Antiproliferative drugs have revolutionised the management of coronary artery disease. Following implantation of the first drug-eluting stent (DES) in a coronary artery in 19991 and subsequent publication of the Randomized Comparison of a Sirolimus-Eluting Stent with a Standard Stent for Coronary Revascularization (RAVEL) trial, the field of interventional cardiology was changed forever. The RAVEL trial demonstrated that a sirolimus-eluting stent dramatically reduced restenosis, major adverse cardiac events and mortality compared to a bare metal stent (BMS), with durable results up to five years2-4. Subsequent large-scale randomised trials confirmed these results, as well as the cost-effectiveness of both sirolimus- and paclitaxel-eluting stents5-8. Second-generation DES provided incremental improvement in outcomes over first-generation platforms and DES were shown to be superior to BMS in almost every clinical and anatomic scenario1. Continued improvements in stent design, device deliverability, and the evolution of drug/polymer chemistry have further established DES as the standard of care for percutaneous coronary intervention1,9.
Based on these remarkable results, there was also enthusiasm regarding the potential of DES to improve the durability of peripheral vascular interventions. Despite this anticipation of great success, early experience with DES in the peripheral arteries was disappointing. The first randomised study of drug-coated stents in the peripheral vasculature was the SIROlimus Coated COrdis SMART™ Nitinol Self-expandable Stent for the Treatment of Obstructive Superficial Femoral Artery Disease (SIROCCO) trial10-12. In this study and its follow-up, 93 patients with an average SFA lesion length of 8.3 cm were treated with either a self-expanding sirolimus-eluting stent or a self-expanding BMS. Despite promising early results, no difference in clinical outcomes or in-stent restenosis was found at 24 months between DES and BMS. Numerous explanations for the failure of DES were proposed, including inappropriate sirolimus dose and/or elution kinetics, and the potential negative impact of the polymeric stent coating. The Superficial Femoral Artery Treatment with Drug-Eluting Stents (STRIDES) non-randomised trial evaluated the Dynalink everolimus-eluting stent (Abbott Vascular, Santa Clara, CA, USA)13. This single-arm study of 104 patients with a mean SFA lesion length of 9 cm demonstrated a primary patency rate of only 68.5% at 12 months13. The STRIDES results were not dissimilar to those previously demonstrated with the bare metal Dynalink stent. Disappointing results from these two trials led to the abandonment of both peripheral DES programmes.
The paclitaxel-eluting Zilver® PTX® (Cook Medical, Bloomington, IN, USA) stent is the only peripheral DES that has been shown to improve patency compared to BMS. A unique feature of the Zilver PTX stent is direct application of paclitaxel to the stent without the use of a polymeric coating. Paclitaxel’s unique properties make it well suited as an antirestenosis agent for peripheral vascular interventions. Paclitaxel is lipophilic and avidly binds intracellular target proteins, which allows drug uptake in the target artery with detectable retention for up to two months, despite being cleared from the circulation within 10 hours14-16. This ability to bind rapidly to the arterial wall made it possible for the Zilver PTX stent to deliver paclitaxel from the abluminal surface of the stent without the aid of polymers, bindings, or carriers.
The Zilver PTX was evaluated in a randomised controlled trial of 474 patients with lesions in the SFA and proximal popliteal artery (mean lesion length of 6.5 cm)14. Patients were randomised to angioplasty alone (PTA) or DES. For patients who required a stent after inadequate PTA (due to dissection or poor response), there was a secondary randomisation between BMS and DES. At one year, primary patency was higher after stenting with the Zilver PTX compared to PTA (83% versus 32.8%, p<0.001). Bail-out stenting was required in 50% of the PTA group – in this subset, the primary patency at one year for provisional DES was superior to bail-out BMS (89.9% versus 73%, p=0.01), representing a 60% reduction in restenosis rate with DES14. Two-year and five-year follow-up demonstrated sustained benefit of DES over BMS (two-year: 83.4% versus 61.1%; five-year: 72.4% versus 53.0%)17,18.
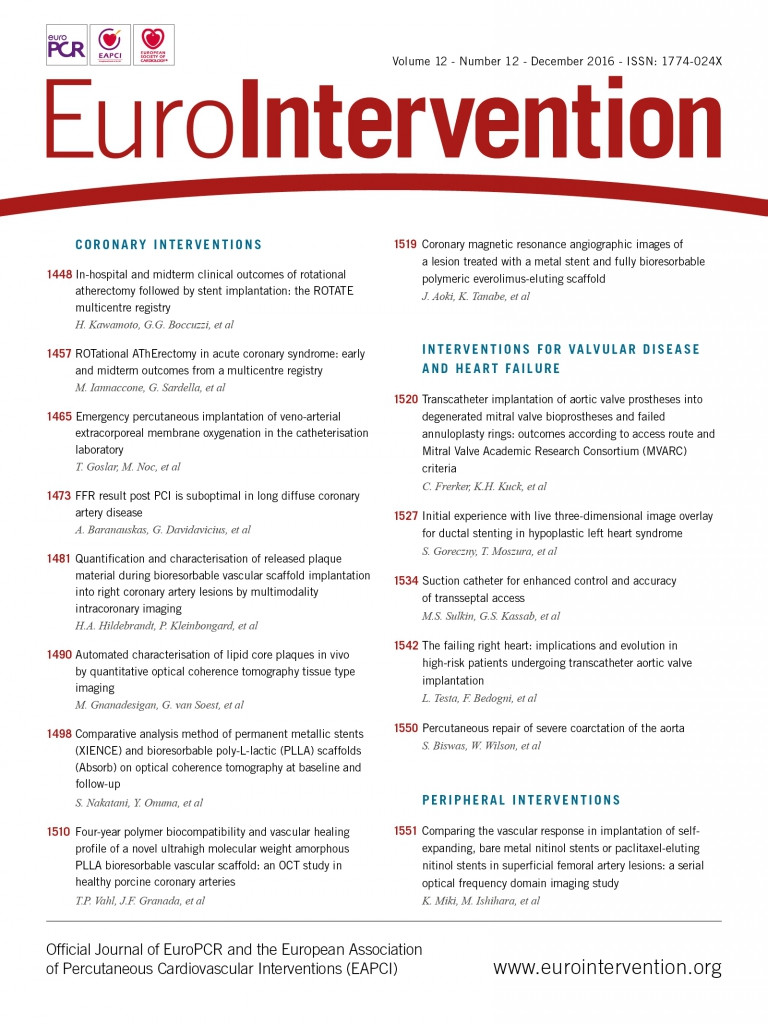
In the current issue of EuroIntervention, Miki and colleagues19 contribute further to our understanding regarding paclitaxel-eluting DES in the SFA by allowing us to see precise differences in neointimal growth within the Zilver PTX compared to BMS with optical imaging. This is the first study of its kind to use an advanced imaging modality to characterise better the vascular response to self-expanding DES in a peripheral artery. The investigators used optical frequency domain imaging (OFDI), a light-based imaging modality generated from optical coherence technology. This second-generation OCT technique provides higher imaging resolution and greater depth penetration than conventional time-domain OCT. OFDI also allows imaging with faster pullback speed, making it suitable for imaging longer lesions in peripheral arteries, such as in the SFA. Twenty-eight SFA lesions in 26 patients were ultimately evaluated, 13 of which were treated with BMS and 15 with paclitaxel-eluting stents. Patients were evaluated with angiography and OFDI after implantation and at six months. Quantitative vascular angiography demonstrated that the percent stenosis at six-month follow-up was significantly lower in the DES group than in the BMS group (28.5% stenosis vs. 39.7%, p=0.04). Volumetric OFDI analysis revealed that neointimal volume index was smaller (7.4±2.6 mm3/mm vs. 10.5±3.2 mm3/mm, p<0.01) and late lumen area loss was lower (2.9±1.3 mm3/mm vs. 5.6±2.8 mm3/mm, p<0.01) in the DES group. Post-stent implantation abnormalities noted on OFDI imaging (protruding materials, edge dissections, malapposed struts) had almost completely resolved at six months with no differences between the two groups.
The authors should be commended on this unique and detailed assessment of the vascular response to implantation of bare and drug-eluting self-expanding stents in the SFA. They confirm that, in the short term, DES have improved patency and less neointimal proliferation than BMS. This study was a sub-analysis of a larger prospective randomised study, but was well powered to answer the question that they asked. A limitation of this paper is the short follow-up period of only six months. Another important limitation is the use of a BMS stent platform other than the Zilver stent. It is possible that differences in the vascular response to healing could be due to stent design rather than drug effect.
Although many questions remain about the appropriate strategy for endovascular treatment of SFA lesions, we now have additional evidence that local delivery of paclitaxel from a drug-eluting stent can modify the biologic response to injury and reduce neointimal proliferation. For those who doubted that direct application of paclitaxel to a self-expanding stent could lead to a meaningful therapeutic effect, “seeing is believing”. Evolving evidence also suggests that local delivery of paclitaxel from a drug-coated balloon can result in sustained improvement in patency compared to PTA alone20,21. Much like in the coronary arteries, the combination of antiproliferative drugs and devices will become a mainstay of treatment for SFA disease in the years to come.
Conflict of interest statement
J. Laird is a consultant or advisory board member for Bard Peripheral Vascular, Boston Scientific, Medtronic, and Abbott Vascular. He receives research support from W.L. Gore. M. Loja has no conflicts of interest to declare.