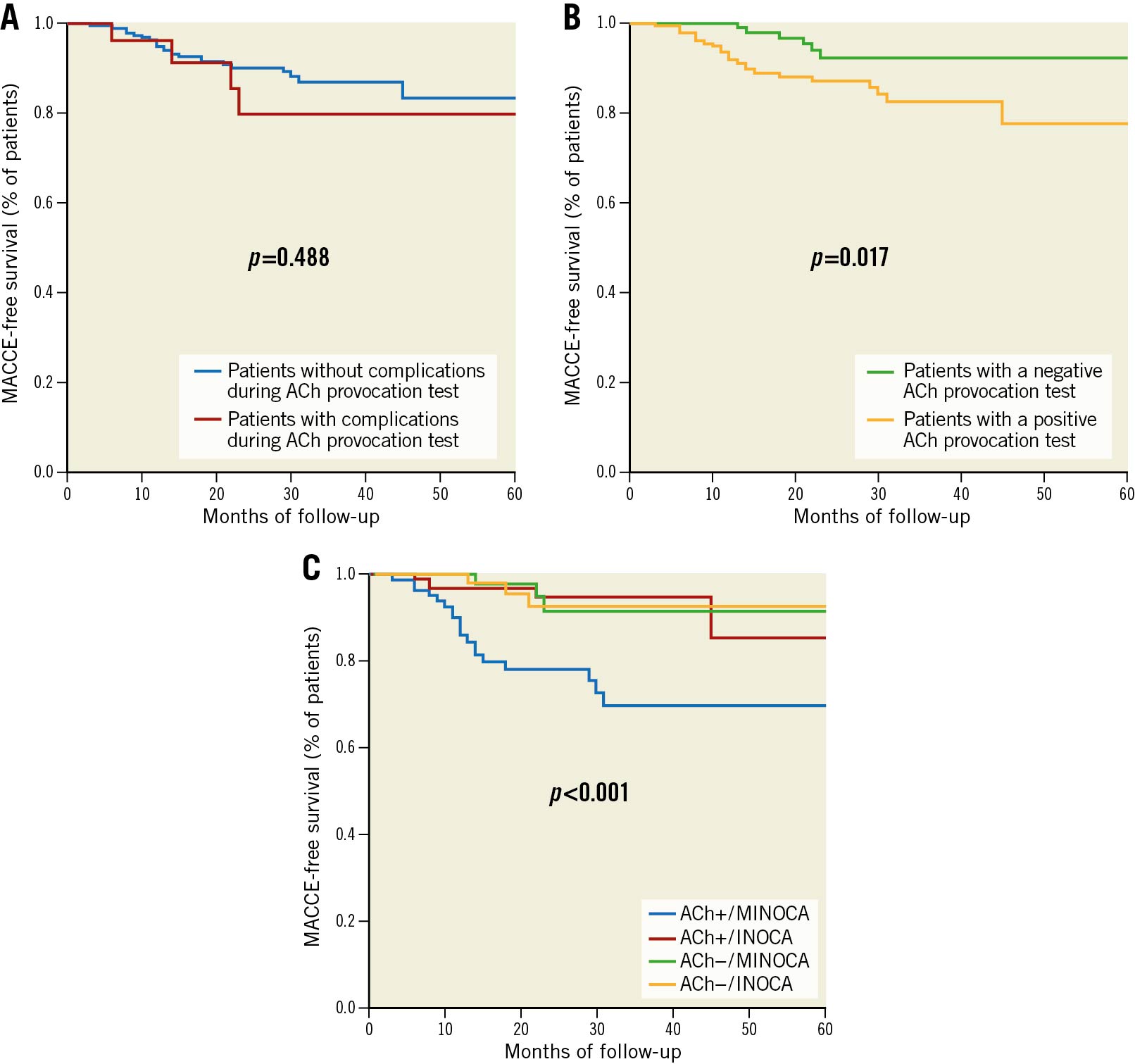
Figure 2. Survival analysis. A. Survival Kaplan–Meier curve for MACCE according to the occurrence of complications during an ACh provocation test. B. Survival Kaplan–Meier curve for MACCE according to a positive or negative ACh invasive provocation test. C. Survival Kaplan–Meier curve for MACCE according to clinical presentation (MINOCA vs INOCA) and response to provocation test (positive vs negative). Curves are compared by the log-rank test. ACh: acetylcholine; INOCA: ischaemia with non-obstructive coronary arteries; MACCE: major adverse cardiovascular and cerebrovascular event; MINOCA: myocardial infarction with non-obstructive coronary arteries
Clinical outcomes according to provocation test response
The incidence of MACCE was higher among patients with a positive ACh test compared to patients with a negative test (24 [13.0%] vs 6 [4.5%]; p=0.017), mainly driven by a higher rate of hospitalisation for UA (16 [8.6%] vs 4 [3.0%]; p=0.049), without differences in the incidence of CV death (1 [0.5%] vs 0 [0.0%]; p=0.397), non-fatal MI (5 [2.7%] vs 1 [0.8%]; p=0.226) and cerebrovascular events (3 [1.6%] vs 1 [0.8%]; p=0.520). Moreover, patients with a positive ACh provocation test experienced a higher rate of recurrent angina compared to those with a negative response (58 [31.4%] vs 14 [10.6%], p<0.001), and the SAQ summary score at 12-month follow-up was lower in patients with a positive test (82 [IQR 75.5-88] vs 84 [IQR 78-88]; p=0.022) (Supplementary Table 3, Figure 3).
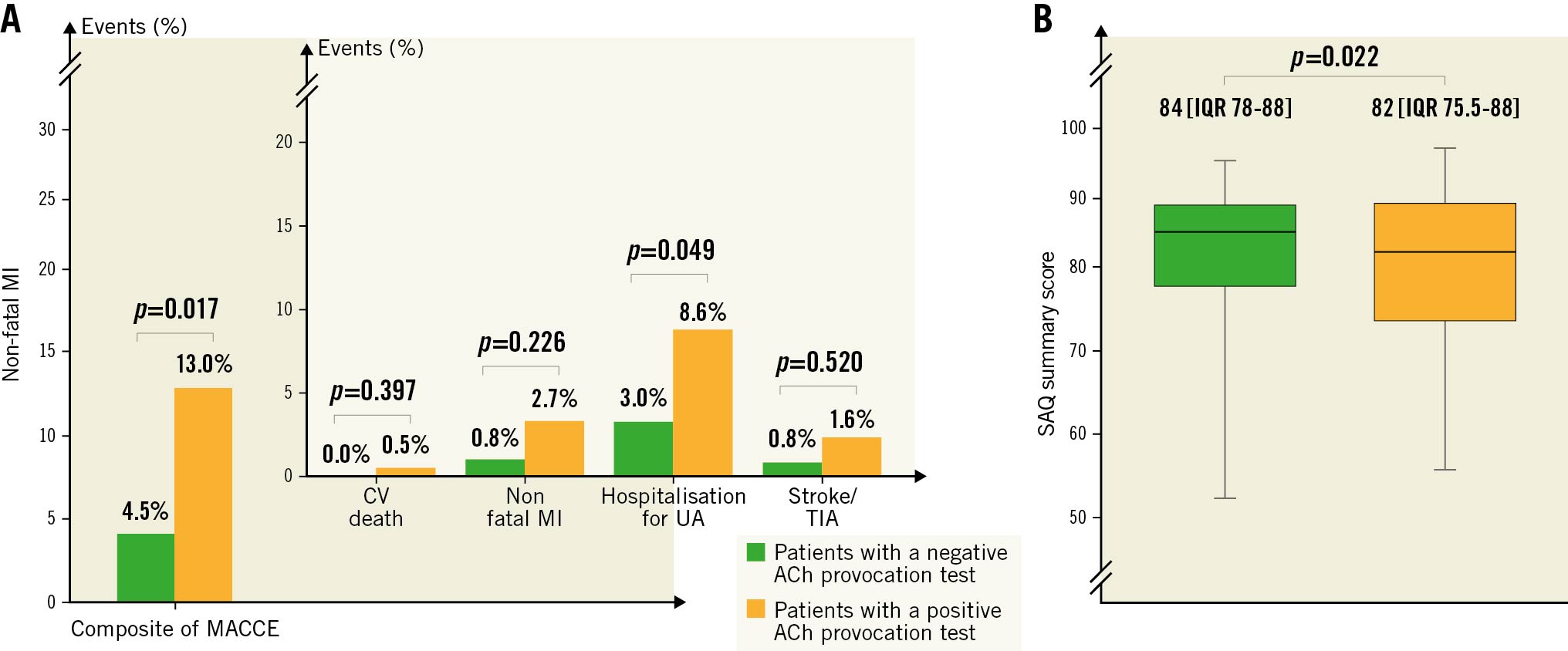
Figure 3. Clinical outcomes according to provocation test response. A. Incidence of composite of MACCE and individual components of MACCE at follow-up according to a positive or negative ACh invasive provocation test. B. SAQ summary score at follow-up according to a positive or negative ACh invasive provocation test. ACh: acetylcholine; CV: cardiovascular; IQR: interquartile range; MACCE: major adverse cardiovascular and cerebrovascular event; MI: myocardial infarction; SAQ: Seattle Angina Questionnaire; TIA: transient ischaemic attack; UA: unstable angina
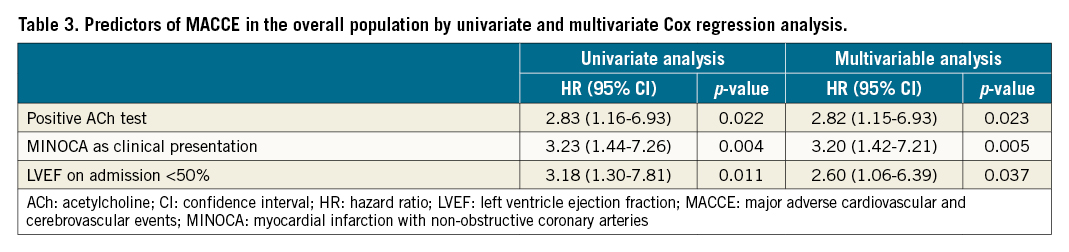
Predictors of MACCE in the overall population
In the univariate Cox regression analysis, a positive ACh test (hazard ratio [HR] 2.83, 95% CI: 1.16-6.93; p=0.022), MINOCA as clinical presentation (HR 3.23, 95% CI: 1.44-7.26; p=0.004) and left ventricle ejection fraction (LVEF) on admission <50% (HR 3.18, 95% CI: 1.30-7.81; p=0.011) were the only predictors for the occurrence of MACCE. In multivariate analysis, a positive ACh test (HR 2.82, 95% CI: 1.15-6.93; p=0.023), MINOCA as clinical presentation (HR 3.20, 95% CI: 1.42-7.21; p=0.005) and LVEF on admission <50% (HR 2.60, 95% CI: 1.06-6.39; p=0.037) remained independent predictors for the occurrence of MACCE in the overall population (Table 3). Comparisons of the Kaplan–Meier curves by log-rank test showed that patients with a positive ACh test had a lower MACCE-free survival (p=0.017) (Figure 2B).
Clinical outcomes according to provocation test response and clinical presentation
In a subgroup analysis according to clinical presentation, the incidence of MACCE among patients presenting with MINOCA was higher compared to patients with INOCA (22 [15.4%] vs 8 [4.6%]; p=0.003), mainly driven by a higher rate of hospitalisation for UA (15 [10.5%] vs 5 [2.9%]; p=0.009). Moreover, patients presenting with MINOCA experienced a higher rate of recurrent angina compared to those with a negative response (43 [30.1%] vs 29 [16.7%]; p=0.018) (Supplementary Table 4).
Furthermore, among MINOCA patients, the incidence of MACCE among patients with a positive ACh test was higher compared to patients with a negative test (19 [22.6%] vs 3 [5.1%]; p=0.006), mainly driven by a higher rate of hospitalisation for UA (13 [15.5%] vs 2 [3.4%]; p=0.021) and with a lower SAQ summary score at follow-up (80 [IQR 74-86] vs 84 [IQR 78-88]; p=0.028) (Supplementary Table 5). On the other hand, among INOCA patients, the incidence of MACCE did not differ between patients with a positive test compared to patients with a negative test (5 [5.0%] vs 3 [4.1%]; p=0.937), as well as the SAQ summary score at follow-up (82 [IQR 77.5-88] vs 84 [IQR 78-90]; p=0.242) (Supplementary Table 6).
In MINOCA patients, in the univariate Cox regression analysis a positive ACh test (HR 4.69, 95% CI: 1.39-15.88; p=0.013) was the only predictor for the occurrence of MACCE (Supplementary Table 7), while in INOCA patients, in the univariate Cox regression analysis an LVEF <50% at admission (HR 9.22, 95% CI: 2.16-39.38; p=0.003) was the only predictor for the occurrence of MACCE (Supplementary Table 8).
Finally, we performed comparisons of the Kaplan–Meier curves by log-rank test according to clinical presentation (MINOCA vs INOCA) and response to provocation testing (positive vs negative), showing that patients with MINOCA and a positive ACh test had the lowest MACCE-free survival, representing the group with the worst prognosis (p<0.001) (Figure 2C).
Discussion
This study represents, to the best of our knowledge, the largest study evaluating both the safety and the prognostic relevance of invasive coronary provocation testing in patients with stable myocardial ischaemia or MI and non-obstructive coronary arteries. It is the first to identify the predictors and the prognostic value of complications occurring during the provocation test and, at the same time, to clarify the role of this test for prognostic stratification in these patients.
The main results of our study can be summarised as follows: 1) the overall rate of complications during ACh provocation testing was rather low (9.1%), with no difference between INOCA or MINOCA patients or between patients with a positive or a negative test response; 2) previous history of paroxysmal AF, moderate-to-severe LV diastolic dysfunction and higher QT dispersion at baseline ECG were the only predictors for the occurrence of complications during the test; 3) the occurrence of complications during intracoronary ACh testing was not associated with a worse prognosis at a medium- to long-term follow-up; 3) a positive ACh test portended worse clinical outcomes, mainly due to a higher rate of rehospitalisation for UA; 4) a positive ACh response predicted a worse prognosis in MINOCA but not INOCA patients.
Our results are in line with previous evidence9171819 reporting low rates of complications in patients undergoing intracoronary provocation testing in experienced centres. We previously showed in 80 MINOCA patients that invasive provocation testing for spasm is safe and identifies a high-risk subset of patients in terms of clinical endpoints and quality of life4. Recently Probst et al9 reported the safety data of ACh provocation testing in 180 patients with myocardial ischaemia and non-obstructive CAD. No irreversible events were observed, and overall transient arrhythmic complications occurred in 28 (16%) patients, with no differences between INOCA and MINOCA.
Of interest, in our study we did not find any differences in the rate of arrhythmic complications between patients with a positive or negative ACh test, suggesting that the mechanisms that underlie the occurrence of these complications are probably linked to a direct arrhythmogenic effect of ACh rather than being consequent to ACh-induced myocardial ischaemia. Indeed, we demonstrated that the presence of an increased QT dispersion may predispose the development of complications, suggesting that a baseline inhomogeneity of repolarisation may increase the susceptibility to arrhythmias (i.e., a transient exacerbation of QT dispersion due to ACh effect). Accordingly, Suzuki et al20 demonstrated that patients with vasospastic angina had a higher QT dispersion that was associated with the occurrence of ventricular arrhythmias during provocation tests for spasm, and Kaski et al21 reported that an increased QT dispersion in patients with vasospastic angina was associated with a higher rate of cardiac arrest and syncope. The non-uniform effects of ACh on ventricular endocardial and epicardial action potential might accentuate QT dispersion22 and favour the occurrence of provocation-related arrhythmic events, which, however, might also be further favoured by the induction of ischaemia23.
In addition, a history of paroxysmal AF predicted the occurrence of complications during the test in our patients, in agreement with previous data24. Indeed, a previous episode of AF often implies the presence of a latent electrical instability in the atrial myocardium252627 which can be triggered by ACh due to its shortening effects on atrial refractory period. Interestingly, the presence of grade II or III LV diastolic dysfunction, which might be related to higher pressure in the left atrium and therefore may enhance the electrical arrhythmogenic effects of ACh, also predicted the occurrence of complications during ACh testing2829.
Of importance, we demonstrated that at medium- to long-term follow-up there were no differences in the rate of MACCE between patients experiencing complications compared to those without complications during ACh testing, as well as of arrhythmic events in the 24-hour ECG recording, angina recurrence and the SAQ summary score. Thus, these data can reassure patients and clinicians about the lack of consequences of testing-related events in their clinical outcome. On the other hand, these results should encourage cardiologists to perform provocation testing whenever the presence of a coronary vasomotor disorder is suspected. Indeed, we demonstrated that performing an ACh provocation test has relevant prognostic implications, as patients with a positive test have a higher risk of MACCE at follow-up. Of note, we showed for the first time that the prognostic relevance of a positive provocation test seems to be restricted to MINOCA patients, while for INOCA patients a positive ACh test does not predict a worse clinical outcome (Central illustration). Explanations for these findings are multiple. Indeed, MINOCA patients compared to INOCA have a higher number of events at follow-up, probably due to the more aggressive functional alterations underlying the occurrence of myocardial ischaemia. This point may explain why a provocation test can be more useful in stratifying the prognosis in MINOCA than in INOCA patients. In addition, even though a positive provocation test did not predict the prognosis in INOCA, a tailored therapy was started based on the results of the ACh test, and this may per se improve the outcome in these patients30.
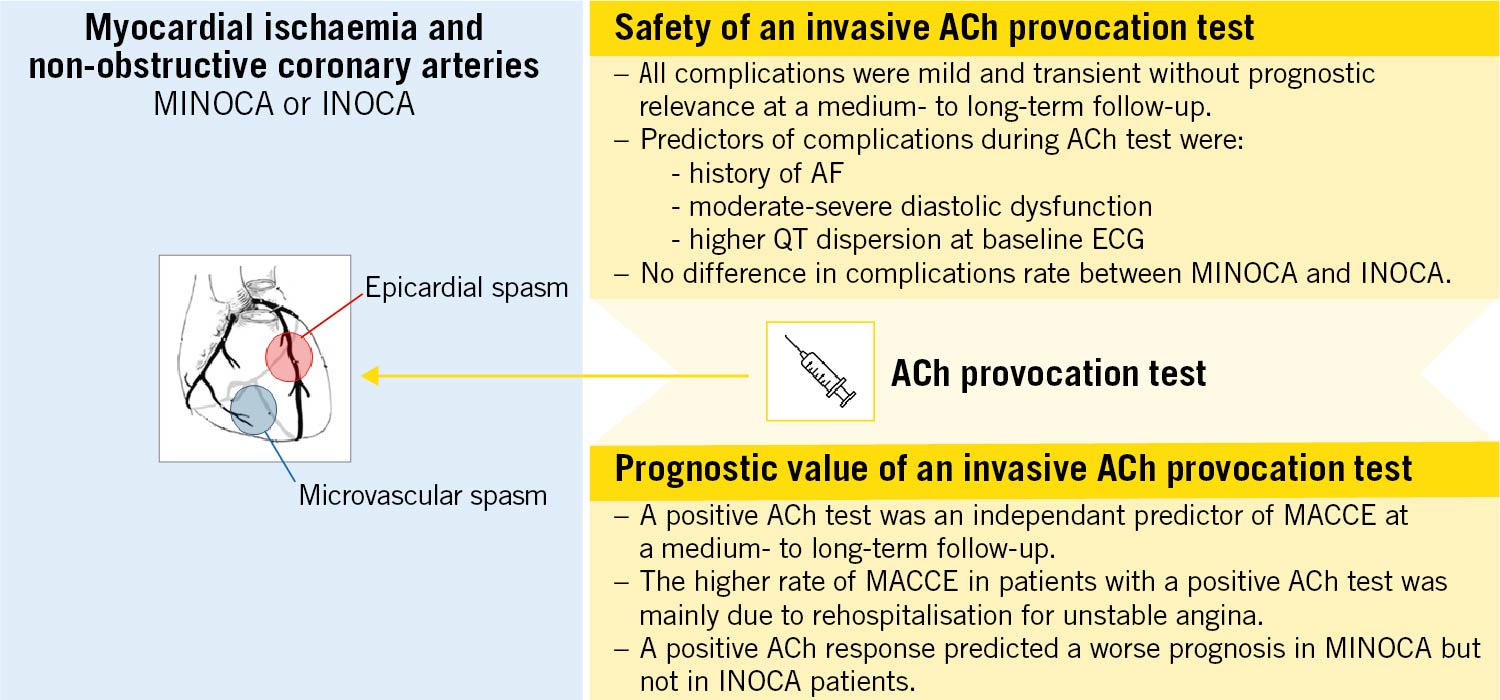
Central illustration. Safety and prognostic value of an invasive ACh provocation test. ACh: acetylcholine; AF: atrial fibrillation; ECG: electrocardiogram; INOCA: ischaemia with non-obstructive coronary arteries; MACCE: major adverse cardiovascular and cerebrovascular event; MINOCA: myocardial infarction with non-obstructive coronary arteries
Study limitations
Some limitations of our study should be acknowledged. First, this is a single-centre study. Second, the definition of arrhythmic complications at follow-up has the limit of using a single 24-hour ECG recording, thus likely underestimating the real arrhythmic burden of these patients. Third, we did not invasively measure coronary blood flow and coronary flow reserve and resistance during the invasive study; thus, their potential relationship with the response to vasoconstrictor stimuli remains undetermined. Moreover, we did not assess the presence of endothelial dysfunction at the lowest dose of ACh and its relation to outcomes, potentially confounding the relation between spasm and MACCE. However, MACCE mainly occurred in patients whose ACh test was positive for spasm, while the event rate in patients with an ACh negative response was very low. This suggests that coronary spasm may represent a major determinant for the prognosis of these patients. Fourth, in MINOCA patients taking vasoactive drugs, the provocation tests were not performed after a washout period for CCB and nitrates, potentially interfering with the result of the test. Fifth, the choice to administer the highest dose of ACh for the LCA (200 mcg) was left to the operator’s discretion. Finally, the choice to perform a provocation test, especially in patients presenting with stable angina, was left to the operator’s discretion. This could have resulted in a selection bias and could explain why the prevalence of MINOCA patients in our study population was higher compared with previous studies.
Conclusions
In conclusion, performing an ACh provocation test in patients with myocardial ischaemia and non-obstructive coronary arteries is safe with a low rate of complications, with no differences between INOCA and MINOCA patients. Moreover, our study identified the presence of paroxysmal AF, moderate/severe diastolic dysfunction, along with QT dispersion, as predictors of complications during intracoronary provocation testing with ACh, helping clinicians to select those patients requiring particular attention during the test. Finally, the demonstration that complications during the ACh test are not associated with a worse prognosis at follow-up may reassure clinicians for post-discharge management. In addition, showing that performing an ACh test can help stratify the prognosis, especially in MINOCA patients, may suggest the presence of a net clinical benefit deriving from its use and supports the decisions of national drug regulatory agencies to approve the use of this test in routine clinical practice.
Impact on daily practice
Performing an acetylcholine provocation test in patients with myocardial ischaemia and non-obstructive coronary arteries is safe with a low rate of complications, with no differences between patients presenting with INOCA or MINOCA. A history of paroxysmal atrial fibrillation, moderate/severe diastolic dysfunction, along with QT dispersion, are predictors of complications during intracoronary provocation testing with acetylcholine, helping clinicians to select patients who require particular attention during the test. Performing an acetylcholine provocation test can help in stratifying the prognosis, especially in MINOCA patients, as patients with a positive test have a higher risk of MACCE at follow-up. These results may suggest the presence of a net clinical benefit deriving from its use.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.