Abstract
Pulmonary embolism (PE) ranks as a leading cause of in-hospital mortality and the third most common cause of cardiovascular death. The spectrum of PE manifestations varies widely, making it difficult to determine the best treatment approach for specific patients. Conventional treatment options include anticoagulation, thrombolysis, or surgery, but emerging percutaneous interventional procedures are being investigated for their potential benefits in heterogeneous PE populations. These novel interventional techniques encompass catheter-directed thrombolysis, mechanical thrombectomy, and hybrid approaches combining different mechanisms. Furthermore, inferior vena cava filters are also available as an option for PE prevention. Such interventions may offer faster improvements in right ventricular function, as well as in pulmonary and systemic haemodynamics, in individual patients. Moreover, percutaneous treatment may be a valid alternative to traditional therapies in high bleeding risk patients and could potentially reduce the burden of mortality related to major bleeds, such as that of haemorrhagic strokes. Nevertheless, the safety and efficacy of these techniques compared to conservative therapies have not been conclusively established. This review offers a comprehensive evaluation of the current evidence for percutaneous interventions in PE and provides guidance for selecting appropriate patients and treatments. It serves as a valuable resource for future researchers and clinicians seeking to advance this field. Additionally, we explore future perspectives, proposing “percutaneous primary pulmonary intervention” as a potential paradigm shift in the field.
Pulmonary embolism (PE) is a serious medical condition that occurs when fragments of a venous thrombus are dislodged and occlude one or more pulmonary arterial vessels, resulting in high morbidity and mortality1. Among cardiovascular diseases, PE ranks third after stroke and myocardial infarction, with an estimated annual incidence of 39 to 115 cases per 100,000 individuals2. The economic burden of PE is also substantial, encompassing costs associated with hospitalisation, diagnostic testing, anticoagulant therapy and long-term management of complications, resulting in an estimated healthcare burden of €3.8 billion in Europe and $18.9 billion in the United States, annually3. In addition, PE has a high mortality rate, with approximately 350,000 patients dying each year and up to 20% of patients dying within the first year after diagnosis245. Even after successful treatment of an acute episode, PE survivors are at risk of developing recurrent PE, chronic thromboembolic vascular disease, or chronic thromboembolic pulmonary hypertension, which can lead to functional impairment and further increase the risk of death over time6.
To mitigate the risks associated with PE, it is critical to focus on prevention, early diagnosis, proper risk stratification, and optimal treatment. In the prevention of PE, percutaneous positioning of filters in the inferior vena cava is an established option for selected high-risk patients with conditions such as vein thrombosis or recurrent PE despite antiÂcoagulation7. Regarding treatment, the approach to managing PE depends on the estimated mortality risk. Current guidelines recommend patients with haemodynamical instability to be considered at high risk of death, while stable patients are stratified based on various clinical, imaging, and laboratory markers, as well as any concomitant conditions that may impact their prognosis1. Anticoagulation is the mainstay of acute treatment for PE across all risk categories, but the management of PE is rapidly evolving with the development of new interventions and drugs that have shown promising results in selected patients. This expansion of available options offers new opportunities for both the treatment and prevention of PE1.
Systemic thrombolysis is currently indicated for high-risk PE patients, and as a rescue strategy for intermediate- or low-risk patients who experience haemodynamic deterioration despite anticoagulation1. This therapy can rapidly improve pulmonary perfusion and right ventricular (RV) function and is associated with a decreased risk of PE recurrence and mortality89. However, systemic thrombolysis is accompanied by substantial increases in the risk of major bleeding and intracranial haemorrhage8910. Furthermore, it cannot be used in patients with absolute contraindications, such as active bleeding, recent stroke or surgery, or central nervous system neoplasm. Additionally, systemic thrombolysis is not always successful, supporting the need for alternative treatment options8.
In response to the limitations of systemic thrombolysis, several percutaneous catheter-directed treatments have emerged as alternatives. These treatments aim to prevent the migration of thrombotic emboli from the deep venous system to the pulmonary circulation by utilising a filter or directly targeting the embolus in the pulmonary circulation through a venous catheter11. Percutaneous treatment options include the local administration of low-dose thrombolysis, with or without the aid of ultrasound imaging, and mechanical techniques for the fragmentation and aspiration of thrombi, or direct clot retrieval121314. These techniques have a high procedural success rate of approximately 87% and are associated with reduced mortality and a lower risk of major bleeding compared to systemic thromboÂlysis in patients with intermediate- or high-risk PE1516.
With this background in mind, the main focus of this article is to provide a comprehensive overview of percutaneous management options for PE, with a specific emphasis on catheter-directed treatments and their effect on patient outcomes. Furthermore, we aimed to identify gaps in current knowledge and areas for future research in the field, including the potential expansion of these techniques to patients at intermediate risk, which could lead to a broader application of these interventions.
Prevention of pulmonary embolism
INFERIOR VENA CAVA FILTER
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and PE, is strongly associated with transient hospitalisation or prolonged immobilisation and is often due to major surgery and major trauma. The two conditions account for approximately 60% of all VTE cases. The incidence of VTE is over 100 times greater in hospitalised patients compared to non-hospitalised patients, where active cancer accounts for almost 20% of all incident VTE in the latter group1718.
Patients at a high risk of VTE and those who have contraÂindications to anticoagulant therapy (or who experience recurrent PE despite adequate anticoagulation) may be candidates for vena cava interruption, which involves the placement of a filter device that mechanically prevents the embolisation of venous clots in the pulmonary circulation. A detailed and extensive overview regarding device characteristics, insertion procedure and supporting evidence is provided in Supplementary Appendix 1, Supplementary Table 1 and Supplementary Table 2.
Treatment of pulmonary embolism
RISK STRATIFICATION
Risk assessment is crucial to determining the appropriate management for patients with PE19. For high-risk cases (i.e., massive PE) accompanied by haemodynamic instability, an immediate referral for reperfusion treatment via an emergency management algorithm is necessary (Figure 1). This includes systemic thrombolysis, surgical embolectomy, or percutaneous catheter-directed treatments, with or without mechanical haemodynamic support (e.g., extracorporeal membranous oxygenation or isolated percutaneous right RV support)2021222324.
For patients without haemodynamic instability, further risk stratification of PE through prognostic clinical scores, imaging, and laboratory parameters is recommended. The low Pulmonary Embolism Severity Index (PESI) classes and low simplified PESI are reliable predictors of low-risk PE that requires therapeutic anticoagulation alone25262728. Conversely, PESI classes III-V identify intermediate-risk patients, and particularly, those with evidence of RV dysfunction and elevated cardiac biomarkers levels are classified as intermediate-high risk (i.e., submassive PE). These patients can be treated with anticoagulation alone; however, reperfusion treatment becomes essential if haemodynamic deterioration occurs1029.
Thrombolytic therapy − either systemic (most common) or directed by a catheter into the pulmonary arteries − can restore pulmonary circulation, relieve RV afterload, and improve systemic oxygenation and overall haemodynamics30. High-risk patients with haemodynamic compromise account for about 5% of the total PE cases and represent the subgroup at the highest risk for early mortality (about 50%), making them the ones who stand to benefit most from thrombolytic therapy3132 (Figure 2). The role of systemic or catheter-directed thrombolysis (CDT) in other patient subgroups is uncertain.
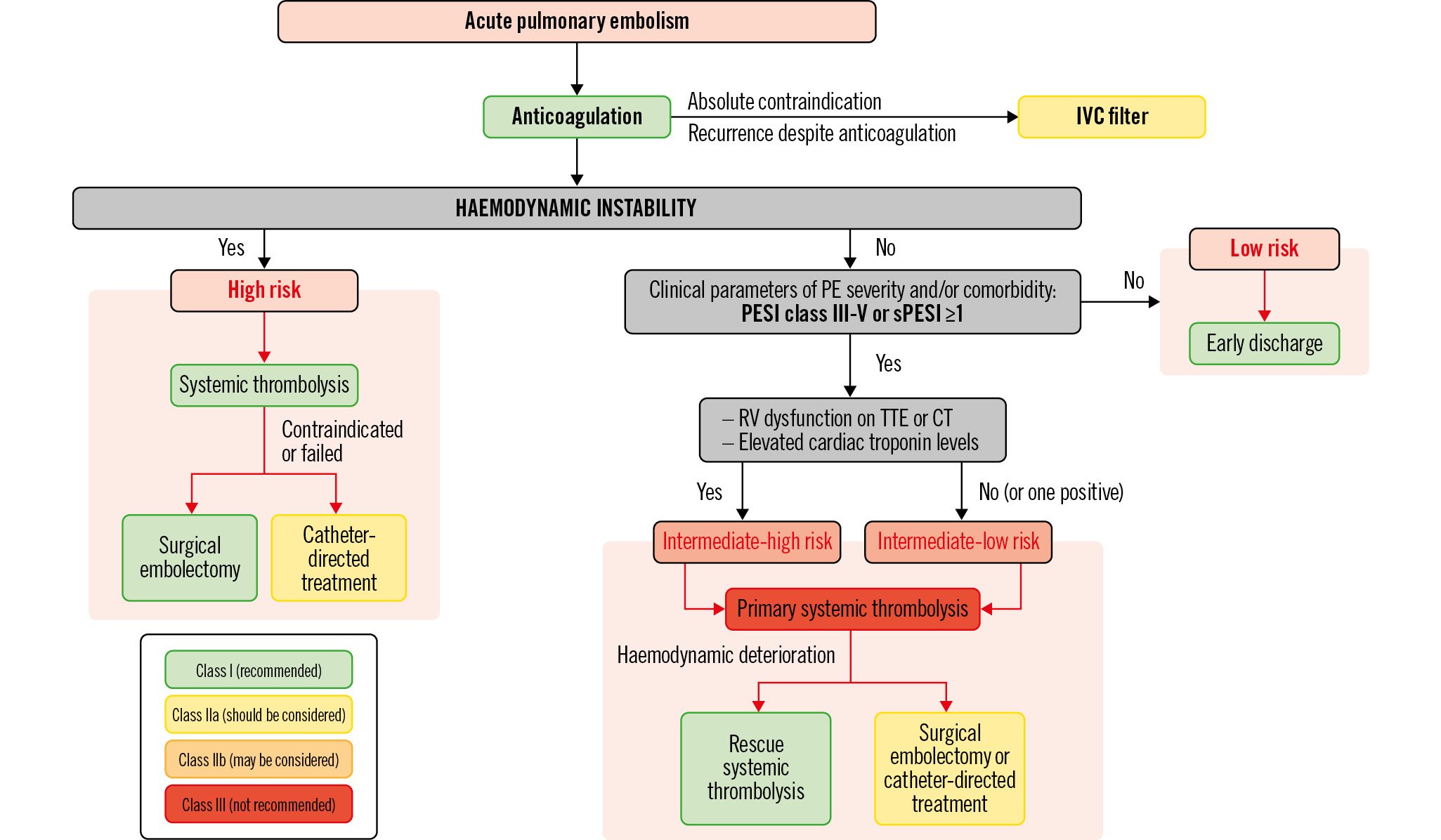
Figure 1. Therapeutic management of pulmonary embolism. The treatment of acute pulmonary embolism (PE) is closely related to the individual risk factors and the haemodynamic stability of the patient. In high-risk patients, characterised by the instability of haemodynamic parameters, parenteral anticoagulation with unfractionated heparin (UFH) represents the first-line therapy and must be started immediately (Class I recommendation). Anticoagulation must be associated with adequate reperfusion treatment: the approach of choice is represented by systemic thrombolysis (Class I), but, where this is contraindicated or has failed, current guidelines recommend surgical pulmonary embolectomy (Class I) or catheter-directed treatment (Class IIa). In intermediate-risk patients, anticoagulation is the first-line therapy; as with high-risk patients, it should be started immediately. Current guidelines recommend the use of low-molecular-weight heparin or fondaparinux over UFH. In the case of oral anticoagulant treatment, direct oral anticoagulants are preferred over vitamin K antagonists in eligible patients. In this clinical context, the routine use of systemic thrombolysis is not recommended (Class III) and is reserved as rescue therapy in patients who develop haemodynamic instability during anticoagulant treatment (Class I). Surgical pulmonary embolectomy or percutaneous catheter-directed treatment should be considered as an alternative to thrombolysis (Class IIa). Following resolution of the acute episode, a recurrence prevention strategy is critical. Anticoagulant therapy is recommended for all patients for at least 3 months after the index event (Class I), with the possibility of continuing it even in the long term depending on the causal event (e.g., antiphospholipid antibody syndrome, cancer). In patients with an absolute contraindication to anticoagulant treatment, a valid alternative is represented by inferior vena cava (IVC) filter placement, with the aim of mechanically preventing emboli from reaching the pulmonary circulation (Class IIa). Furthermore, IVC filters should be considered in case of recurrence despite adequate anticoagulant treatment (Class IIa), while their routine use is not recommended (Class III). CT: computed tomography; PESI: Pulmonary Embolism Severity Index; RV: right ventricular; sPESI: simplified Pulmonary Embolism Severity Index; TTE: transthoracic echocardiogram
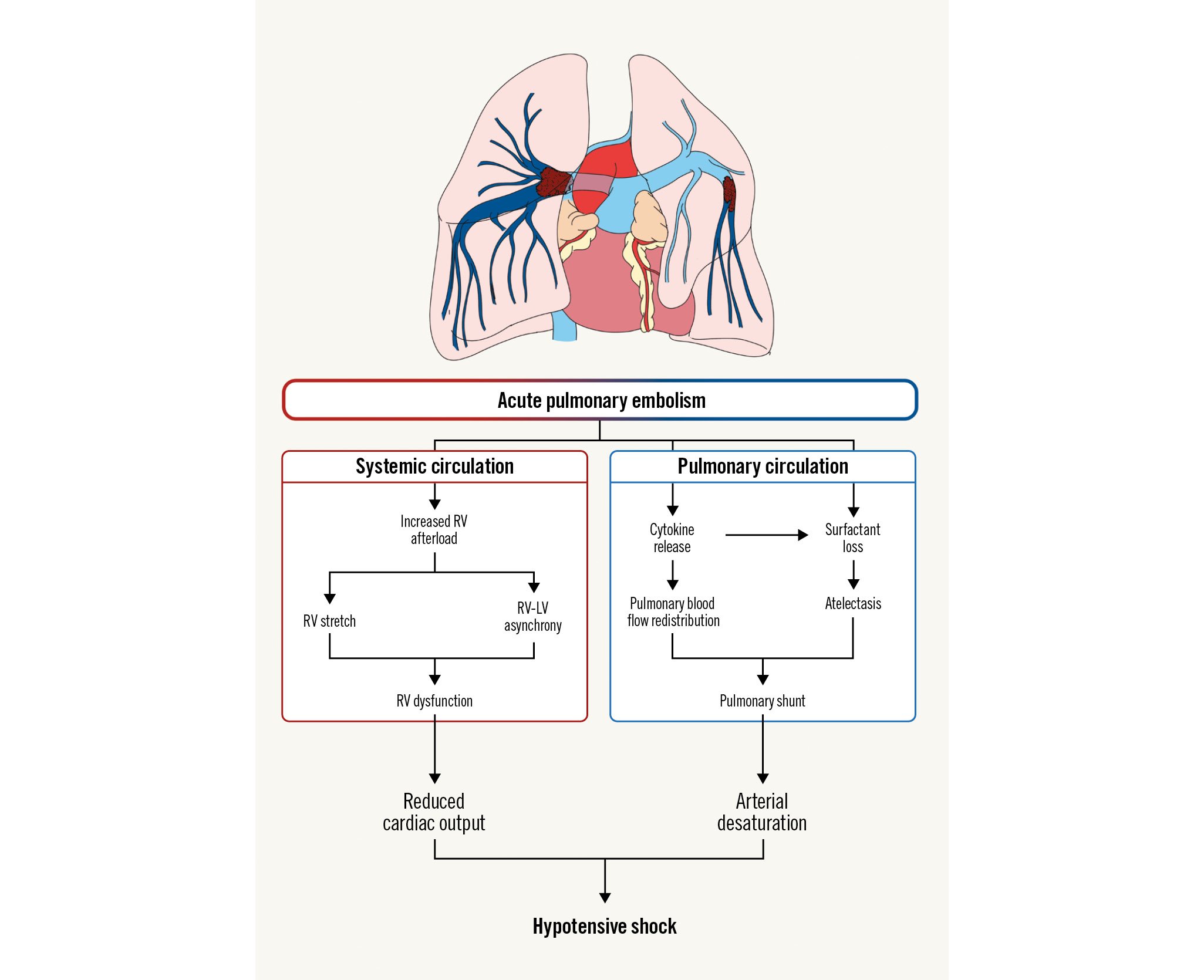
Figure 2. Pathophysiology of acute pulmonary embolism. Acute pulmonary embolism is characterised by a deep interplay between pulmonary and systemic circulation, which can lead to a wide range of presentations, from subclinical events to hypotensive shock. The pulmonary vasculature (blue box) can suffer from a dramatic redistribution in regional blood flow, due not only to the mechanical obstruction caused by the blood clot itself, but also from the local vasoconstricting cytokine release from the clot (i.e., histamine) and surrounding cells (i.e., endothelin, thromboxane). Such vasoactive agents can also act in alveoli surrounding the infarcted zone, leading to further vasoconstriction, reduced surfactant production and, ultimately, atelectasis. As a result, the redistribution can cause pulmonary shunt, resulting in increased ventilation/perfusion mismatch and systemic desaturation. The mechanical obstruction and pulmonary artery vasoconstriction can also impair systemic circulation (red box). The increased afterload can increase right ventricular filling pressure and impair blood efflux, ultimately leading to ventricle asynchrony and right ventricular dysfunction, resulting in reduced cardiac output. When the vascular bed is wide enough, the events occurring in the pulmonary and systemic circulations can exceed the counter-regulatory mechanisms (i.e., increased respiratory rate, reflex tachycardia), ultimately resulting in systemic hypotensive shock. RV: right ventricle; RV-LV: right ventricle-left ventricle
SYSTEMIC THROMBOLYSIS
Systemic thrombolysis is the primary treatment for high-risk PE, as it reduces total and PE-related mortality and PE recurrence, compared with unfractionated heparin alone133. Systemic thrombolysis involves intravenous administration of a fibrinolytic agent to promote clot resolution and restore distal pulmonary flow. However, its widespread use is limited because of multiple contraindications. In particular, systemic thrombolysis is associated with an increase in bleeding complications, including major bleeding and intracranial haemorrhage, reported in 10% of cases91034. As a result, only a minority of high-risk PE patients suitable for systemic thrombolysis actually receive it because of the perceived increased risk of bleeding3235. Nonetheless, in patients with relative contraindications to systemic thrombolysis, a half-dose thrombolytic therapy can provide similar efficacy rates35. Overall, in the setting of high-risk PE, the benefits of systemic thrombolysis mostly outweigh the risks, as prompt reperfusion is crucial in conditions of haemodynamic instability, and its wide availability allows for a reduced door-to-reperfusion time.
Conversely, further investigations are warranted to define the role of systemic thrombolysis in intermediate-risk PE. The largest randomised controlled trial to investigate the effect of systemic thrombolysis in normotensive patients with intermediate-risk PE was PEITHO10. It demonstrated that the decreased risk of haemodynamic decompensation associated with systemic thrombolysis was not accompanied by a reduction in 7-day mortality and came at the cost of an increased risk of severe extracranial and intracranial bleeding. Furthermore, over a median follow-up time of 37.8 months, systemic thrombolysis neither resulted in a lower mortality rate, nor did it reduce residual dyspnoea or RV dysfunction36. A single-centre, randomised trial of intermediate-risk PE showed that the strategy of administering a reduced-dose thrombolytic regimen was as effective and safe as administering a full-dose thrombolytic regimen in terms of reducing pulmonary pressure and bleeding complications37. In this context, the PEITHO-3 trial will randomise 650 intermediate-high-risk patients to receive either reduced-dose thrombolysis or standard-dose anticoagulation38. Overall, the use of systemic thrombolysis in intermediate-risk PE remains controversial and must be tailored to the individual patient.
SURGICAL EMBOLECTOMY
Surgical embolectomy is a potential treatment option for high-risk PE patients who cannot receive systemic thrombolysis due to contraindications or for whom this therapy previously failed1. To extract thrombi, a median sternotomy access is required with cardiopulmonary bypass, without aortic cross-clamping or cardioplegic cardiac arrest.
Over time, advances in surgical techniques and patient selection have reduced peri- and postoperative mortality rates, expanding the eligibility criteria for systemic embolectomy to include intermediate-high-risk PE with a risk of clinical deterioration and signs of impending RV failure2123. Surgical embolectomy is recommended for cases with a high proximal thrombus burden, thrombus in transit, paradoxical embolism, or haemodynamic instability, as it can improve RV function similarly to thrombolysis, with comparable 30-day mortality and 5-year survival rates3940. While most surgical outcome data come from small observational studies, the randomised Lungembolism trial (ClinicalTrials.gov: NCT03218410) compared surgical embolectomy to catheterÂ-directed therapies in high- or intermediate-high-risk PE patients.
It is important to note that this highly invasive procedure requires skilled surgeons and carries potential risks such as bleeding, infection, and haemodynamic instability. Therefore, it should only be considered when other treatment options are not feasible and the benefits outweigh the risks.
CATHETER-DIRECTED THERAPIES
In recent years, percutaneous catheter-based approaches have gained attention as an alternative to anticoagulation, systemic thrombolysis, and surgical embolectomy, due to their lower risk and potential benefits. These techniques involve endovascular techniques to disrupt, fragment, or remove an occlusive thrombus, or locally deliver reduced doses (i.e., one-third) of thrombolytic agents with a lower risk of bleeding compared to systemic administration41. While complete thrombus removal is not always necessary, the primary goal should be to stabilise the patient’s haemodynamics, as attempting to remove all clots at once can increase the risk of adverse events such as contrast-associated kidney injury, access-related vascular complications, arterial wall damage, or device-specific complications2242.
These approaches provide a minimally invasive treatment option for high-risk PE patients who have a contraindication to systemic thrombolysis or in whom this therapy has failed. Factors such as overall patient condition, operator experience, local availability, and thrombus burden and location (e.g., in the main or lobar ramus) should be considered when selecting the appropriate approach43. Procedural success rates for catheter-directed therapies (defined as haemodynamic stabilisation, correction of hypoxia and survival to hospital discharge) are reported at around 87%, with low rates of major bleeding complications (0.35% for intracranial haemorrhage and 4.65% for major bleeding or vascular injury)1541444546.
Importantly, high-quality evidence from randomised controlled trials is lacking to support the efficacy and safety of these approaches. While percutaneous catheter-based approaches hold promise as an alternative to traditional treatments, current guidelines do not recommend them as a first choice for any PE risk category (Figure 1).
Percutaneous devices
Percutaneous approaches to PE treatment include CDT and mechanical thrombectomy (e.g., thrombus fragmentation and rotational thrombectomy, rheolytic thrombectomy, and aspiration embolectomy) (Table 1, Central illustration).
Table 1. Main current catheter-based options for acute pulmonary embolism.
| Device | Mechanismof thrombus removal | Technical details | Vascular access | EU/US certificate for PE therapy | Pros | Cons |
|---|---|---|---|---|---|---|
| Pigtail catheters, peripheral balloon catheters | Mechanical fragmentation | Diameters: 6 and 8 Fr | F/J | Not applicable | Atraumatic, easily available, cost-effective | Risk of distal embolisation |
| Cragg-McNamara (Medtronic) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 40, 65, 100, and 135 cmTreatment zones: 5, 10, 20, 30, 40, and 50 cm | F | Yes | No guidewire needed for infusion | Requires 12-24 hours for thrombolytic infusion |
| Fountain Infusion Systems (Merit Medical) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 5, 10, 20, 30, 40, and 50 cm | F | No | Cost-effective | Limited clinical data |
| Uni-Fuse (AngioDynamics) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 2, 5, 10, 15, 20, 30, 40, and 50 cm | F | Yes | Even distribution of thrombolytic agent | Requires 12-24 hours for thrombolytic infusion |
| Pulse-Spray Infusion System (AngioDynamics) | Thrombolytic infusion | Diameters: 3, 4, and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 2, 5, 10, 15, 20, 30, 40, and 50 cm | F | No | Even distribution of thrombolytic agent.Short duration of infusion | Limited clinical data |
| BASHIR (Thrombolex) | Mechanical fragmentation, aspiration and thrombolytic infusion | Diameter: 7 FrLength: 92.5 cmTreatment zone: 12.5 cm | F | No | Delivery of thrombolytic agent at multiple points on the thrombus | Limited clinical data |
| EkoSonic(Boston Scientific) | Ultrasound-assisted thrombolysis (USAT) | Diameters: 5.4 and 7.8 FrLengths: 106 and 135 cmTreatment zones: 6, 8, 12, 16, 18, 20, 24, 30, 40, and 50 cm | F/J | Yes | Ultrasounds may enhance the thrombolytic effect by disaggregating fibrin strands. Low dosage of thrombolytic agent needed | Expensive.Benefit from ultrasound power still uncertain |
| Aspirex(Becton Dickinson) | Mechanical fragmentation and aspiration | Diameters: 6, 8, and 10 FrLengths: 85, 110, and 135 cm | F | Yes in EU, no in US | Easy to use, no thrombolysis needed | Possibly only effective in fresh thrombi |
| AngioJet(Boston Scientific) | Rheolytic thrombectomy with the option of thrombolytic injections (Power Pulse) | Diameters: 6 and 8 FrLength: 120 cmFlow rate: 60 ml/min | F/J | Yes in EU, FDA black box label* | Double action of thrombus fragmentation and aspiration, with optional thrombolysis | Systemic complications |
| AngioVac (AngioDynamics) | Aspiration with a veno-venous bypass | Diameters: 18 and 22 Fr | F/J | No** | Limited blood loss. Effective on large, organised right heart thrombus | Requires perfusion team. Contraindicated in chronic PE |
| AlphaVac (AngioDynamics) | Aspiration independent from circulatory support | Diameters: 18 and 22 FrLengths: 77 and 105 cmAngles: 20°, 85°, and 180° | F/J | No | Limited blood loss.No need for perfusion team | Limited clinical data. Contraindicated in chronic PE |
| FlowTriever(Inari Medical) | Aspiration with the option of mechanical fragmentation | Diameters: 16, 20, and 24 FrLengths: 90 and 113 cmCatheter sizes: S (6-10 mm), M (11-14 mm), L (15-18 mm), XL (19-25 mm) | F | Yes | Effective on large volumes of thrombi. Aspirated blood can be filtered and reinfused (FlowSaver system) | Difficult to reach distal PA branches due to size and rigidity |
| Indigo (Penumbra) | Aspiration with mechanical fragmentation | Diameters: 12 and 16 FrLengths: 80, 100 and 115 cm | F/J | Yes | Easy to reach distal PA branches due to flexibility. Lightning system reduces blood loss due to a thrombus-detection technology that differentiates between clot and blood | No possibility to filter and reinfuse aspirated blood. Possibly only effective in fresh thrombi |
| *Due to reports of bradycardia and asystole secondary to haemolysis and release of adenosine during rheolytic thrombectomy of pulmonary artery thrombus. Haemoglobinuria and renal insufficiency have also been reported. **FDA-cleared for the removal of undesirable intravascular material. EU: European Union; F: femoral; FDA: U.S. Food and Drug Administration; Fr: French; J: jugular; PA: pulmonary artery; PE: pulmonary embolism; US: United States | ||||||
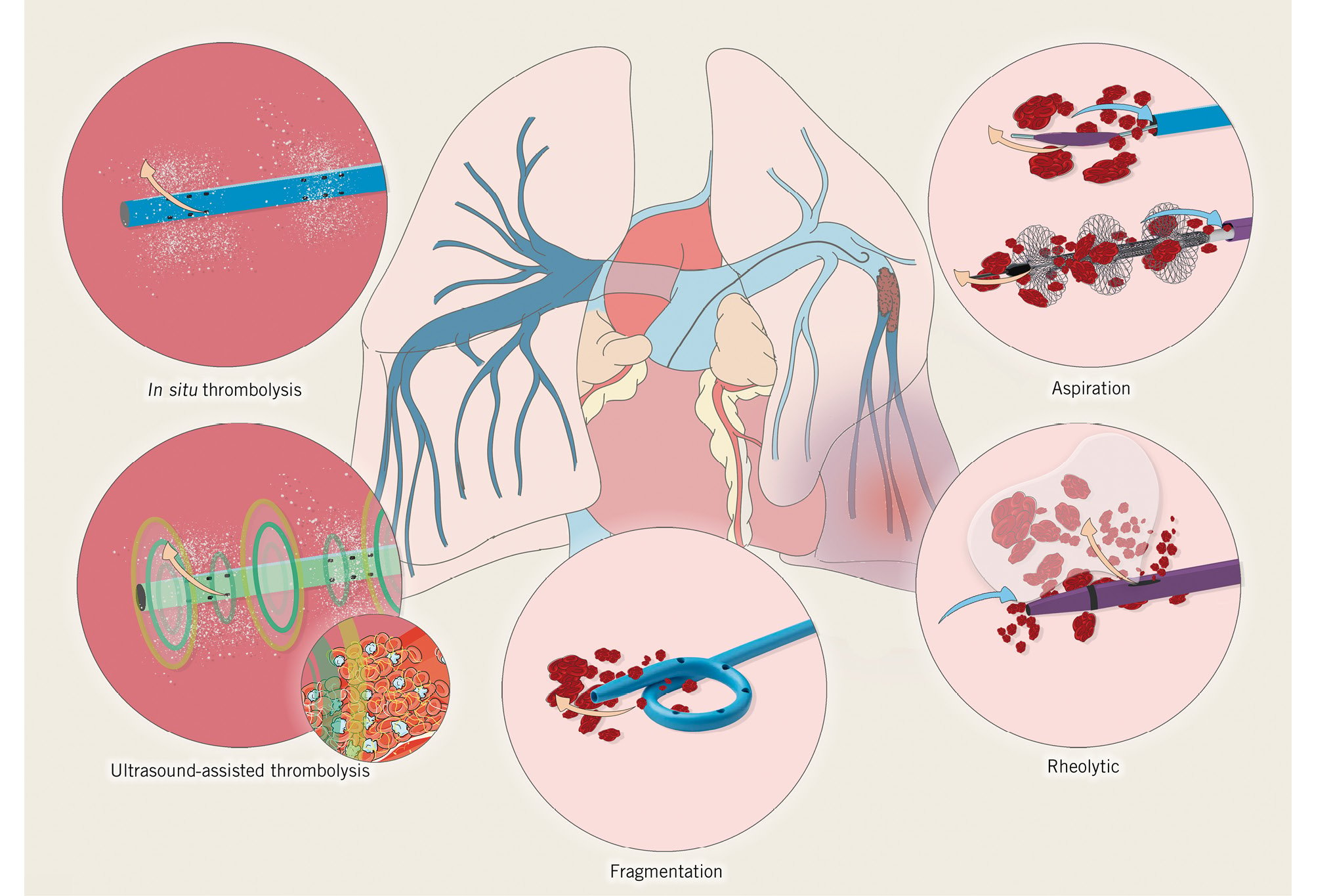
Central illustration. Interventional options for the treatment of acute pulmonary embolism. Percutaneous approaches to pulmonary embolism treatment include catheter-directed thrombolysis techniques (dark pink circles) and mechanical thrombectomy (light pink circles), which includes thrombus fragmentation, aspiration embolectomy, and rheolytic thrombectomy. These techniques are often used in combination with thrombolytic agents to increase efficacy and reduce bleeding complications. Catheter-directed thrombolysis involves a dedicated side-hole catheter that delivers a low-dose thrombolytic drug directly into the pulmonary artery or thrombus. Mechanical catheter fragmentation of thrombus can be performed prior to or during drug injection to enhance the efficacy of the treatment. Dedicated catheters with side holes for thrombolytic injection include Uni-Fuse and Cragg-McNamara. Ultrasound-assisted thrombolysis combines local thrombolysis with the delivery of ultrasound energy. The EkoSonic endovascular system is a catheter that has two lumens: one containing a filament equipped with multiple ultrasound transducers emitting pulsed high-frequency, low-energy ultrasound waves; and the other with multiple holes along its length to deliver the thrombolytic agent. Thrombus fragmentation with a pigtail catheter is the most basic and widely used technique due to its simplicity and low cost. Rheolytic thrombectomy uses pressurised fluid to disrupt blood clots and a vacuum to actively remove debris, with the option of thrombolytic injections. Aspiration embolectomy aims to restore haemodynamics by removing the thromboembolic burden and preventing distal embolisation. The FlowTriever system is a large lumen aspiration device that includes a large-bore aspiration catheter, a 60 ml aspiration syringe, and 3 self-expanding nitinol mesh discs; the discs are required in up to 25% of cases when conventional aspiration is unsuccessful. The Indigo system has a smaller, more flexible profile, connected to a continuous suction vacuum system, and a separator wire with a soft dedicated tip in the catheter lumen to disrupt the thrombus and facilitate aspiration.
CATHETER-DIRECTED THROMBOLYSIS
CDT utilises a catheter, a pigtail or, most commonly, a dedicated side-hole catheter to deliver a low-dose thrombolytic drug directly into the thrombotic pulmonary arteries. By doing so, CDT increases the thrombus surface area exposed to the thrombolytic agent while minimising the phenomenon of blood shunting towards the unobstructed pulmonary segments. Additionally, mechanical catheter thrombus fragmentation can be performed prior to or during drug injection to enhance the efficacy of the treatment. This process induces the peripheral dispersal of the thrombus fragments, leading to the rapid improvement of haemodynamics47. CDT aims to maximise thrombolytic efficacy while reducing bleeding complications. This is achieved by using a reduced dose of thrombolytic agent, compared with systemic thrombolysis. Furthermore, CDT has been proven to be the least expensive technique among all percutaneous approaches48.
Ultrasound guidance is used to achieve access via the internal jugular or common femoral vein with a 5-7 Fr sheath. If the thrombus burden requires dual catheter infusion to both pulmonary arteries, a second access in the same vein may be obtained. Several catheters, including straight or angled pigtail catheters, balloon catheters, or Cobra catheters (for the right pulmonary artery), can be advanced over a guidewire and manipulated through the right atrium and right ventricle to access the pulmonary circulation. Then the catheter is exchanged for a multiside-hole infusion catheter with an infusion length of 5 cm to 10 cm, depending on the clot burden identified at the pulmonary angiography or computed tomography.
Dedicated catheters with side holes for thrombolytic injection include Uni-Fuse (AngioDynamics; 4 Fr or 5 Fr), Cragg-McNamara (Medtronic; 4 Fr or 5 Fr), or the Pulse-Spray infusion system (AngioDynamics; 3 Fr, 4 Fr or 5 Fr)49. The BASHIR endovascular catheter (Thrombolex) differs from the others because of its larger size (7 Fr) and the presence, at the distal segment of the device, of a basket that is made up of mini-infusion catheters and expands within the thrombus. All these systems share the common indication of administering fluids, including thrombolytic agents and contrast media, into the peripheral vasculature50.
Once the infusion catheter is in place, a bolus of a thrombolytic drug (4-6 mg) is administered before starting the infusion. Dosing regimens may vary among centres, but they are usually 0.5-1 mg/h of alteplase per catheter, with the total dose not exceeding 30 mg (1/3-1/4 of the systemic dose) for about 12-24 hours under monitoring41. At the end of the infusion, the catheters and sheaths may be removed at bedside, without a need for repeat imaging2243. The infusion should be stopped in case of major bleeding or evidence of haemoÂdynamic improvement. In unstable patients, the goal of CDT is not complete thrombus removal but rather downstaging from high-risk to intermediate-risk PE.
One development in these standard infusion catheters is ultrasound-assisted thrombolysis (USAT), which combines local thrombolysis with the delivery of ultrasound energy. The EkoSonic endovascular system (Boston Scientific) is a catheter with two lumens: one containing a filament equipped with multiple ultrasound transducers emitting pulsed high-Âfrequency, low-energy ultrasound waves (2 MHz) and the other with multiple holes along its length to deliver the thrombolytic agent51. The ultrasound waves have the potential to unwind and disaggregate the fibrin strands, thus enhancing the thrombolytic effect by exposing more drug receptor sites52.
Compared to standard CDT, USAT is more expensive but achieves increased thrombolytic drug penetration at a lower dose over a shorter duration. Two different French sizes are available: 5.4 Fr for EkoSonic and 7.8 Fr for EkoSonic+ (which has 50% more ultrasound power and 32% more lysis than the conventional EkoSonic device). USAT has been investigated in several randomised trials and prospective registries (ClinicalTrials.gov: NCT03426124) and has obtained U.S. Food and Drug Administration (FDA) approval and European conformity (CE) marking specifically for the treatment of PE515354.
As noted, CDT can be used in combination with other techniques, such as thrombus aspiration or fragmentation, to increase the surface area exposed to fibrinolytics, resulting in a synergistic enhancement of the thrombolytic effect. Rare complications such as distal embolisation, intraprocedural haemodynamic or respiratory decompensation, intracranial haemorrhage, non-intracranial major bleeding and pulmonary haemorrhage have been reported in the FDA Manufacturer and User Facility Device Experience (MAUDE) database5556.
MECHANICAL THROMBECTOMY
Mechanical thrombectomy, including catheter-directed thrombus fragmentation, and rotational, rheolytic and aspirational embolectomy, uses different devices that are usually combined with a thrombolytic drug infusion to debulk the thromboembolic obstruction and thereby restore pulmonary perfusion (Table 1).
Table 1. Main current catheter-based options for acute pulmonary embolism.
| Device | Mechanismof thrombus removal | Technical details | Vascular access | EU/US certificate for PE therapy | Pros | Cons |
|---|---|---|---|---|---|---|
| Pigtail catheters, peripheral balloon catheters | Mechanical fragmentation | Diameters: 6 and 8 Fr | F/J | Not applicable | Atraumatic, easily available, cost-effective | Risk of distal embolisation |
| Cragg-McNamara (Medtronic) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 40, 65, 100, and 135 cmTreatment zones: 5, 10, 20, 30, 40, and 50 cm | F | Yes | No guidewire needed for infusion | Requires 12-24 hours for thrombolytic infusion |
| Fountain Infusion Systems (Merit Medical) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 5, 10, 20, 30, 40, and 50 cm | F | No | Cost-effective | Limited clinical data |
| Uni-Fuse (AngioDynamics) | Thrombolytic infusion | Diameters: 4 and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 2, 5, 10, 15, 20, 30, 40, and 50 cm | F | Yes | Even distribution of thrombolytic agent | Requires 12-24 hours for thrombolytic infusion |
| Pulse-Spray Infusion System (AngioDynamics) | Thrombolytic infusion | Diameters: 3, 4, and 5 FrLengths: 45, 90, and 135 cmTreatment zones: 2, 5, 10, 15, 20, 30, 40, and 50 cm | F | No | Even distribution of thrombolytic agent.Short duration of infusion | Limited clinical data |
| BASHIR (Thrombolex) | Mechanical fragmentation, aspiration and thrombolytic infusion | Diameter: 7 FrLength: 92.5 cmTreatment zone: 12.5 cm | F | No | Delivery of thrombolytic agent at multiple points on the thrombus | Limited clinical data |
| EkoSonic(Boston Scientific) | Ultrasound-assisted thrombolysis (USAT) | Diameters: 5.4 and 7.8 FrLengths: 106 and 135 cmTreatment zones: 6, 8, 12, 16, 18, 20, 24, 30, 40, and 50 cm | F/J | Yes | Ultrasounds may enhance the thrombolytic effect by disaggregating fibrin strands. Low dosage of thrombolytic agent needed | Expensive.Benefit from ultrasound power still uncertain |
| Aspirex(Becton Dickinson) | Mechanical fragmentation and aspiration | Diameters: 6, 8, and 10 FrLengths: 85, 110, and 135 cm | F | Yes in EU, no in US | Easy to use, no thrombolysis needed | Possibly only effective in fresh thrombi |
| AngioJet(Boston Scientific) | Rheolytic thrombectomy with the option of thrombolytic injections (Power Pulse) | Diameters: 6 and 8 FrLength: 120 cmFlow rate: 60 ml/min | F/J | Yes in EU, FDA black box label* | Double action of thrombus fragmentation and aspiration, with optional thrombolysis | Systemic complications |
| AngioVac (AngioDynamics) | Aspiration with a veno-venous bypass | Diameters: 18 and 22 Fr | F/J | No** | Limited blood loss. Effective on large, organised right heart thrombus | Requires perfusion team. Contraindicated in chronic PE |
| AlphaVac (AngioDynamics) | Aspiration independent from circulatory support | Diameters: 18 and 22 FrLengths: 77 and 105 cmAngles: 20°, 85°, and 180° | F/J | No | Limited blood loss.No need for perfusion team | Limited clinical data. Contraindicated in chronic PE |
| FlowTriever(Inari Medical) | Aspiration with the option of mechanical fragmentation | Diameters: 16, 20, and 24 FrLengths: 90 and 113 cmCatheter sizes: S (6-10 mm), M (11-14 mm), L (15-18 mm), XL (19-25 mm) | F | Yes | Effective on large volumes of thrombi. Aspirated blood can be filtered and reinfused (FlowSaver system) | Difficult to reach distal PA branches due to size and rigidity |
| Indigo (Penumbra) | Aspiration with mechanical fragmentation | Diameters: 12 and 16 FrLengths: 80, 100 and 115 cm | F/J | Yes | Easy to reach distal PA branches due to flexibility. Lightning system reduces blood loss due to a thrombus-detection technology that differentiates between clot and blood | No possibility to filter and reinfuse aspirated blood. Possibly only effective in fresh thrombi |
| *Due to reports of bradycardia and asystole secondary to haemolysis and release of adenosine during rheolytic thrombectomy of pulmonary artery thrombus. Haemoglobinuria and renal insufficiency have also been reported. **FDA-cleared for the removal of undesirable intravascular material. EU: European Union; F: femoral; FDA: U.S. Food and Drug Administration; Fr: French; J: jugular; PA: pulmonary artery; PE: pulmonary embolism; US: United States | ||||||
THROMBUS FRAGMENTATION AND ROTATIONAL THROMBECTOMY
Pigtail thrombus fragmentation is the most basic and atraumatic technique, widely available and used because of its simplicity and low cost57. It previously accounted for about half of catheter-directed approaches but has been replaced by the advent of modern techniques58. In pigtail thrombus fragmentation, a modified pigtail catheter manually rotates around the guidewire that exits from a side hole59. Frequently, this technique can be facilitated by thrombus maceration performed with either peripheral balloons, which are typically sized smaller than the true arterial lumen diameter42, or with concomitant thrombolytic administration, which makes it difficult to isolate the benefit of mechanical therapy alone. These techniques may be helpful in patients who are in a hypotensive state and have a proximal occlusion, because recanalisation of the central embolic occlusion can rapidly provide some forward flow and partially decompress the RV until further treatment. However, the downstream dislocation of small thrombus fragments can worsen the obstruction, embolising in previously patent branches4259.
To overcome this issue, over-the-wire rotational thrombectomy systems combine mechanical clot fragmentation with a motor-driven, rotating, flexible sinusoidal tip placed directly into the thrombus and active negative-pressure removal of debris to prevent distal embolisation606162. Nevertheless, the rotational approach carries a risk of vascular wall injury. Studies of these techniques are generally small, and their effectiveness is poorly described.
RHEOLYTIC THROMBECTOMY
The AngioJet device (Boston Scientific) is a rheolytic system that uses pressurised fluid to disrupt blood clots and a vacuum to actively remove debris with the possibility of thrombolytic injection (via its patented Power Pulse feature)6364. The catheter has a double-lumen construction, with one lumen serving to inject saline solution under high pressure for thrombus fragmentation and the other to aspirate the saline solution, along with any blood clots (Bernoulli’s principle). Indications for rheolytic thrombectomy range from patients with acute myocardial infarction undergoing percutaneous coronary intervention to patients with DVT undergoing pharmacoÂmechanical catheter-directed venous thrombolysis656667. Adverse effects include transient haemolysis resulting in reversible haemoglobinuria. Moreover, a meta-analysis of 35 published series on the invasive treatment of massive PE found that rheolytic thrombectomy was associated with a higher incidence of bradyarrhythmia (e.g., asystole, atrioventricular blocks), usually following a prolonged activation time − possibly due to the release of adenosine, bradykinin or potassium subsequent to haemolysis − as compared with other invasive modalities57. As a result, the FDA has issued a “black box” warning regarding the device’s use in PE treatment. However, thrombolytic delivery can often result in a shorter treatment time and a faster restoration of flow, reducing the risk of complications686970.
ASPIRATION EMBOLECTOMY
Aspiration embolectomy aims to restore haemodynamics by removing the thromboembolic burden and preventing distal embolisation. Greenfield et al introduced suction embolectomy as a treatment for PE, using a 12 Fr catheter with a cup on its distal end and manual aspiration applied to the catheter hub71. Nowadays, the aspiration of large and organised thrombi is achieved through large-bore specialised catheters (8 Fr or greater) to enable greater vacuum effects. Three available aspiration systems have mainly been tested for the treatment of acute PE.
The AngioVac (AngioDynamics) was one of the first aspiration devices on the market, consisting of an extracorporeal veno-venous bypass system that simultaneously reinfuses filtered blood back into the patient using jugular and femoral accesses72. However, due to its contraindicated use in the pulmonary arteries and the need for perfusionist support, it was not considered optimal for PE extraction and was approved only for the removal of thrombi from the superior and inferior vena cava and from the right atrium73. More recently, the AlphaVac (AngioDynamics) was developed, which uses a manual multipurpose aspiration system with a deliverable cannula independent of circulatory support. The device is under investigation for PE indication in the ongoing APEX-AV study (ClinicalTrials.gov: NCT05318092).
The FlowTriever system (Inari Medical) is a large lumen aspiration device comprising various sizes and shapes. The system can be accessed via the internal jugular or femoral vein, preferably with ultrasound-guided puncture. A stiff wire with a short flexible tip is necessary for placement in a distal pulmonary artery. The system includes 3 large-bore aspiration catheters (16 Fr, 20 Fr, and 24 Fr), a 60 ml aspiration syringe, and 3 self-expanding nitinol mesh discs − ranging from 6 mm to 25 mm in diameter − that open inside the thrombus for further retraction. These disc catheters are required in up to 25% of cases when conventional aspiration techniques are unsuccessful74. The FlowTriever also features an external blood return system, called FlowSaver, consisting of a 40 micron filtration system which strains thrombi and returns blood to the patient. Three mechanical clot removal techniques can be performed: direct aspiration, the “lollipop” technique in which the clot is trapped in suction at the tip of the catheter, and the disc aspiration technique. Despite its versatility, the system is notable for its size and rigidity that can make it challenging to deliver or advance into distal vessels. Furthermore, there is a learning curve, and experienced operators are needed for optimal results.
The Indigo system (Penumbra) offers a smaller, more flexible profile, with 12 Fr and 16 Fr catheters available. This system is connected to a continuous suction vacuum system, and a separator wire with a soft dedicated tip is located in the catheter lumen to disrupt the thrombus and facilitate aspiration. The catheter can be advanced through the thrombus multiple times, permitting more extensive removal, and the smaller calibre of the catheter allows access to more distal clots, compared to the larger profile of the FlowTriever system. Furthermore, the recently developed computer-aided Lightning system (Penumbra) consists of an automatic valve control which, thanks to a microprocessor with a proprietary thrombus removal algorithm, helps the operator to identify thrombus location. Blood loss usually does not exceed 400 ml, rarely leading to the need for postprocedural transfusions75.
Both the FlowTriever and Indigo systems can be used in combination with local thrombolysis. Optimised introducer sheaths with a dedicated haemostasis valve are recommended to prevent blood loss during aspiration embolectomy.
Practical aspects of percutaneous treatment, evidence basis, and outlook
TIMING, MONITORING, AND IMAGING
When considering the use of percutaneous techniques, the proper timing of intervention is critical. High-risk patients necessitate immediate intervention, while intermediate-risk patients may tolerate a short delay. However, studies have shown that early interventions (i.e., within 24-48 hours of presentation) have better efficacy and safety compared to delayed interventions (i.e., >48 hours after presentation)535476. For high-risk patients, a recent European Society of Cardiology (ESC) protocol recommends initiating the treatment within 60 minutes of the diagnosis, or up to 90 minutes if the diagnosis is made in a centre that does not perform percutaneous treatment22. Continuous monitoring of vital signs, including oxygen saturation, systemic arterial and pulmonary pressure, and heart rhythm, is mandatory during the procedure to ensure that haemodynamic stabilisation is obtained77. Intraprocedural imaging is valuable to localise the clots and assess the embolic load.
EFFICACY, SAFETY, AND TECHNIQUE SELECTION
The decision to perform a percutaneous intervention for PE and the choice of technique must consider the trade-off between efficacy and safety. However, due to significant heterogeneity in patient characteristics, techniques used, and clinical outcomes across studies, this decision-making process is challenging. The available data suggest that catheter-directed treatments, assuming adequate operator expertise, can achieve haemodynamic stabilisation and in-hospital survival rates close to 90%, but these outcomes vary depending on patient presentation (high vs intermediate risk) and baseline characteristics (e.g., chronic kidney disease, bleeding risk)4146.
CDT may be considered a safe technique, with periprocedural bleeding being the most commonly reported complication, having an incidence of extracranial major bleeding that ranges from 1% to 9.2%41 and intracranial haemorrhage occurring in approximately 1% of cases842. Mechanical thrombectomy carries higher risks due to its larger and stiffer catheters that require broader movement, potentially causing trauma to pulmonary structures. Thrombus fragmentation during mechanical thrombectomy may also dislodge thrombi distally, resulting in increased RV afterload and worsened systolic function. Recent data provide some reassurance regarding the higher number of serious adverse events associated with rheolytic thrombectomy70. When considering the efficacy and safety of each procedure, minor complications such as access-related issues, infections, and acute kidney injury should also be taken into account during the planning of any interventional strategy414678.
INTERDISCIPLINARY COLLABORATION
The rapidly advancing landscape of innovative therapeutic approaches and interventional devices has posed increasing challenges in treatment decision-making. To address this, the concept of a multidisciplinary team involved in early decision-making and therapeutic selection has emerged. Pulmonary Embolism Response Teams (PERTs) have been proposed as a model for cross-speciality collaboration, enabling real-time case evaluations from diverse clinical and interventional perspectives to reach a consensus on treatment decisions798081. A typical PERT consists of emergency medicine physicians, interventional radiologists, cardiologists, pulmonologists, critical care specialists, and other healthcare professionals who collaborate to mitigate individual and intraspeciality biases in a real-time setting providing emergency care for PE patients. A growing body of evidence demonstrates that PERT activation is associated with lower 30- and 90-day mortality rates and reduced readmissions compared to cases without PERT activation8283. Interestingly, the implementation of PERTs has led to an increased utilisation of interventional strategies for intermediate-risk patients8283.
SUPPORTING EVIDENCE
Over the years, a series of clinical trials have provided evidence for various techniques and devices for catheter-directed therapy (Table 2, Table 3, Supplementary Figure 1, Supplementary Figure 2, Supplementary Figure 3, Supplementary Figure 4). Overall, the major available studies of CDT and aspiration embolectomy provide an initial evidence base for the use of catheter-based therapies for acute management of PE. These trials not only highlight the progress in the field, but they also suggest the potential for continued advancements and innovations in the future.
Table 2. Key studies of catheter-directed thrombolysis.
| Study | Devices | Design | Sample | Population | Intervention | Control | Efficacy outcome | Safety outcomes | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| ULTIMA53(NCT01166997), 2013 | EkoSonic | Randomised, open-label | 59 | Intermediate-risk PE | Anticoagulation plus tPA-USAT (10 mg) | Anticoagulation monotherapy | ∆RV/LV ratio at 24 h: 0.30±0.20 vs 0.03±0.16 (p<0.001) | 0 deaths, 0 major bleeds, 3 minor bleeds at 90 days | 90 days |
| SEATTLE II51(NCT01513759), 2015 | EkoSonic | Single-arm | 150 | Intermediate-high-risk PE | Anticoagulation plus tPA-USAT (12-24 mg) | - | ∆RV/LV ratio at 48 h: 0.42±0.36 (p<0.0001) | 7 deaths, 15 major bleeds at 30 days | 30 days |
| OPTALYSE PE54(NCT02396758), 2018 | EkoSonic | Randomised, open-label | 101 | Intermediate-risk PE | Anticoagulation plus tPA-USAT (4 mg, 6 mg, or 12 mg) | Compared 4 tPA regimens* | RV/LV ratio reduced in all arms at 48±6 h | 5 major bleedsat 72 h | 365 days |
| SUNSET sPE84 (NCT02758574), 2021 | EkoSonic vs Cragg-McNamara or Uni-Fuse | Randomised, single-blind | 81 | Intermediate-risk PE | Anticoagulation plus tPA-USAT (4-8 mg) | Anticoagulation plus CDT | ∆RV/LV ratio at 48 h: 0.37±0.34 vs 0.59±0.42 (p=0.01) | 2 major bleeds, 3 minor bleeds and 1 in-hospital death | 90 days |
| CANARY85 (NCT05172115), 2022 | Cragg-McNamara | Randomised, open-label | 94 | Intermediate-high-risk PE | Anticoagulation plus CDT (12-24 mg) | Anticoagulation monotherapy | ∆RV/LV ratio reduced at 3 months: 0.7 vs 0.8 (p=0.01) | 1 BARC Type 3a major bleed | 90 days |
| RESCUE50 (NCT04248868), 2022 | BASHIR | Single-arm | 109 | Intermediate-risk PE | Anticoagulation plus CDT (7-14 mg) | - | ∆RV/LV ratio at 48 h: 0.56±0.41 (p<0.0001) | 1 death, 3 major bleeds at 30 days | 30 days |
| Kroupa et al86 (pilot study), 2022 | Cragg-McNamara | Randomised, open-label | 23 | Intermediate-high-risk PE | Anticoagulation plus CDT (20 mg) | Anticoagulation monotherapy | ∆RV/LV ratio at 48 h: 0.88±0.16 vs 1.42±0.44 (p=0.01) | 0 BARC Type 5 or 3c major bleeds | 30 days |
| * Arm 1 (4 mg/lung/2 h), arm 2 (4 mg/lung/4 h), arm 3 (6 mg/lung/6 h), and arm 4 (12 mg/lung/6 h). BARC: Bleeding Academic Research Consortium; CDT: catheter-directed thrombolysis; h: hours; LV: left ventricular; PE: pulmonary embolism; RV: right ventricular; tPA: tissue plasminogen activator; USAT: ultrasound-assisted thrombolysis | |||||||||
Table 3. Key studies of aspiration embolectomy.
| Trial | Devices | Design | Sample | Population | Intervention | Control | Efficacy outcome | Safety outcomes | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| FLARE [74](NCT02692586), 2019 | FlowTriever | Single-arm | 106 | Intermediate-risk PE | Anticoagulation plus FlowTriever | - | ∆RV/LV ratio at 48 h: 0.41±0.05 (p<0.0001) | All-cause death: 0; major bleeding: 0.9% at 48 h | 30 days |
| EXTRACT-PE [75](NCT03218566), 2021 | Indigo | Single-arm | 119 | Intermediate-risk PE | Anticoagulation plus Indigo | - | ∆RV/LV ratio at 48 h: 0.43±0.26 (p<0.0001) | All-cause death: 1.1%; major bleeding: 1.6% at 48 h | 30 days |
| FLAME [89](NCT04795167), 2023 | FlowTriever | Prospective, non-randomised | 104 | High-risk PE | Anticoagulation plus FlowTriever | Other therapies | Composite of all-cause mortality, clinical deterioration, bailout, and major bleeding: 17% vs 63.9% | All-cause death: 1.9% vs 29.5%; major bleeding: 11.3% vs 24.6% | In hospital |
| h: hours; LV: left ventricular; PE: pulmonary embolism; RV: right ventricular | |||||||||
CATHETER-DIRECTED THROMBOLYSIS
The ULTIMA trial (ClinicalTrials.gov: NCT01166997) was a landmark study that assessed the efficacy and safety of USAT in 59 patients with acute intermediate-risk PE and demonstrated a significant reduction in RV dysfunction at 24 hours, with no increase in bleeding risk (i.e., no major bleeding and 3 cases of minor bleeding) compared to systemic anticoagulation alone53. OPTALYSE PE (ClinicalTrials.gov: NCT02396758) was built on the success of the ULTIMA trial and showed that even lower doses (4-12 mg) and shorter durations (2-6 hours) of thrombolytic therapy were effective in improving RV function without increasing the bleeding risk54. Conversely, in the single-arm SEATTLE II trial (ClinicalTrials.gov: NCT01513759), the administration of higher thrombolytic doses (24 mg) in 150 PE patients was associated with a higher incidence of major bleeding (10%)51. In the SUNSET-sPE trial (ClinicalTrials.gov: NCT02758574), the EkoSonic USAT was evaluated in comparison to other devices for CDT (Uni-Fuse and Cragg-McNamara) in 81 patients with intermediate-risk PE84. Although the trial did not meet its primary efficacy endpoint (thrombus burden reduction using the modified Miller scoring system and reduction in RV dysfunction, both measured by computed tomography), it demonstrated a low incidence of major bleeding84. The CANARY Trial (ClinicalTrials.gov: NCT05172115) aimed at further evaluating the safety and efficacy of catheter-directed therapy in patients with intermediate-high-risk PE and, although it was prematurely stopped because of the COVID-19 pandemic, it confirmed, in 94 of the 288 initially planned patients, the positive results of previous trials85. Kroupa et al sought to confirm the safety and efficacy of CDT compared with systemic anticoagulation in a small, pilot, randomised trial, and no intracranial or life-threatening bleeding was reported in the 23 PE patients randomised86. Preliminary findings from the 2021 KNOCOUT PE registry (ClinicalTrials.gov: NCT03426124) show that 489 intermediate-high- to high-risk PE patients treated with USAT had a 2.5% major bleeding rate and no intracerebral haemorrhages at 30 days. The average thrombolytic dose was 17.9 mg, and the infusion time was 10.4 hours. A 38% reduction in RV dysfunction was observed at the 3-month follow-up, indicating lower recurrent VTE rates (0.8%) than previously reported87.
ASPIRATION EMBOLECTOMY
The FLARE Study was the first single-arm clinical trial supporting the use of the FlowTriever device in patients with acute PE, demonstrating improvements in RV function, haemodynamic stability, and reduced bleeding risk compared to standard anticoagulation therapy; also, in this study, less than half of patients (41.3%) needed intensive care unit monitoring after the intervention74. The ongoing FLASH registry corroborated these findings, reporting safety and efficacy data from the first 800 US patients (8% high-risk PE and 92% intermediate-risk PE)88. The FlowTriever device improved haemodynamic parameters and functional outcomes, but, after 30 days, 6 deaths occurred (none associated to the device, but 2 deaths were PE related), and the readmission rate was 6.2%. Recently, the FLAME trial, a non-randomised study, compared high-risk PE patients treated with the FlowTriever device and those treated with other strategies, mainly systemic thrombolysis or anticoagulation alone89. Differently from previous trials, the primary endpoint was a composite of in-hospital clinical outcomes, including all-cause mortality, clinical deterioration, major bleeding, and bailout therapy. The primary endpoint was reached in 17.0% of patients in the FlowTriever arm and in 63.9% of those in the context arm, with no difference between systemic thrombolytics (66.7%) and anticoagulation alone (71.4%). Specifically, in-hospital mortality in the FlowTriever and context groups occurred in 1.9% and 29.5% of patients, respectively. The EXTRACT-PE trial evaluated the safety and efficacy of the first-generation Indigo aspiration system for patients with acute PE. The trial demonstrated significant improvements in haemodynamic parameters (27% reduction of RV/left ventricular ratio) and a favourable safety profile (1.7% rate of major bleeding), further supporting the use of aspiration embolectomy as an alternative to standard anticoagulation therapy75.
OTHER STUDIES
Several nationwide or multicentre registries have demonstrated the feasibility of catheter-directed treatments in different PE subsets44909192939495969798. A recent network meta-analysis including 81,705 patients in 45 studies, both randomised and observational, compared the efficacy and safety of CDT, anticoagulation alone, and systemic thrombolysis in patients with acute PE99. CDT had lower mortality (odds ratio [OR] 0.55, 95% confidence interval [CI]: 0.39-0.80) but higher major bleeding (OR 1.84, 95% CI: 1.10-3.08) and higher haemorrhagic stroke (OR 1.51, 95% CI: 0.75-3.04) risks compared to anticoagulation. However, when compared with systemic thrombolysis, CDT showed not only lower mortality (OR 0.48, 95% CI: 0.34-0.68) but also lower stroke risk (OR 0.66, 95% CI: 0.50-0.88). Moreover, results were consistent when focusing on studies involving intermediate-risk PE.
Ongoing trials and future directions
Several ongoing clinical trials are investigating various percutaneous techniques for the management of PE in intermediateÂ-high-risk populations (Table 4).
The PE-TRACT trial (ClinicalTrials.gov: NCT05591118), a phase 3, assessor-blinded trial, will evaluate the short-term safety and efficacy of catheter-directed therapies (CDT or mechanical thrombectomy) compared to standard anticoagulation protocols in 500 PE patients.
Three specific trials are comparing CDT with standard anticoagulation protocols. The HI-PEITHO (ClinicalTrials.gov: NCT04790370) and PRAGUE-26 (ClinicalTrials.gov: NCT05493163) trials are enrolling 406 and 558 patients, respectively, to assess the use of heparin in combination with USAT and standard anticoagulation protocols, focusing on reducing the 7-day incidences of all-cause death, haemodynamic decompensation, and PE recurrence. The STRATIFY study (ClinicalTrials.gov: NCT04088292), a singleÂ-blind, phase 3 trial, is comparing USAT, low-dose systemic thrombolysis, and standard anticoagulation protocol, randomising 210 patients in a 3-arm design and aiming to demonstrate a reduction in Miller score, as assessed by pulmonary computed tomography at 96 hours.
Furthermore, direct mechanical thrombectomy devices are being evaluated. An ongoing phase 1 trial (ClinicalTrials.gov: NCT05612854) is examining the safety and efficacy of catheter-directed therapies including CDT, pigtail mechanical fragmentation and aspiration embolectomy using the Indigo system, compared to standard anticoagulation, in 200 patients. The STORM-PE trial (ClinicalTrials.gov: NCT05684796) is comparing patients treated with the recent 12 Fr-size Indigo catheter to those treated with standard anticoagulation protocols.
The PEERLESS Study (ClinicalTrials.gov: NCT05111613) is an open-label, randomised trial directly comparing catheterÂdirected therapies for PE, specifically investigating the short-term outcomes of the FlowTriever system compared to CDT in 550 intermediate-high-risk patients, of which 150 patients have an absolute contraindication to thrombolytics. In PEERLESS II (ClinicalTrials.gov: NCT06055920), 1,200 intermediate-risk patients will be randomised to FlowTriever treatment or standard anticoagulation alone to assess 30-day haemodynamic decompensation and all-cause hospital readmission, and 3-month all-cause death, PE-related mortality and major bleeding.
In addition to these trials for percutaneous PE treatment, another ongoing trial (ClinicalTrials.gov: NCT05127915) is exploring the use of absorbable caval filters for the percutaneous prevention of PE, evaluating the safety and efficacy of a new absorbable vena cava filter in high-risk patients.
The results of these trials will provide valuable insights into the safety and efficacy of percutaneous techniques for PE treatment and prevention. If proven safe and effective, these techniques may become the preferred approach for managing PE in specific patient populations. Overall, the future outlook for percutaneous treatment of PE is promising, and these ongoing trials will further advance our understanding of this innovative approach to PE management.
Table 4. Ongoing randomised trials of pulmonary embolism treatment enrolling 100 patients or more.
| Trial | Design | Sample | Population | Intervention | Control | Primary outcomes | Follow-up |
|---|---|---|---|---|---|---|---|
| HI-PEITHO (NCT04790370) | Single-blind, phase 4 | 406 | Intermediate-high-risk PE | USAT | Standard anticoagulation | All-cause death, haemodynamic decompensation, recurrent PE | 7 days |
| NCT05612854 | Open-label, phase 1 | 200 | Intermediate-high-risk PE | Fragmentation, aspiration | Standard anticoagulation | MACE | 2 years |
| PE-TRACT (NCT05591118) | Open-label, phase 3 | 500 | Intermediate-high-risk PE | CDT or mechanical thrombectomy | Standard anticoagulation | Peak oxygen consumption, NYHA FC, major bleeding | 7 days,3 months, 12 months |
| PEERLESS (NCT05111613) | Open-label | 550 | Intermediate-high-risk PE | Aspiration embolectomy (FlowTriever system) | CDT | All-cause death, intracranial haemorrhage, major bleeding, haemodynamic decompensation | 7 days |
| PEERLESS II (NCT06055920) | Open-label | 1,200 | Intermediate-high-risk PE | Aspiration embolectomy (FlowTriever system) | Standard anticoagulation | Haemodynamic decompensation, all-cause hospital readmission, bailout therapy | 30 days |
| PRAGUE-26 (NCT05493163) | Open-label, phase 4 | 558 | Intermediate-high-risk PE | CDT | Standard anticoagulation | All-cause death, haemodynamic decompensation, recurrent PE | 7 days |
| STORM-PE (NCT05684796) | Open-label | 100 | Intermediate-high-risk PE | Aspiration embolectomy (Indigo system) | Standard anticoagulation | Change in right ventricle/left ventricle ratio | 48 hours |
| STRATIFY (NCT04088292) | Single-blind, phase 3, 1:1:1 | 210 | Intermediate-high-risk PE | USAT or low-dose thrombolysis | Standard anticoagulation | Miller score | 96 hours |
| CDT: catheter-directed thrombolysis; MACE: major adverse cardiovascular events; NYHA FC: New York Heart Association Functional Class; PE: pulmonary embolism; USAT: ultrasound-assisted thrombolysis | |||||||
Conclusions
Percutaneous catheter-based therapies for PE show promising advancements as an alternative to traditional treatments, but there is currently limited high-quality evidence to support their efficacy and safety. Indeed, current guidelines do not recommend them as a first choice for any PE risk category.
However, as further catheter-directed options are available, more data accrue and safety profiles improve, there may be a shift towards a “primary percutaneous pulmonary intervention” approach, similar to what occurred many years ago with ST-elevation myocardial infarction. Indeed, the expanding range of treatment options for PE can offer the opportunity to overcome the significant limitations of systemic thrombolysis, thus reducing the hidden bleeding burden that impacts on mortality outcomes. The development of a PE treatment network can facilitate the efficient and appropriate transfer of high-risk PE patients to high-volume centres where a multidisciplinary response team can offer a comprehensive, tailored approach to treatment.
Improving survival among high-risk PE patients is a priority, and the greater availability of percutaneous options highlights the importance of an endovascular approach. Engendering high-quality evidence through ongoing clinical trials will be crucial in determining the role of percutaneous therapies in the management of PE.
Guest Editor
This paper was guest edited by Franz-Josef Neumann, MD, PhD, FESC; Department of Cardiology and Angiology II, University Heart Center Freiburg - Bad Krozingen, Bad Krozingen, Germany.
Conflict of interest statement
D. Capodanno has received speaker honoraria from Daiichi Sankyo and Sanofi; and institutional payments from Medtronic. The other authors have no conflicts of interest to declare. The Guest Editor reports lecture fees paid to his institution from Amgen, Bayer Healthcare, Biotronik, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, Edwards Lifesciences, Ferrer, Pfizer, and Novartis; consultancy fees paid to his institution from Boehringer Ingelheim; and grant support from Bayer Healthcare, Boston Scientific, Biotronik, Edwards Lifesciences, GlaxoSmithKline, Medtronic, and Pfizer.
Supplementary data
To read the full content of this article, please download the PDF.

