We read with great interest the recent report by Capodanno et al1. In the European multicentre GHOST-EU registry, the authors reported that the rate of definite/probable scaffold thrombosis was 2.1% (definite scaffold thrombosis: 1.8%, probable scaffold thrombosis: 0.3%) in an all-comers population at six months. More specifically, the rate of definite/probable scaffold thrombosis was 1.4% (9/626) in stable/silent angina pectoris (SAP), 2.5% (14/563) in acute coronary syndrome (ACS) and 2.1% (4/192) in ST-segment elevation myocardial infarction (STEMI). This publication prompted us to review the rates of scaffold thrombosis in all-comers, SAP, ACS and STEMI either reported so far in peer review journals or presented at international meetings.
Table 1 summarises the rate of scaffold thrombosis in each individual report. Excluding the GHOST-EU registry, the rate of definite/probable scaffold thrombosis was 0.89% in all-comers, 0.68% in SAP, 1.71% in ACS and 0.67% in STEMI. There were 25 definite and two probable scaffold thromboses. Out of 27 patients with scaffold thrombosis, two had acute (≤24 hours after procedure) thrombosis (0.06%) and 15 had subacute after one day (≤1 month after procedure) thrombosis (0.48%). Premature discontinuation of dual antiplatelet therapy (DAPT) or resistance to clopidogrel at the time of scaffold thrombosis was documented in 29.4% patients (5/17). The rate of scaffold thrombosis when the GHOST-EU registry is added to the series is tabulated at the bottom of Table 1. Potential aetiological causes of scaffold thrombosis could be: 1) suboptimal implantation resulting in underexpansion/acute incomplete strut apposition2-4 or acute disruption of struts5; 2) platelet activation due to low shear stress created by the relatively thick strut6; 3) delayed tissue coverage in an overlapped segment7-9; 4) discontinuation of DAPT or resistance to DAPT9.
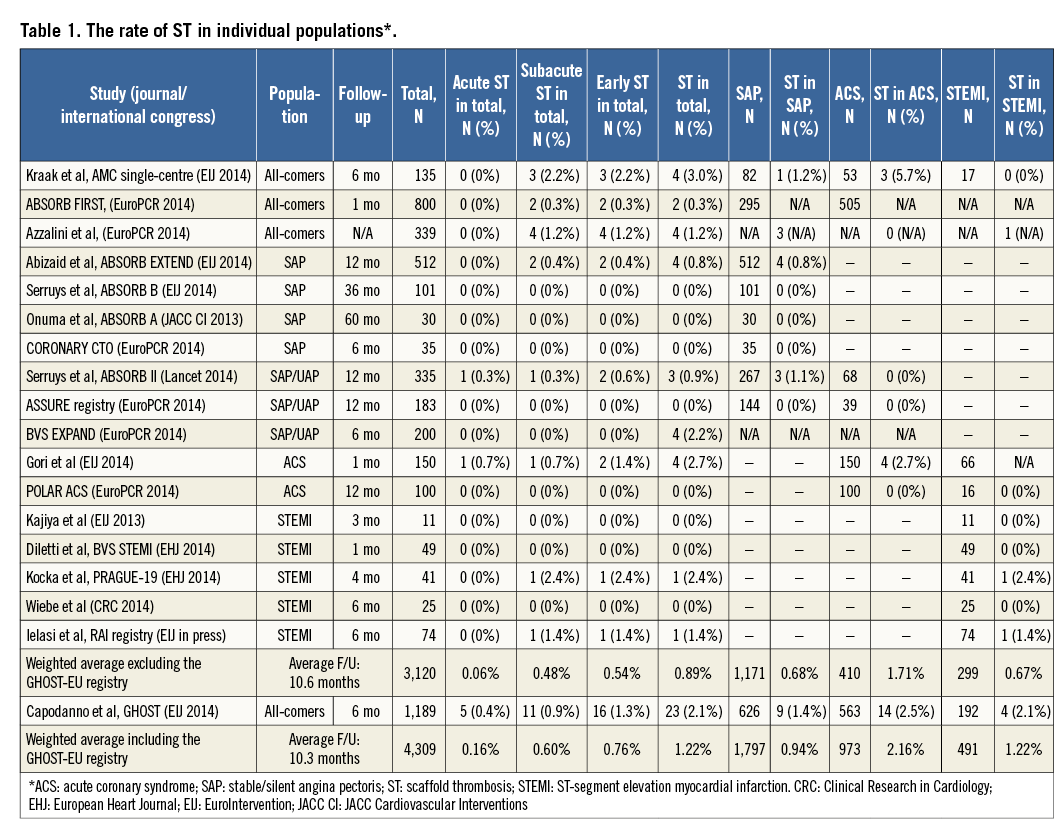
In the first randomised comparison of ABSORB II10, the rate of definite scaffold/stent thrombosis was 0.6% in Absorb (one acute and one subacute case) and 0% in XIENCE (p=1.0), and the rate of definite/probable scaffold/stent thrombosis was 0.9% in Absorb and 0% in XIENCE (p=0.55)10.
Further randomised studies may or may not confirm these scaffold thrombosis rates in the future11,12.
Conflict of interest statement
The authors have no conflicts of interest to declare.

