Abstract
Aims: The aim of this study was to address the association of lipid profiles with periprocedural myocardial infarction (pMI) after elective percutaneous coronary intervention (PCI).
Methods and results: Of the 302 consecutive patients who received elective PCI at the Chubu Rosai Hospital, Nagoya, Japan between June 2009 and December 2010, data from 231 native coronary lesions were analysed. Various biomarkers including serum troponin T (TnT), eicosapentaenoic acid (EPA), arachidonic acid (AA), and low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol were measured at baseline and at 18 hrs after PCI. pMI was defined as a post-procedural increase of TnT >3 times above the upper normal limit. Patients with pMI had significantly lower EPA/AA (0.25 [0.19-0.28] vs. 0.45 [0.21-0.62], p<0.001) and higher LDL/HDL cholesterol (3.00±1.05 vs. 2.36±0.90, p=0.008) than patients without pMI. On multivariate logistic analysis, EPA/AA per 0.1 increase (hazard ratio [HR] 0.62, 95% CI: 0.43-0.88, p=0.007), LDL/HDL (HR 1.92, 95% CI: 1.15-3.19, p=0.012), stented length (HR 1.40, 95% CI: 1.07-1.83, p=0.015), and the presence of unstable angina pectoris (UAP) (HR 8.89, 95% CI: 2.83-27.9, p<0.001) were significantly and independently associated with the incidence of pMI.
Conclusions: EPA/AA and LDL/HDL were significantly associated with pMI after PCI, creating the possibility of a new therapeutic target of pMI.
Introduction
A number of studies have shown a correlation between periprocedural myocardial infarction (pMI) following elective percutaneous coronary intervention (PCI) and adverse clinical outcome1,2. The predictors of pMI can be broadly categorised as patient-related, procedure-related, and lesion-related risk factors3. The major risk factors, in terms of both frequency and potency, are diabetes mellitus, renal failure, left ventricular dysfunction, complex lesion, and complex procedures4-6. In addition, coronary plaque characteristics in target lesions are responsible for the occurrence of pMI7. Although the number of microemboli correlates positively with the severity of myocardial microvascular dysfunction and myonecrosis, there is considerable overlap with regard to the magnitude of plaque microembolisation between patients with and those without pMI8,9. This finding suggests that factors other than the burden of plaque microembolisation also influence the likelihood of pMI, such as the release of vasoactive factors from the atherosclerotic plaque and platelet activation10.
There are several pleiotropic effects of n-3 polyunsaturated fatty acids (PUFAs), such as inhibiting platelet aggregation11,12, vasodilation13,14, anti-atherosclerosis effects15,16 and effects on endothelial function17. In addition, we have recently reported the association of decreased serum PUFA levels with coronary plaque instability18. These various beneficial effects of PUFA may have an impact on the prevention of pMI. Therefore, in the present study we examined the potential value of serum PUFA levels for predicting pMI following an elective PCI in patients with stable angina pectoris (SAP) and unstable angina pectoris (UAP), taking into account possible related clinical and procedural factors.
Methods
PATIENTS AND STUDY DESIGN
This study was an observational investigation involving consecutive patients who underwent an elective PCI for SAP or UAP between June 2009 and December 2010. The exclusion criteria were as follows: elevated pre-procedural biomarkers, multivessel stenting in a single procedure, chronic total occlusion, angioplasty with atherectomy, occlusion of a side branch originating from a stented segment, the use of distal protection devices, and intake of dietary supplements including n-3 PUFAs. UAP was defined as either angina with a progressive crescendo pattern or angina that occurred at rest. Moreover, ischaemic ST changes in a resting state without elevation of myocardial biomarkers were also included as UAP. Recent acute coronary syndrome was defined as acute coronary syndrome within one month. This study was approved by the ethics committee of Chubu Rosai Hospital and all patients provided informed consent.
DATA COLLECTION AND LABORATORY EXAMINATIONS
Various lipid profiles including low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol, eicosapentaenoic acid (EPA), and arachidonic acid (AA) were measured using commercial radioimmunoassay kits and specific immune radiometric assays. The composition of serum fatty acids was determined by capillary gas chromatography. Total lipids were extracted by Folch’s procedure and then fatty acids were methylated with boron trifluoride and methanol; methylated fatty acids were analysed using a Shimadzu GC-17A gas chromatograph (Shimadzu Corporation, Kyoto, Japan) and an Omegawax 250 capillary column (0.25 mm internal diameter, 30 m; Supelco, Inc., Bellefonte, PA, USA). Serum troponin T (TnT) was measured using an enzyme immunoassay kit (Roche Diagnostics, Tokyo, Japan). The detection limit of this system is 0.03 ng/mL and linearity is achieved from 0.1 to 2 ng/mL. A level of TnT <0.03 ng/mL was considered a negative result and any reading from 0.03 up to 0.1 ng/mL was considered 0.1 ng/mL. A TnT level of >2 ng/mL was considered 2 ng/mL. We defined a post-procedural TnT level of >0.3 ng/mL as pMI, which was three times the normal limit (manufacturer’s clinical cut-off value 0.1 ng/mL).
DEFINITION OF RISK FACTORS
Hypertension was defined as a history or presence of hypertension with systolic blood pressure of >140 mmHg and/or diastolic blood pressure of >90 mmHg, or antihypertensive treatment. Diabetes mellitus was defined as a history of diabetes mellitus, a fasting plasma glucose concentration >126 mg/dL, a randomised plasma glucose concentration >200 mg/dL and/or antihyperglycaemic treatment. Smoking status was defined as current or cessation within six months before PCI.
PCI PROCEDURE
All patients received treatment with at least one antiplatelet agent 24 hrs prior to the procedure. Before performing coronary angiography and PCI, patients were given an intracoronary dose of 0.5 mg isosorbide dinitrate to prevent coronary spasm. In quantitative coronary angiography, reference diameter and percent diameter stenosis were measured by a validated automated edge-detection programme (QCA-CMS; Medis, Leiden, The Netherlands).
STATISTICAL ANALYSIS
Continuous and categorical variables are expressed as mean ±standard deviation and proportions, respectively. Univariate analysis was employed to compare various clinical and procedural parameters between patients with and without pMI. The Student’s t-test was used for continuous normally distributed variables, and the Mann-Whitney U test was used for non-normally distributed variables. Chi-square and Fisher’s exact tests were applied for categorical variables, when appropriate. Regarding the rate of pMI, three groupings of LDL/HDL or EPA/AA tertiles were evaluated using the Cochran-Armitage chi-square test for trend. Logistic regression analysis was performed to study the univariate and multivariate predictors for pMI adjusting for confounding factors (age, sex, and BMI), presence of UAP, stented length, and lipid profiles. Comparison of area under the curve (AUC) was performed to study the superiority of lipid profiles for predicting pMI. A p-value <0.05 was considered statistically significant.
Results
A total of 302 patients fulfilled the inclusion criteria. Of these, the following patients were excluded: elevated pre-procedural biomarkers (12 patients), multivessel stenting in a single procedure (10 patients), chronic total occlusion (18 patients), angioplasty with atherectomy (15 patients), occlusion of a side branch originating from a stented segment (three patients), the use of distal protection devices (six patients), and intake of dietary supplements including n-3 PUFAs (five patients). Therefore, 231 patients were enrolled in this study. All of these patients had angina pectoris, documented ischaemia or both.
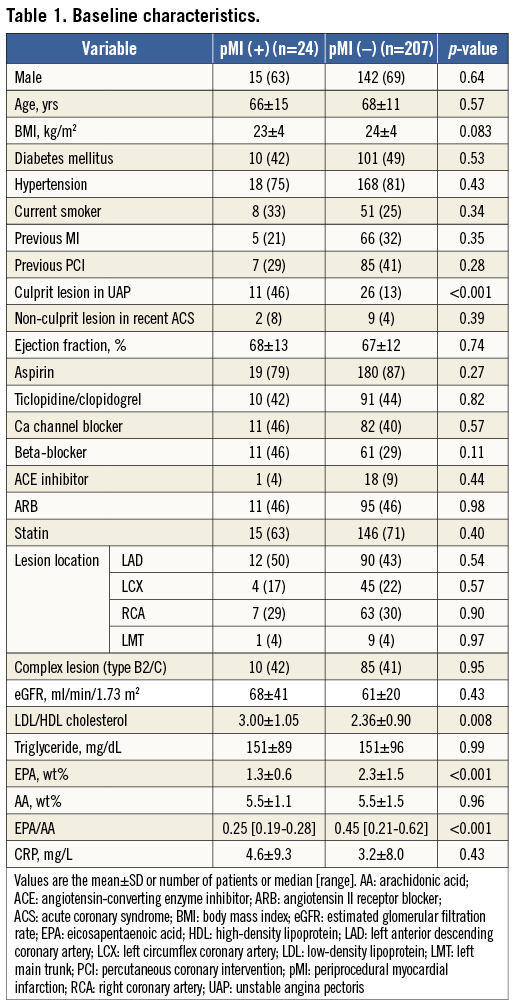
Baseline characteristics
The baseline characteristics of patients are presented in Table 1. There were 24 patients with pMI and 207 patients without pMI. Of the 24 patients with pMI, chest discomfort was observed in seven patients, and ST change on electrocardiography was observed in five patients. No patient showed development of new Q-wave. We could not find any significant differences in clinical status or medical treatment between patients with and without pMI except for the greater proportion of UAP in patients with pMI. LDL/HDL (3.00±1.05 vs. 2.36±0.90, p=0.008) was significantly increased, and EPA/AA was significantly decreased (0.25 [0.19-0.28] vs. 0.45 [0.21-0.62], p<0.001) in patients with pMI compared with those without pMI.
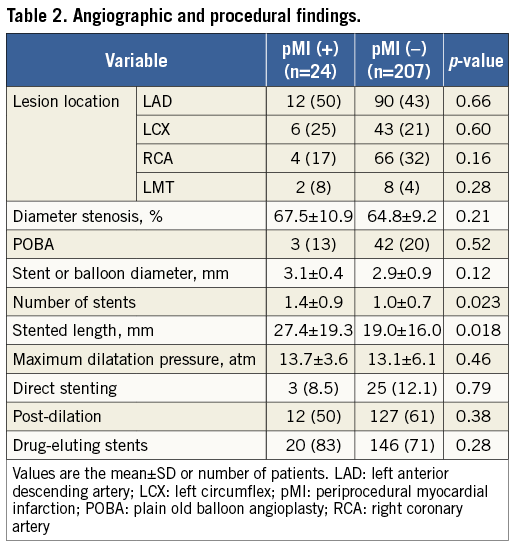
There were no significant differences in angiographic and procedural findings except for a greater number of stents (1.4±0.9 vs. 1.0±0.7, p=0.023) and stented length (27.4±19.3 vs. 19.0±16.0 mm, p=0.018) in patients with pMI compared with those without pMI (Table 2).
RELATIONSHIP OF VARIOUS PARAMETERS WITH THE INCIDENCE OF PERIPROCEDURAL MYOCARDIAL INFARCTION
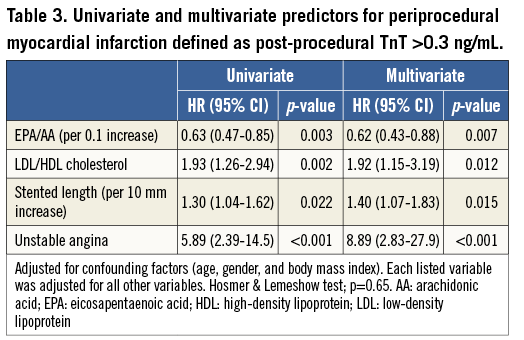
Figure 1 shows the relationship between lipid profiles and the incidence of pMI. The rate of pMI was significantly associated with a decreasing tertile of EPA/AA (p=0.006) (Figure 1A), and an increasing tertile of LDL/HDL (p=0.021) (Figure 1B). On multivariate logistic analysis after adjustment for age, sex, BMI, stented length, and presence of UAP, EPA/AA per 0.1 increase (hazard ratio [HR] 0.62, 95% CI: 0.43-0.88, p=0.007), LDL/HDL (HR 1.92, 95% CI: 1.15-3.19, p=0.012), stented length (HR 1.40, 95% CI: 1.07-1.83, p=0.015), and the presence of UAP (HR 8.89, 95% CI: 2.83-27.9, p<0.001) were significantly and independently associated with the incidence of pMI (Table 3).
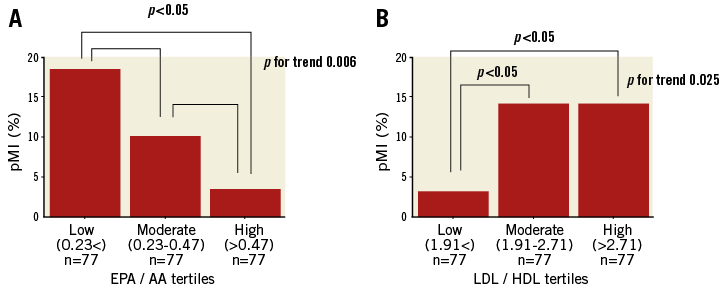
Figure 1. The incidence of pMI according to EPA/AA and LDL/HDL tertiles. The incidence of pMI was significantly associated with a decreasing tertile of EPA/AA (p=0.006) in panel A, and an increasing tertile of LDL/HDL (p=0.021) in panel B. AA: arachidonic acid; EPA: eicosapentaenoic acid; HDL: high-density lipoprotein; LDL: low-density lipoprotein; pMI: periprocedural myocardial infarction
PREDICTIVE VALUE OF LIPID PROFILES FOR pMI
The area under the receiver operating characteristic curve (AUC) was 0.706 (95% CI: 0.717-0.891) for EPA/AA and 0.675 (95% CI: 0.717-0.891) for LDL/HDL, and the optimal cut-off value was 0.33 and 2.34, respectively. Both low EPA/AA (<0.33) and high LDL/HDL (>2.34) provided an incremental predictive value for pMI (AUC=0.804, 95% CI: 0.717 to 0.891; sensitivity=0.75, specificity=0.81) (Figure 2). Figure 3 shows the distribution plot for EPA/AA and LDL/HDL. Eighteen of 24 patients (75%) in whom pMI occurred had low EPA/AA (<0.33) and high LDL/HDL (>2.34).
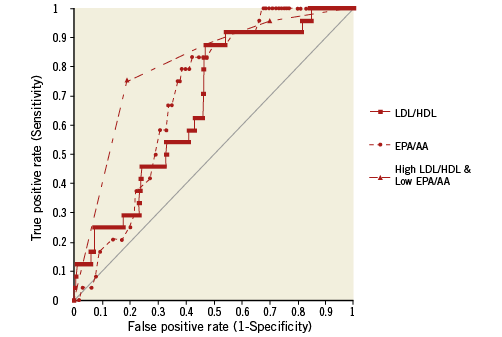
Figure 2. Comparison of ROC analysis according to the lipid profiles. The receiver operating characteristic analysis showed the superiority of both EPA/AA and LDL/HDL cholesterol (AUC=0.804, 95% CI: 0.717-0.891) compared to EPA/AA (AUC=0.702; 95% CI: 0.717-0.891, p=0.024) or LDL/HDL cholesterol (AUC=0.675; 95% CI: 0.717-0.891, p=0.001) alone. AA: arachidonic acid; EPA: eicosapentaenoic acid; HDL: high-density lipoprotein; LDL: low-density lipoprotein; ROC: receiver operating characteristic curve
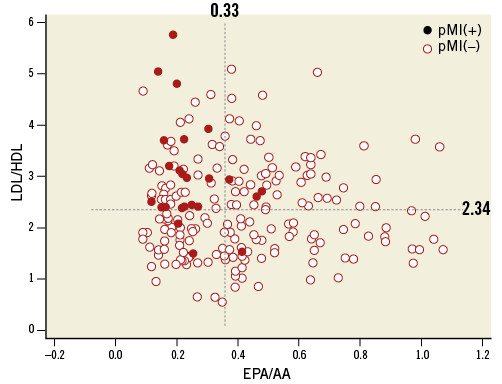
Figure 3. Distribution plot according to EPA/AA and LDL/HDL. Eighteen of 24 patients (75%) in whom a pMI occurred had low EPA/AA (<0.33) and high LDL/HDL (>2.34). AA: arachidonic acid; EPA; eicosapentaenoic acid; HDL: high-density lipoprotein; LDL: low-density lipoprotein; pMI: periprocedural myocardial infarction
Discussion
This study demonstrated that lipid profiles including EPA/AA and LDL/HDL were significantly associated with the incidence of pMI, independent of the known predictors such as the presence of UAP and increased stented length. In addition, as shown in Figure 2 and Figure 3, the combination of decreased EPA/AA and increased LDL/HDL provided the incremental predictive value for pMI.
Previous studies have reported the association of pMI with adverse events. However, these studies evaluating the relationship between the post-procedural cardiac troponin level and long-term prognosis have, in general, not excluded patients with acute coronary syndromes, many of whom would have had abnormal cardiac biomarker levels at baseline19,20. In addition, most periprocedural myocardial infarcts are very small in relation to the magnitude of myonecrosis, especially in patients with SAP. Hence, in the present study, patients with elevated pre-procedural biomarkers at baseline were excluded, and patients with pMI defined as a TnT level >0.3 ng/mL were significantly associated with a worse outcome, although much higher adverse event rates in patients with pMI than in those without pMI might be attributable to the relatively low number of patients with pMI at risk (Online Figure 1, Online Figure 2). These findings suggest that we cannot ignore the impact of pMI on long-term outcome, even in patients with very low levels of myonecrosis. Nevertheless, management of pMI in the setting of elective PCI remains a matter of considerable controversy and uncertainty, especially regarding therapeutic implications21-23. The size of pMI correlates directly with the extent to which the plaque volume is reduced (embolised) by PCI, because more debris is sent downstream. Moreover, the composition of the plaque influences the extent of pMI. PCI for plaques with large lipid cores leads to greater degrees of myonecrosis, whereas fibrous plaques are relatively inert in this regard24. Indeed, we have previously reported the direct correlation of large lipid core with the extent of pMI7. On the other hand, we have recently reported the association of decreased PUFAs and increased LDL/HDL level with lipid-rich plaques18,25. In the present study, the change of plaque composition in patients with decreased EPA/AA and increased LDL/HDL may be one possible mechanism to prevent pMI.
Regarding therapeutic implications, statins, which are widely used to decrease LDL cholesterol level, have been shown to reduce the occurrence of pMI26. In our population, as shown in Table 1, baseline treatment with statins did not have any impact on pMI. This discrepancy compared with previous studies may be due to the relatively small sample size of our study population and/or the various doses and classes of statins prescribed in this study. Although the underlying mechanism of the beneficial effects of statins in preventing pMI remains elusive, pleiotropic effects beyond LDL cholesterol level reduction have been advocated27. In this regard, n-3 PUFAs also have several anti-arteriosclerotic effects including inhibiting platelet aggregation, inflammatory cytokine production, and the expression of adhesion molecules, which play a critical role in the prevention of pMI10. In the present study, serum EPA/AA was significantly associated with the incidence of pMI. Management of PUFAs in addition to statin treatment might further reduce the incidence of pMI, but this needs further confirmation in a prospective trial. A recent large-scale randomised clinical trial and a meta-analysis failed to show the beneficial effect of n-3 PUFA supplements on major cardiovascular events28,29. These landmark studies had several differences in terms of methodological issues from the present study. Serum PUFA levels were not measured in these studies. Furthermore, in these studies hard endpoints such as death or major cardiovascular events were used as the primary endpoints, whereas pMI was used as the primary endpoint in the present study as a major complication of PCI or a surrogate marker of plaque vulnerability.
Limitations
Several limitations should be addressed. First, the study population was relatively small. Second, there are also no data regarding dietary characteristics or lifestyle factors which may have influenced PUFA levels30. Finally, this study is an observational study, not a randomised design. Therefore, the result of this study does not allow us to make definitive conclusions regarding the management of pMI. Our findings need further confirmation of the therapeutic implications.
Conclusion
In conclusion, both low EPA/AA and high LDL/HDL cholesterol were significantly associated with pMI, creating the possibility of a new therapeutic target of pMI.
| Impact on daily practice The occurrence of pMI following elective PCI is associated with adverse clinical outcome. As shown in this study, patients with lower EPA/AA and higher LDL/HDL have a higher incidence of pMI. Thus, EPA/AA and LDL/HDL levels provide useful information for prediction of pMI, creating the possibility of a new therapeutic target of pMI. |
Acknowledgements
We thank Masaaki Soma, PhD, for his excellent assistance with the manuscript.
Conflict of interest statement
The authors have no conflicts of interest to declare.
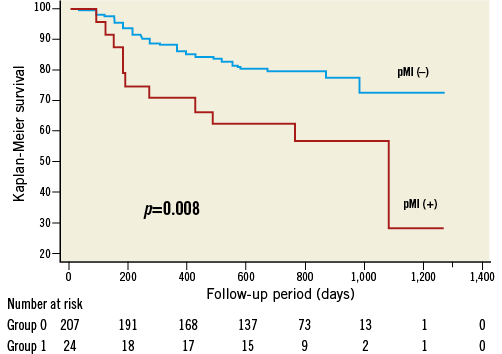
Online Figure 1. Kaplan-Meier survival curves for major adverse cardiac events according to the presence or absence of pMI. Patients with pMI following an elective PCI showed worse long-term clinical outcomes as compared with their counterparts without pMI (log-rank p=0.008). PCI: percutaneous coronary intervention; pMI: periprocedural myocardial infarction
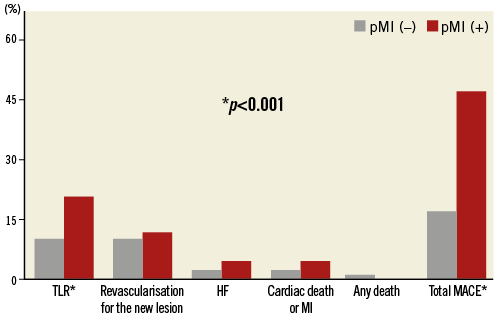
Online Figure 2. Events during follow-up according to the presence or absence of pMI. HF: heart failure; MACE: major adverse cardiac events; MI: myocardial infarction; TLR: target lesion revascularisation