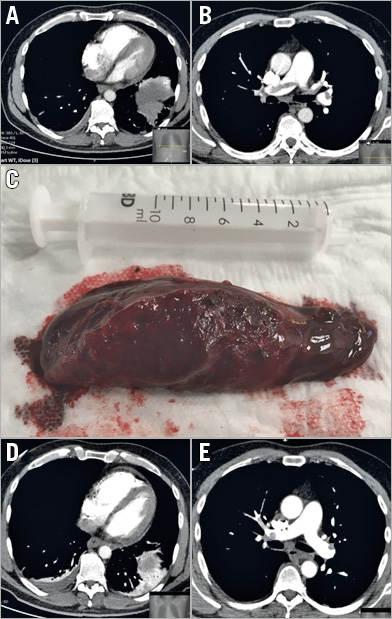
Figure 1. Lung embolism before and after aspiration. A) & B) Evidence of right heart dysfunction and lung embolism before procedure. C) The lung embolism after aspiration. D) & E) Post-procedural evidence of improved haemodynamics and absence of the embolus.
A 50-year-old man with a known heterozygous factor V Leiden mutation and a history of deep vein thrombosis (1980 and 2015) underwent abdominal surgery for colorectal carcinoma. Fourteen days after surgery, under prophylactic therapy with 5,000 IU dalteparin o.d., the patient developed dyspnoea and tachycardia. Blood pressure was 100/60 mmHg, heart rate 110/min. ECG showed a typical SIQIII pattern, and computed tomography confirmed the presence of central lung embolism with signs of right ventricular overload (RV/LV ratio ~2, RV diameter 45 mm) (Figure 1A, Figure 1B). Peak HS-troponin I was 566 ng/ml. Based on the presence of signs of impending haemodynamic instability with a contraindication to systemic lysis (recent surgery, cancer), it was decided to perform thrombus aspiration.
After administration of heparin 5,000 IU, a 65 cm 8 Fr sheath (Destination®; Terumo, Leuven, Belgium) was advanced through a right femoral access over an Amplatz extra stiff 0.035” wire. The pulmonary artery was engaged using a standard JR4 catheter. The right pulmonary artery was selectively imaged using a 6 Fr pigtail catheter, confirming the presence of a large thrombus (Moving image 1). Multiple aspirations were performed with an Indigo System CAT8 (Penumbra, Inc., Alameda, CA, USA) (Moving image 2). At the end of the procedure, a ~8×3 cm thrombus could be retrieved from the canister (Figure 1C). Selective imaging confirmed the removal of the thrombus (Moving image 3), which was also evident at control tomography 24 hours after the procedure. At this time, the RV/LV ratio was ~1, with an RV diameter of 40 mm (Figure 1D, Figure 1E). On echocardiography, pulmonary pressure was 20 mmHg without signs of right ventricular overload. Intravenous (followed by subcutaneous) low-molecular weight heparins were administered after the procedure, followed by oral anticoagulation. The patient was discharged from the intensive care unit on day one in a stable haemodynamic condition.
We describe a case of lung embolism in a patient treated with prophylactic low-molecular weight heparin and a contraindication to thrombolysis. Catheter-based techniques (i.e., the use of devices and techniques to remove/fragment thrombi with or without low-dose thrombolytic therapy) is a rarely used alternative for the treatment of lung embolism1,2. Although current evidence is mostly limited to case reports and retrospective series, these techniques may represent an alternative/adjunct to thrombolytic therapy, particularly for patients with contraindications to lysis and a favourable anatomy (central embolisms). Randomised trials on the effectiveness and safety of these therapies are necessary. The current case demonstrates the possible efficacy of this approach.
Conflict of interest statement
The author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Evidence of thrombus in the right pulmonary artery.
Moving image 2. Aspiration with the Indigo System.
Moving image 3. Immediate result.