Abstract
Aims: Coronary microvascular function has important diagnostic and prognostic implications but routine assessment is difficult. The index of microcirculatory resistance (IMR) is a reliable but invasive measure. We evaluated whether left ventricular contractile reserve (CR), measured with strain imaging on dobutamine echocardiography (DSE), is a reliable non-invasive measure of coronary microvascular function.
Methods and results: Forty-five patients underwent low-dose DSE and invasive coronary angiography with IMR measurement in the left anterior descending artery. Global mean peak systolic longitudinal strain was measured in three apical views at rest, and with low-dose DSE. CR was the difference between the resting and low-dose values. Mean IMR was 19.8 (range 6-104): mean peak global systolic strain at rest was –17.90% and at low-dose was –21.46%, giving a mean CR of +3.6% (20% relative increase). IMR and CR were significantly correlated, IMR–1=(0.0014×CR+0.05), r=0.64, p<0.001. CR of ≥10% relative increase identified IMR <25 (100% sensitivity and specificity) and <16 (93% sensitivity, 50% specificity [AUC=0.84]). CR ≥20% identified IMR of <16 (78% sensitivity, 82% specificity) with CR ≥ 41% having 100% specificity.
Conclusions: LV CR with low-dose DSE may be used to estimate IMR non-invasively. An impaired CR indicates coronary microvascular dysfunction.
Abbreviations
CFR: coronary flow reserve
CR: contractile reserve
DSE: dobutamine stress echocardiography
FFR: fractional flow reserve
IMR: index of microcirculatory resistance
LV: left ventricular
Introduction
The endothelium plays a pivotal role in vascular homeostasis and controls blood flow to end organs. The earliest manifestation of vascular disease may be seen as microvascular dysfunction before overt changes are seen in larger conduit vessels. Coronary microvascular dysfunction may lead to myocardial ischaemia in the absence of epicardial coronary artery disease, and can occur in the presence of vascular risk factors without overt atherosclerotic disease1. It is present in a wide range of cardiovascular disorders, including cardiomyopathies, stable coronary artery disease and in acute coronary syndrome. As coronary microvascular dysfunction is of prognostic value in a wide range of cardiovascular diseases and may be reversible with risk factor modification, lifestyle changes and treatment2, its earliest detection and proper evaluation are of clinical importance.
Routine assessment of the coronary microcirculation is difficult. Anatomical measures to evaluate the coronary microvasculature are limited as visualisation is not possible with current imaging techniques. Non-invasive assessment with transthoracic (including Doppler and contrast) echocardiography, CT scan or nuclear techniques have been unsatisfactory and are not applied routinely3. The index of microcirculatory resistance (IMR) is a novel invasive measure of coronary microvascular function and has been validated in vitro4, in animal models, and tested in stable patients with coronary disease as well as in those with acute myocardial infarction4-8. This technique is relatively independent of haemodynamic changes, and can be used in the presence of epicardial disease9. While the IMR allows assessment of coronary microvascular function, it cannot be used in routine clinical practice due to its invasive nature and costs; hence suitable and easily applicable non-invasive surrogates are still lacking.
A reduced left ventricular (LV) contractile reserve (CR) to inotropic stimuli has been shown to be a reliable sign of subclinical LV dysfunction in valvular heart disease10. The evaluation of CR in this setting was limited to visual wall motion assessment, and the measurement of post-exercise ejection fraction and LV end-systolic volume. Two-dimensional (2-D) speckle tracking is commercially available semi-automated software that tracks myocardial motion throughout the cardiac cycle and allows rapid generation of regional and global myocardial strain that is site-specific, load and angle independent11-13. Two-dimensional speckle tracking strain imaging during DSE allows sensitive and accurate quantification of CR compared with visual wall motion assessment and has been shown to be of incremental value to visual assessment during dobutamine echocardiography14. We postulate that LV CR in response to low-dose dobutamine is endothelial function-dependent and, measured with strain imaging, is a reliable non-invasive surrogate of microvascular function as measured by IMR in patients without significant epicardial disease.
Methods
PATIENTS
Forty-eight patients referred for elective diagnostic coronary angiography at our institution were recruited. As severe epicardial coronary stenoses may affect the measurement of microvascular resistance, requiring the additional measurement of coronary wedge pressure to account for the influence of the collateral circulation9, only coronary arteries without high-grade epicardial stenoses (defined as ≥70% diameter stenosis by computer-assisted quantitative coronary angiography using multiple planes, and fractional flow reserve [FFR] ≤0.75) were included in this study. Patients with known significant coronary artery disease, acute coronary syndrome, significant valvular disease, severe hypertension (systolic pressure >200 mmHg and diastolic pressure >120 mmHg at rest), significant renal insufficiency (eGFR <30 ml/min/m2), left bundle branch block and rhythm other than sinus were excluded. All cardiac medications (including beta-blocking agents and calcium channel antagonists) were continued throughout the studies with no modifications made to the patients’ treatment regimen. All patients provided written informed consent. The study was approved by the hospital human research ethics committee.
CORONARY ANGIOGRAPHY AND CORONARY PHYSIOLOGY MEASUREMENTS
Selective coronary angiography was performed in multiple projections according to standard techniques. After conventional diagnostic coronary angiography, a total of 100 U/kg of intravenous heparin was administered, a 6 Fr coronary guiding catheter was used to engage the left main coronary artery, after which 200 mcg of intracoronary nitroglycerine was given. A 0.014 inch coronary pressure wire (St. Jude Medical, St. Paul, MN, USA) was calibrated, equalised to the guiding catheter pressure with the sensor positioned just outside the ostium of the guiding catheter, and then advanced to the distal left anterior descending artery. The mean distance from the guide tip to the sensor was 8.6±2.1 cm. Coronary flow reserve (CFR), IMR and FFR were then measured at baseline and at maximal hyperaemia as described below.
The transit time of 3 mL of normal saline at room temperature injected down the coronary artery through the guiding catheter was determined using thermodilution technique at rest and again after maximal hyperaemia15. The average of three injections was measured. Steady state maximal hyperaemia was then induced using 140 mcg/kg/min of adenosine infused intravenously through a large-bore cannula in the antecubital fossa. Simultaneous measurements of mean aortic pressure measured at the tip of the guiding catheter and mean distal coronary pressure from the pressure wire were also taken at rest and at maximal hyperaemia. Coronary flow reserve was measured by the transit time at rest divided by the transit time at maximal hyperaemia. The IMR was measured by the product of distal coronary pressure and transit time at maximal hyperaemia6. Fractional flow reserve was calculated as the ratio of distal to proximal coronary pressures at maximal hyperaemia (Figure 1). There was no significant correlation between the distance between the guiding catheter tip and sensor position and mean resting or hyperaemic coronary transit time (r=0.53, p=0.14; and r=0.34, p=0.37, respectively). Cut-off values of an IMR of 16 and 25 to identify coronary microvascular dysfunction were used. These cut-off values of IMR were based on previous validation studies performed in swine models at baseline and after microcirculatory disruption5.
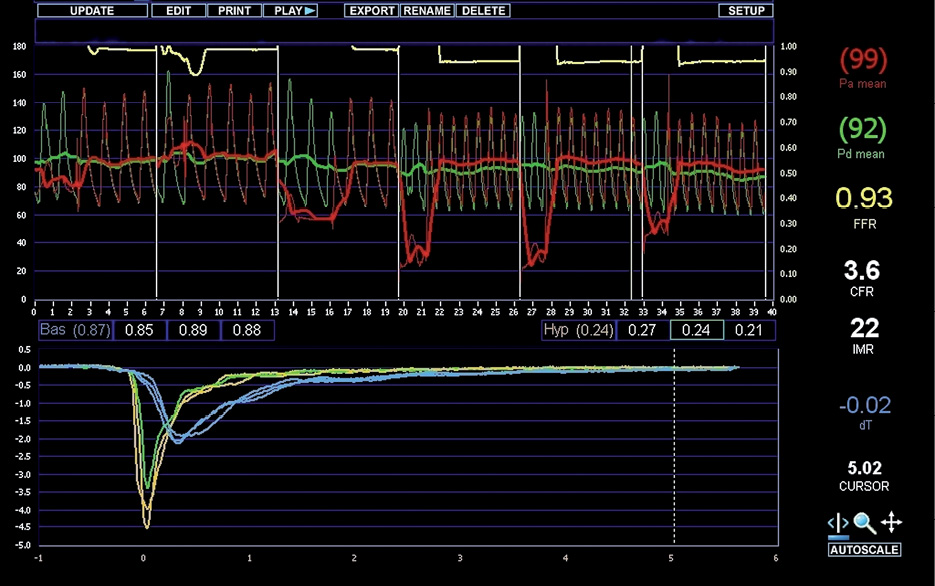
Figure 1. Example of CFR, IMR and FFR measurements. In this example, the mean transit time at rest (blue curves) was 0.87 seconds, and at maximum hyperaemia (yellow and green curves) 0.24 seconds. FFR was 0.93, CFR 3.6 and IMR 22.
DOBUTAMINE ECHOCARDIOGRAPHY
Two-dimensional transthoracic echocardiography was performed in the left lateral decubitus position with commercially available ultrasound equipment (M3S probe, Vivid 7; GE Healthcare Life Sciences, Little Chalfont, Buckinghamshire, UK). Images were digitally stored on hard discs for offline analysis (EchoPAC, BT10; GE Healthcare Life Sciences). A complete 2-D, colour, pulsed and continuous-wave Doppler examination was performed according to standard techniques at rest. LV ejection fraction was calculated using the Simpson biplane method of discs.
Dobutamine stress echocardiograms and coronary angiography were performed at a mean of 5.3 days apart, using standard protocols16. DSE images were acquired at rest and at low-dose dobutamine infusion. Low-dose DSE images were acquired at 10 mcg/kg/min (if the patient was not taking beta-blocking agents or calcium-channel antagonists), or 20 mcg/kg/min (if the patient was on beta-blocking agents or calcium antagonists). The 2-D images of the LV were obtained with the highest possible frame rates in the apical four-chamber, two-chamber, and long-axis views.
TWO-DIMENSIONAL SPECKLE TRACKING
Two-dimensional speckle tracking analyses were performed by an experienced independent observer blinded to the clinical history, coronary angiography and coronary physiology measurements. During 2-D speckle tracking analyses, the endocardial border was manually traced at end-systole and the region of interest width was adjusted to include the entire myocardium. The software then automatically tracks and accepts segments of good tracking quality and rejects poorly tracked segments, while allowing the observer to manually override decisions based on visual assessments of tracking quality. The mean global longitudinal systolic strain was calculated from the three global longitudinal strain curves of the three apical views. The mean global peak negative systolic longitudinal strain was measured in the three apical views at rest and low-dose dobutamine (Figure 2). Contractile reserve was then calculated as the mean global peak negative systolic longitudinal strain at low-dose dobutamine minus the corresponding values at rest. All Doppler and 2-D speckle tracking echocardiographic measurements were taken as averages of three representative cycles.
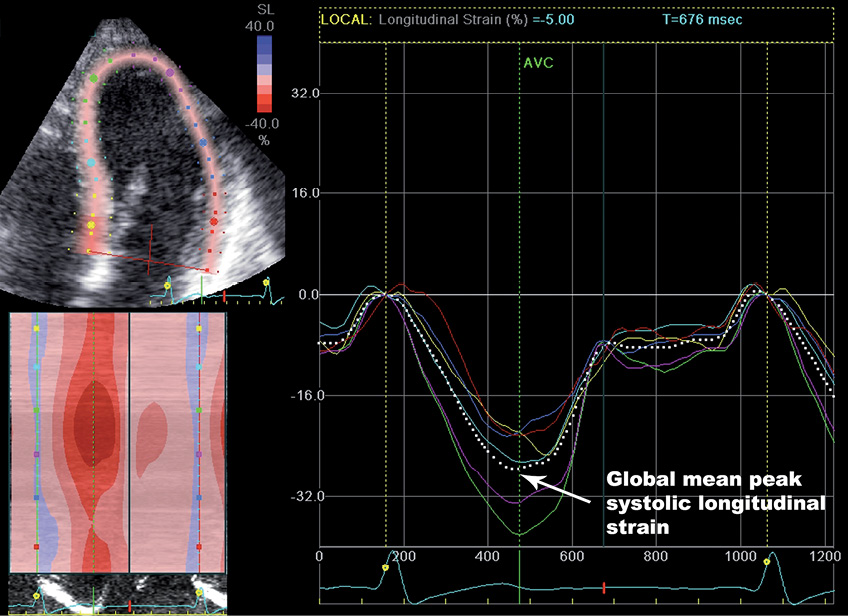
Figure 2. Example of calculation of global mean peak systolic strain from the apical four-chamber view. The left panel shows the two-dimensional representation and the bold dotted white line in the right panel represents the mean values of all LV myocardial segments throughout one cardiac cycle with the ECG shown at the bottom of the graph.
INTEROBSERVER AND INTRAOBSERVER VARIABILITY ANALYSIS
Strain measurements were repeated in five randomly selected patients at rest and low-dose dobutamine at least four weeks apart by the same observer (ML) on the same echocardiographic images, and by a second observer (DL) to determine intraobserver and interobserver variability respectively.
The interobserver and intraobserver variability of measurements of transit times were assessed in five randomly selected patients. After positioning of the pressure wire in the distal left anterior descending artery, one observer (DL) performed three baseline saline injections and recorded the mean transit time. Following this, a second observer (ML), who was blinded to the first result, then repeated these three measurements to determine intraobserver and interobserver variability.
Statistical analysis
Continuous variables were presented as mean±1 SD unless otherwise stated. Simple linear regression was performed using an inverse transformation to ensure Gaussian distribution of the data to determine the relationship between CR and IMR. Correlations between CR and CFR were assessed similarly. Receiver operating characteristic (ROC) analysis was performed for CR to identify optimal cut-offs for identifying significant microvascular dysfunction by IMR defined by the various pre-defined criteria. Intraobserver and interobserver variability were expressed as mean differences and Pearson correlation coefficients between the two sets of measurements and as coefficients of variation. A two-tailed p-value <0.05 was considered significant. All statistical analyses were performed using STATA version 12 (StataCorp, College Station, TX, USA).
Results
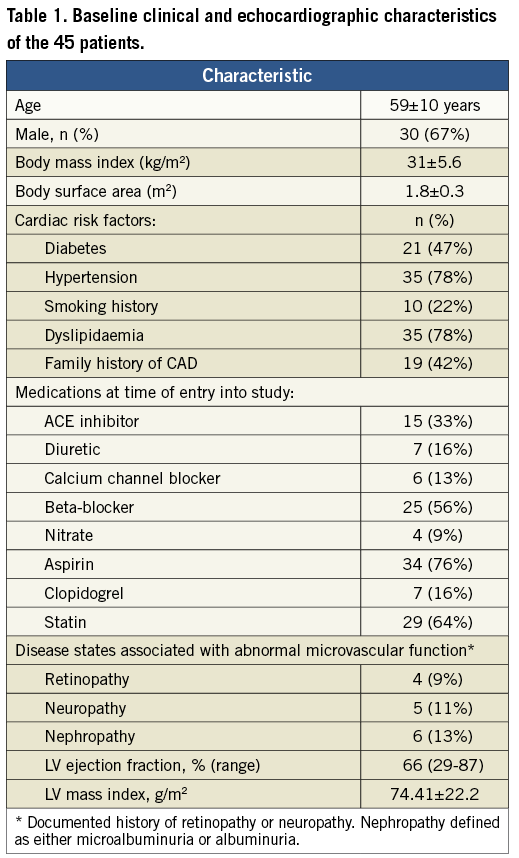
Three patients with either rest or inducible regional wall motion abnormalities on DSE and angiographically significant epicardial coronary artery disease were subsequently excluded. Therefore, DSE and coronary physiology measurements were studied in the remaining 45 patients. Baseline clinical, echocardiographic characteristics and the prevalence of other disease states associated with abnormal microvascular function are presented in Table 1. The primary reasons for referral for coronary angiography were: chest pain (81%), dyspnoea (11%) and dilated cardiomyopathy (8%). During coronary physiology measurements, the mean blood pressure at rest and maximal hyperaemia were 134/74 mmHg and 118/65 mmHg, respectively. During DSE, the mean heart rate and blood pressure at rest were 68±13/min and 136/80±20/12 mmHg; and 72±15/min and 141/76±27/14 mmHg during low-dose dobutamine. The mean CFR was 3.89 (interquartile range [IQR] 2.75-5.20), mean FFR was 0.88 (IQR 0.83-0.92), and mean IMR was 19.85 (IQR 10.68-18.00). There was no significant difference between IMR in males and females (22 vs. 16, p=0.30).
The mean frame rate during DSE was 77.8±8.6 frames/second. The resting and low-dose DSE heart rates were 39.4±7.1% and 45.1±9.2% of age-predicted maximum, respectively. The mean peak global systolic strain at rest was –17.9%, and at low dose –21.46% corresponding to a mean CR of +3.6% (20% relative increase).
RELATIONSHIP BETWEEN CONTRACTILE RESERVE AND IMR
There was a significant linear relationship between the inverse of IMR and CR, expressed in % relative change (Figure 3), IMR–1= (0.0014×CR+0.05), r=0.64, p<0.001.
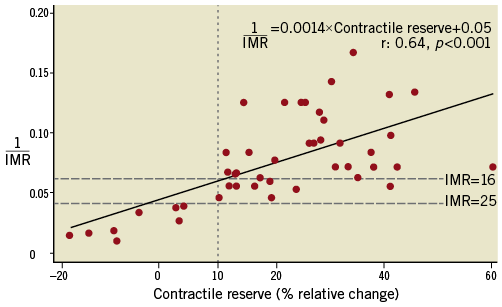
Figure 3. Contractile reserve plotted against the inverse of the index of microvascular resistance (IMR) for the left anterior descending artery. The horizontal lines represent IMR of 25 and 16. The vertical line represents the cut-off value of CR of 10% relative increase, which provides perfect separation between those with good microvascular function (IMR <25) and good CR, and those with impaired microvascular function (IMR ≥25) and poor CR.
Receiver operating characteristic analysis revealed that a CR of ≥10% identified an IMR of <25 with 100% sensitivity and 100% specificity (AUC=1.0), and an IMR of <16 with 93% sensitivity and 50% specificity (AUC=0.84) (Figure 4). A CR of ≥20% identified an IMR of <16 with 78% sensitivity and 82% specificity; whilst a CR of ≥41% identified an IMR of <16 with 100% specificity. There was no significant relationship between CR and CFR. There was no difference in LV mass index in patients with an IMR of ≥ versus <16 (75.59 g/m2 vs. 73.63 g/m2, p=0.78), or patients with an IMR of ≥ versus <25 (77.19 g/m2 vs. 73.82 g/m2, p=0.70).
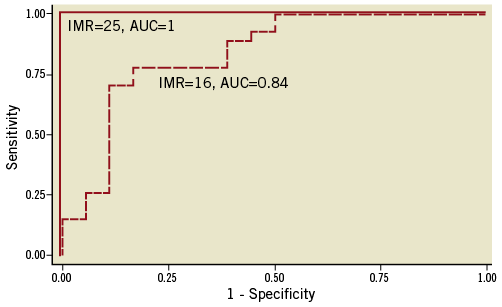
Figure 4. Receiver operating characteristic (ROC) curves for different IMR values. The solid line is the ROC curve for IMR ≥25 and the dotted line is for IMR ≥16. AUC: area under the curve
INTEROBSERVER AND INTRAOBSERVER VARIABILITY
The intraobserver mean differences for resting and low-dose mean global systolic longitudinal strain were –0.15±0.15 (p=0.09, r=0.998) and 0.02±0.07 (p=0.66, r=1), respectively. These corresponded to mean differences in CR and relative increases in CR measurements of 0.16±0.17 (p=0.10, r=1) and 1.18%±0.98% (p=0.06, r=0.999).
The interobserver mean differences for resting and low-dose mean global systolic longitudinal strain were –0.35±1.5 (p=0.63, r=0.82) and 0.07±1.3 (p=0.91, r=0.94), respectively. These corresponded to mean differences in CR and relative increase in CR measurements of –0.43±0.42 (p=0.08, r=0.998) and –4.74%±6.28% (p=0.17, r=0.995).
The coefficients of variation of coronary transit time measurements at baseline were 4.0%±2.2%, and 5.1%±2.7% at maximal hyperaemia.
Discussion
The present study demonstrated that a reduced CR to low-dose DSE accurately identified impaired coronary microvascular function as measured by IMR. Quantitative measurement of CR with low-dose DSE using 2-D speckle tracking strain imaging is feasible and has acceptable interobserver and intraobserver variability.
Microvascular dysfunction is present and has important prognostic implications in a wide range of ischaemic and non-ischaemic cardiovascular diseases17. Furthermore, microvascular dysfunction predates the development of overt atherosclerotic diseases and is potentially reversible. Therefore, early detection is clinically important. While there are a number of methods to assess coronary microvascular function3, their routine clinical use is not practical. Doppler echocardiography to measure CFR has been used. However, obtaining the full spectral display throughout the cardiac cycle may not always be possible due to cardiac motion. Contrast echocardiography with microbubbles has been used to evaluate myocardial perfusion to measure CFR in research studies, but echo contrast is approved only for LV opacification.
The IMR can be measured invasively and has been shown to correlate well with true microvascular resistance in an animal model5. Unlike CFR, it has a much lower measurement variability and is not significantly affected by changes in haemodynamic conditions6. The IMR has been validated in stable coronary disease as well as in the post-infarct setting and has been shown to provide prognostic information5-8,18. Variability in the measurement of transit times for IMR in our study was similar to that reported in other studies6,18. The determination of normal versus abnormal microcirculatory function with IMR has been based upon a swine model before and after microcirculatory disruption by injection of microspheres into the left anterior descending artery. IMR increased from baseline values of 16.9±6.5 to 25.9±14.4 after microvascular disruption. In the subgroup without coronary artery stenosis, IMR increased from 14.7±4.8 to 23.9±3.85. Therefore, an IMR of >25 is generally accepted as indicative of abnormal microcirculatory function. Normal IMR values in humans have not been established. In the present study, cut-off values of IMR of 16 and 25 to identify coronary microvascular dysfunction were used. With a cut-off value of an IMR of 25, CR of ≥10% provided 100% accuracy for detecting microvascular dysfunction. With a lower threshold of an IMR of 16, the same CR provided 93% sensitivity and 50% specificity. Meanwhile, a CR of ≥41% identified an IMR of <16 with 100% specificity. The latter cut-off of ≥41% may be useful in situations where it is necessary to ensure excellent microvascular function indicated by an IMR <16.
The utility of assessing LV CR is well established in a number of clinical conditions. CR may be used to determine the presence of subclinical LV dysfunction in chronic mitral regurgitation in order to predict LV function after mitral valve repair. Exercise was used as the inotropic stimulus, and CR was calculated as the change in ejection fraction and LV end-systolic volume post exercise. Low-dose DSE is an established technique to assess CR of dysfunctional myocardium to identify viability. The detection of viable myocardium is critical for risk stratification, guiding selection of patients who are likely to benefit from revascularisation and predicting LV recovery19. Microvascular integrity is a fundamental prerequisite for myocardial viability20. Therefore, CR is dependent on microvascular function. Dobutamine is predominantly a beta- adrenergic agonist and decreases microvascular resistance21, simultaneously activating additional vascular receptors, dependent on normal microvascular function22,23. It is physiological that LV CR to low-dose dobutamine reflects microvascular function and therefore can be used as an indicator of coronary microvascular function as suggested by the results of our study. The evaluation of CR may be used to confirm the presence of microvascular disease in patients with conditions known to be associated with microvascular dysfunction, in patients with dilated cardiomyopathy, suspected syndrome X, and in patients with unexplained ischaemic symptoms.
Coronary flow reserve has also been used to evaluate coronary microvascular function. However, CFR is limited by high measurement variability and its sensitivity to haemodynamic changes due to variation in baseline flow velocities24. Furthermore, CFR, unlike IMR, is affected by epicardial coronary stenosis25. Therefore, it is perhaps not surprising that CR is not correlated with CFR in our study.
Limitations
Our sample size was relatively small and patients were selected from those who were clinically referred for elective coronary angiography and may represent a biased group. The measurement of CFR, FFR, and IMR are reliant upon the achievement of maximal hyperaemia. Intravenous adenosine is considered the reference standard for inducing maximal hyperaemia, and was used in the present study. Recent studies have suggested a requirement for adenosine dosages of 180 mcg/kg/min13,26. A study by De Bruyne et al on the effects of intravenous adenosine doses in humans of 140-180 mcg/kg/min in achieving maximal hyperaemia showed that at doses >140 mcg/kg/min, there was no further decrease in FFR, nor a further increase in coronary flow velocities. It was concluded that there was no benefit in administering doses higher than 140 mcg/kg/min27. The distance of the pressure-temperature sensor of the coronary wire from the guide catheter tip has been noted in previous studies to impact on the variability of measurement of hyperaemic transit times and coronary thermodilution curves. It has previously been shown that a minimum distance of >6 cm of the transducer from the guide tip results in <10% variability in transit time measurements4. However, in this study, there was no correlation between sensor distance and transit times.
Left ventricular CR at low-dose dobutamine echocardiography is a reliable and non-invasive surrogate for coronary microcirculatory function by the IMR. An impaired CR indicates coronary microvascular dysfunction. Low-dose DSE can be used to evaluate coronary microvascular function non-invasively in patients with risk factors and suggestive symptoms for more refined risk stratification, obviating the need for expensive and invasive studies.
Funding
The study was partially funded by a Pfizer Cardiovascular Lipid Research Grant.
Conflict of interest statement
The authors have no conflicts of interest to declare.

