For many years, the management of patients with acute or chronic coronary syndromes has been impeded by a one-dimensional vision of myocardial ischaemia, namely the presence of epicardial vessel obstruction. Overall, diagnostic uncertainty prevailed when, in patients with chest pain or abnormal electrocardiograms (ECG), ischaemia tests or cardiac biomarkers, the coronary arteriogram failed to reveal obstructive epicardial disease.
Luckily, we may have reached a tipping point in considering an alternative origin of myocardial ischaemia in these patients, both in terms of evidence and interest from the medical community123. The acronyms INOCA and MINOCA, which refer to ischaemia or myocardial infarction of non-obstructive origin, respectively, are now widely used in the current literature. The European Association of Percutaneous Cardiovascular Interventions (EAPCI) Expert Consensus Document on INOCA was the most downloaded article from EuroIntervention in 20211, and recent European Society of Cardiology (ESC) guidelines support the use of intracoronary testing to assess vasomotor and microvascular disorders in INOCA and MINOCA23.
Yet, we anticipate an uneven adoption of the recommended tools for the diagnosis of non-obstructive coronary disease by cardiologists. Although the use of intracoronary guidewires to measure coronary flow reserve (CFR) and microvascular resistance (MR) is simple and intuitive, many physicians are reluctant to perform an intracoronary acetylcholine (ACh) test to assess coronary vasomotor disorders. There are multiple reasons for this, but the predominant one is concern over the safety and the clinical value of the test. Addressing these concerns is important because, in contrast to CFR, which can be measured non-invasively, an objective diagnosis of vasomotor disorders can only be achieved by coronary ACh testing1. As the CorMiCa (CORonary MICrovascular Angina) Trial showed, establishing whether the ischaemia has a vasomotor or structural origin is key to devising an effective stratified medical treatment4. In other words, proper diagnosis of INOCA needs two legs to stand on (Figure 1): namely, the assessment of 1) structural remodelling that may impair microvascular conductance, and 2) vasomotor disorders affecting epicardial vessels or arterioles.
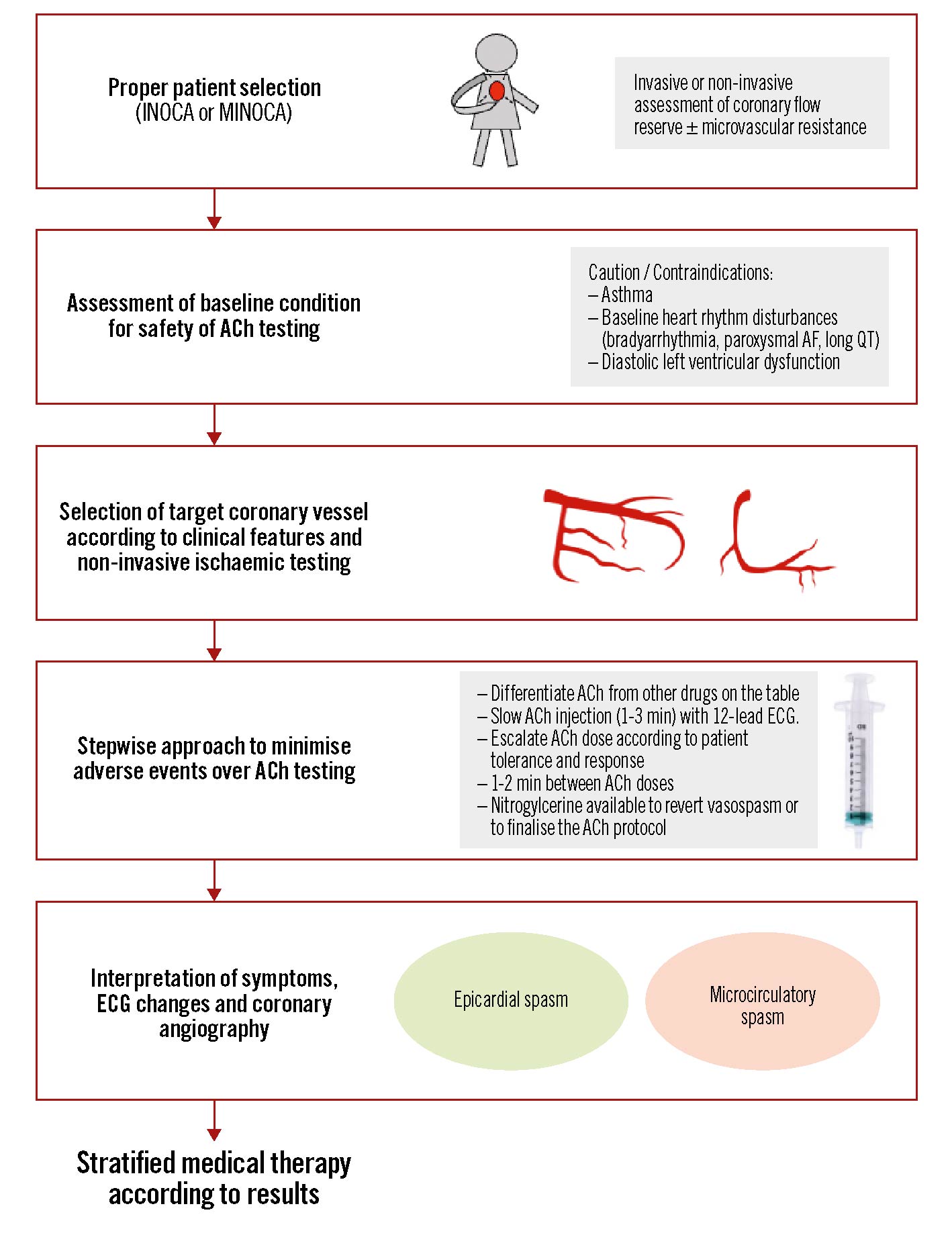
Figure 1. Stepwise approach to assess the coronary microcirculation and vasomotor disorders in patients with non-obstructive coronary artery disease. ACh: acetylcholine; AF: atrial fibrillation; ECG: electrocardiogram; INOCA: ischaemia with non-obstructive coronary arteries; MINOCA: myocardial infarction with non-obstructive coronary arteries
It is in this context that EuroIntervention publishes in this issue a timely article by Montone et al on the safety and prognostic information of ACh testing in clinical practice5. The study is based on a large patient cohort (n=317), prospectively studied with a median follow-up of 22 months. Of note, both patients with INOCA and MINOCA were included. We should state upfront that the main caveat of the study is that CFR and MR were not measured in INOCA patients, and, therefore, the management of these patients does not mirror current recommendations or trial-based evidence12. Yet, the findings are of relevance in reassuring the medical community on the safety and prognostic value of the ACh test.
In this study, there were no deaths related to the test, and the development of life-threatening ventricular arrhythmias was extremely low (0.03% for either ventricular tachycardia or ventricular fibrillation). Atrial fibrillation (AF) or supraventricular tachycardia developed in 2.5% of cases, and transient bradyarrhythmias in 6.3% of cases. The authors found no relationship between the development of ACh-related transient arrhythmias and a worse long-term prognosis. An important piece of information is the link between a history of prior AF and the development of arrhythmias during ACh testing. As a matter of fact, previous studies have identified endothelial dysfunction as a predictor of future AF6. Most cases of AF that develop during ACh testing revert spontaneously, and pharmacological or electrical cardioversion is rarely needed. Also, patients with left ventricular diastolic dysfunction and higher baseline QT dispersion were identified as being prone to developing arrhythmias during the test.
Regarding the prognostic value of ACh testing, these findings should be interpreted in the context of the study design. Since there was no control group, we cannot gauge the benefit of test-based medical treatment in vasomotor disorders compared to non-guided treatment. But we learned that enrolled patients with a positive ACh test, who were discharged on calcium channel blockers, statins and angiotensin-converting enzyme inhibitors, presented with a mean Seattle Angina Questionnaire (SAQ) summary score of 82/100 at follow-up, which, overall, suggests an acceptable level of therapeutic success. It remains unknown whether the SAQ summary score would have been even higher if a more personalised pharmacological treatment, based not only on the ACh test but also on CFR and MR values as currently recommended12, had been set up.
In terms of prognostic information, three independent predictive factors for major adverse cardiac and cerebrovascular events (MACCE) were identified in a multivariate analysis: a positive ACh test, MINOCA as a clinical presentation, and left ventricular ejection fraction (LVEF) <50% on admission. A subgroup analysis revealed a higher incidence of MACCE in patients with MINOCA, compared to those with INOCA. These findings highlight the prognostic implications of vasomotor disorders disclosed by ACh testing in patients who subsequently received pharmacological treatment of coronary vasospasm: the latter consideration is important as we might expect a higher incidence of events if a diagnosis leading to specific treatment had not been reached. Regarding the worse prognosis associated with MINOCA presentation, it remains plausible that in MINOCA, which is a much more heterogenous condition than INOCA (despite the similarity in acronyms), coronary spasm may not always be the primary cause of the syndrome but an epiphenomenon of widespread underlying derangements at a coronary, myocardial or systemic level. In any case, this study revealed that patients with MINOCA at clinical presentation and a positive response to ACh portended the group with the worst prognosis at follow-up, highlighting the clinical relevance of ACh testing in this specific clinical setting.
In summary, we anticipate that the study by Montone et al will help to dissipate fears about the safety of ACh testing in patients with non-obstructive coronary disease syndromes and, also, highlight its prognostic value in chronic and acute presentations. Most cardiologists already feel comfortable using wire-based tools to measure CFR and MR. Incorporating ACh testing into routine clinical practice will enable them to perform a comprehensive diagnosis of vascular dysfunction mechanisms accounting for myocardial ischaemia and, ultimately, improve the quality of life and prognosis of patients: proper diagnosis in INOCA and MINOCA needs two legs to stand on.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.