Abstract
Aims: Recent studies have demonstrated favourable clinical outcomes for the everolimus-eluting bioresorbable vascular scaffold (BVS) ABSORB™ in patients with stable coronary artery disease. There are currently no data on its use in patients with ST-segment elevation myocardial infarction (STEMI). We assessed the safety and impact of BVS in the setting of primary percutaneous coronary intervention (PCI) in patients presenting with STEMI to our institution.
Methods and results: A total of 11 patients who underwent primary PCI with intent for BVS implantation between October 2012 and April 2013 at our institution were included. Median follow-up period was 53.0±45.9 days. One patient presented to the hospital with cardiogenic shock and subsequently died. The other 10 patients did not have any major adverse cardiac events (MACE). There were no acute or subacute stent thromboses at short-term follow-up.
Conclusions: These are the first real-world data using BVS in patients with STEMI. The ABSORB™ BVS may be safely used in patients with STEMI undergoing primary PCI with favourable short-term outcome.
Introduction
In recent large-scale trials second-generation drug-eluting stents (DES), in particular everolimus-eluting stents (EES), have been shown to have better clinical outcomes and safety when compared to paclitaxel-eluting stents1,2. However, problems associated with a permanent polymer and scaffold remain and this has led to efforts to develop a fully bioresorbable vascular scaffold. Recent studies have demonstrated favourable clinical outcomes for the everolimus-eluting bioresorbable vascular scaffold (BVS) compared with conventional metallic drug-eluting stents in patients with stable coronary artery disease3,4. However, the use of BVS in patients with ST-segment elevation myocardial infarction (STEMI) has not been reported other than in isolated case reports. We therefore assessed the safety and impact of BVS in the setting of primary percutaneous coronary intervention (PCI) in patients with STEMI.
Methods
Eleven patients who underwent primary PCI with intent for BVS, ABSORB™ (Abbott Vascular, Santa Clara, CA, USA) implantation between October 2012 and April 2013 at the National University Heart Centre, Singapore, were included. These patients were considered for BVS implant outside of a specified study protocol when the device became commercially available as of the 25th September 2012. The patients considered for BVS implant were generally younger and the procedure was performed by operators with prior experience in its use. Because of the increased cost of this novel device, only patients with appropriate insurance and financial means were considered. Dual antiplatelet therapy was started at presentation to the emergency department in all patients as per our institution protocol. Patients were evaluated for the development of major adverse cardiac events (MACE) defined as cardiac death, myocardial infarction, and target vessel revascularisation, during the period of follow-up at routine clinic visits after one month and by telephone consultations. Written informed consent was obtained from all patients as per our institution’s requirement. Discrete data were presented as frequencies and/or percentages, and continuous variables were presented as median or mean±SD.
Results
The patient characteristics are detailed in Table 1. Mean age was 49.5±10.9 years and 81.8% were male. The transradial approach was used in 90.9% of cases. Primary PCI was successfully performed in all patients using a 6 Fr guide catheter with initial thrombus aspiration without in-catheterisation laboratory complications. Median follow-up period was 53.0±45.9 days. One patient presented to the hospital with cardiogenic shock. This patient was found collapsed outside the hospital and bystander CPR was performed. On arrival in the emergency department an electrocardiogram (ECG) showed ST-elevation in V1-4. After intubation and stabilisation of haemodynamics, PCI with BVS was successfully performed. In spite of inotropic support and therapeutic hypothermia, the patient’s condition did not improve and he subsequently died two days after presentation. The other 10 patients did not have any MACE during the period of follow-up (median 53 days, range of 12 to 158 days). There were no acute or subacute stent thromboses on follow-up.
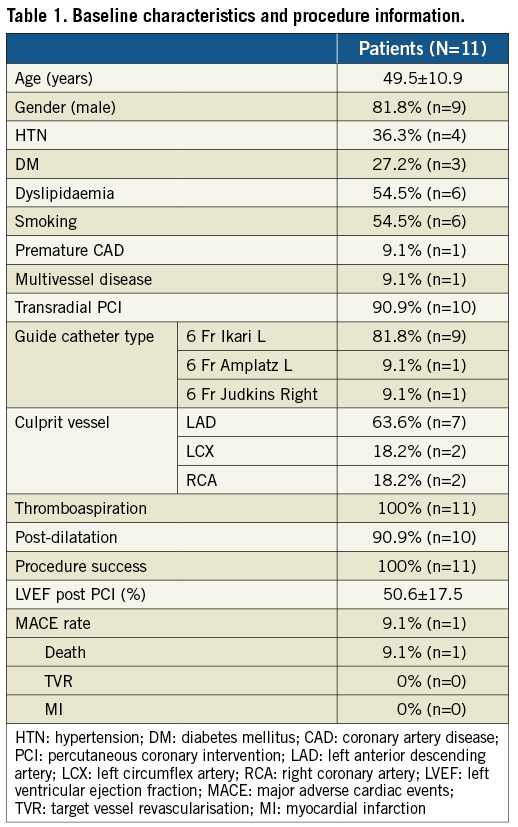
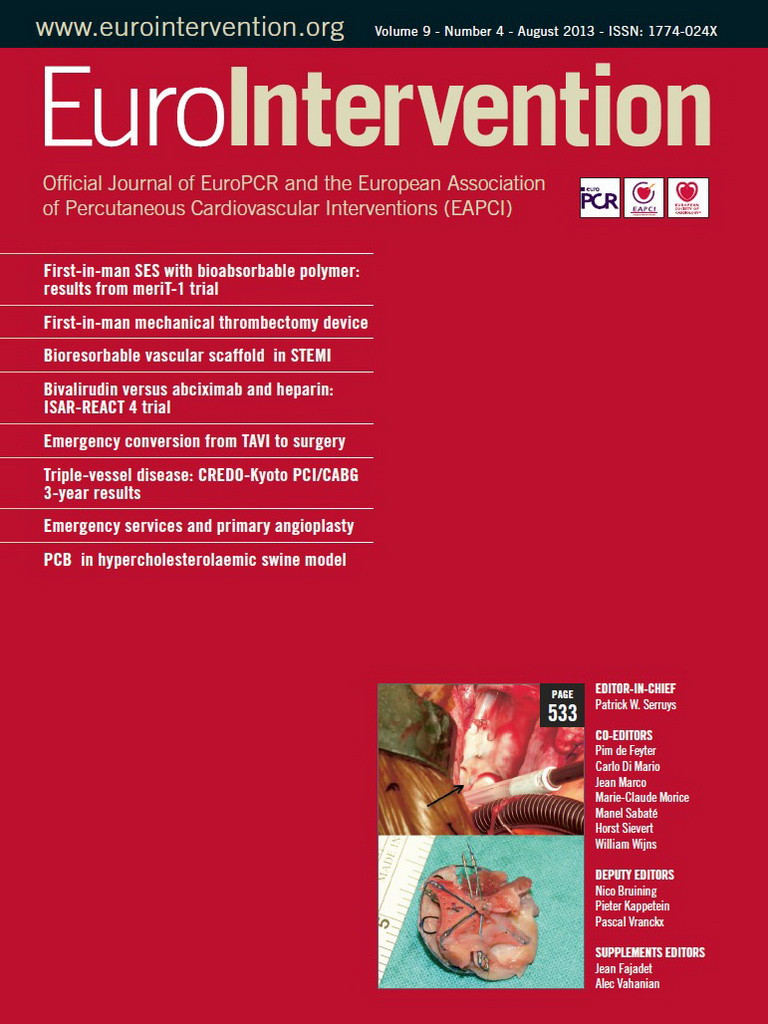
Representative angiography and optical coherence tomography images of a patient presenting with anterior STEMI are detailed in Figure 1 (Moving image 1 - Moving image 3). Details of a patient with diffuse disease are shown in Figure 2 (Moving image 4 - Moving image 7). This patient required implantation of two BVS to the left anterior descending artery.
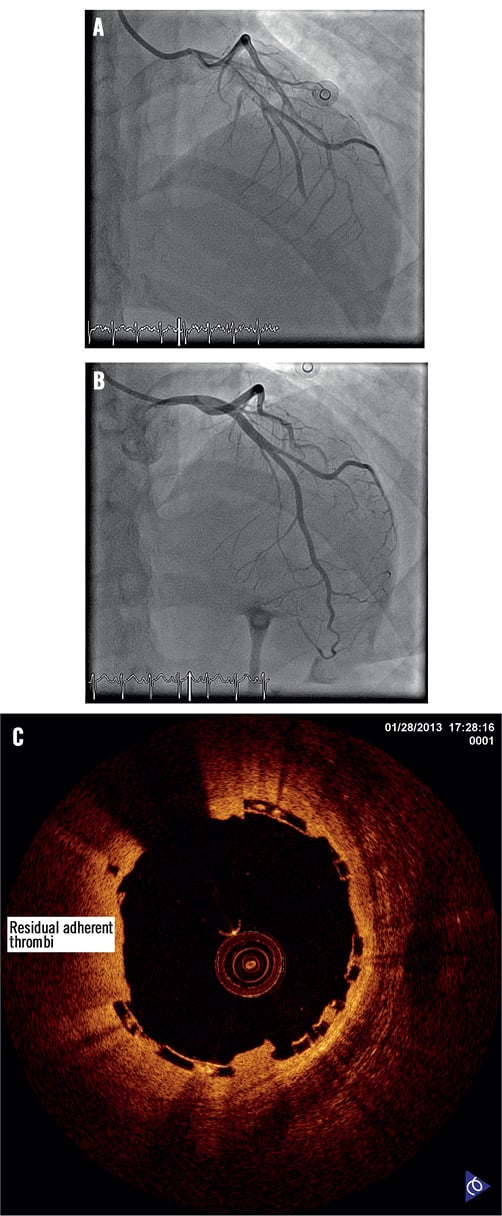
Figure 1. Representative angiography pictures. A) Coronary angiography of patient presenting with anterior STEMI, prior intervention documenting a thrombus in the proximal LAD; B) Coronary angiography of LAD after thrombus aspiration and BVS implant; C) Optical coherence tomography performed at BVS implant site. (Moving images 1-3) BVS: bioresorbable vascular scaffold; LAD: left anterior descending artery; STEMI: ST-segment elevation myocardial infarction
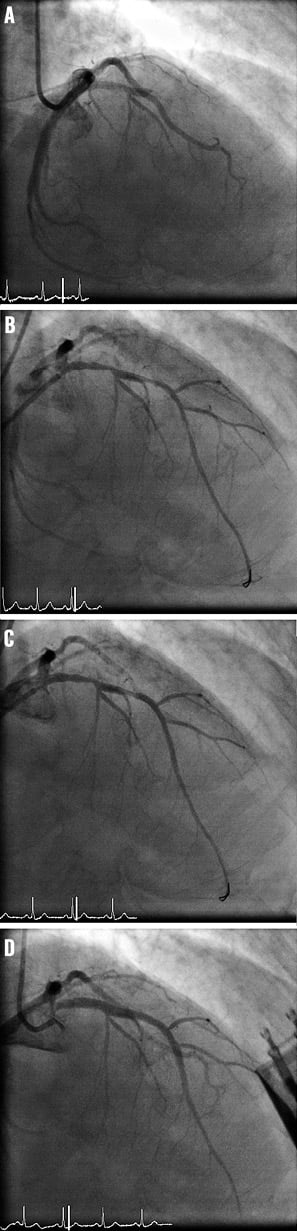
Figure 2. Patient with diffuse LAD disease. A) Coronary angiography documenting occluded LAD at presentation; B) Diffuse nature of LAD is evident after thrombus aspiration and balloon angioplasty; C) Following implant of first BVS across the mid-LAD lesion; D) Final angiography following implant of 2 BVS. (Moving images 4-7) BVS: bioresorbable vascular scaffold; LAD: left anterior descending artery
Discussion
In this single-centre observational study investigating safety and clinical outcomes of BVS in patients with STEMI, we observed that BVS could be safely used with at least a favourable short-term outcome. Recent studies have demonstrated favourable clinical outcomes and neointimal response compared with conventional metallic drug-eluting stents3-5. However, current cohort and randomised clinical trials with BVS exclude patients with acute myocardial infarction3,4,6. Our brief observation involving real-world data supports the use of BVS in patients presenting with STEMI. No acute or subacute stent thromboses were observed despite its use in the emergency setting. The single mortality in our series does not appear related to BVS use and was probably a consequence of the patient’s extremely ill state on presentation.
The appeal of BVS is its non-permanence, especially in the young patient, and this was a major consideration in its choice during primary angioplasty. This is particularly important where there is a high likelihood of repeat intervention either by PCI or subsequent bypass surgery. This is illustrated in the patient with diffuse left anterior descending artery disease requiring two BVS during primary angioplasty (Figure 2). Most patients had good salvage of the myocardium and mean left ventricular ejection fraction was 50.6% post PCI.
The main limitations of our study are the small number of patients and its observational nature. Further studies in a larger number of patients will be required to confirm our findings.
In conclusion, these are the first real-world data using BVS in patients with STEMI. The ABSORB™ BVS may be used safely in patients with STEMI undergoing primary PCI with a favourable short-term outcome.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Coronary angiography of a patient presenting with anterior STEMI prior intervention documenting a thrombus in the proximal left anterior descending artery.
Moving image 2. Coronary angiography after thrombus aspiration and BVS implant.
Moving image 3. Optical coherence tomography performed at BVS implant site.
Moving image 4. Coronary angiography documenting an occluded left anterior descending artery at presentation.
Moving image 5. Diffuse nature of the left anterior descending artery is evident after thrombus aspiration and balloon angioplasty.
Moving image 6. Following implant of 1st BVS across the mid left anterior descending artery lesion.
Moving image 7. Final angiography following implantation of two BVS in the proximal to mid left anterior descending artery.