With the development and implementation into clinical practice of newer drug-eluting stents (DES), stent thrombosis (ST) rates have consistently been decreasing. This is because current platforms are manufactured with thin struts in combination with drug delivery systems promoting rapid endothelialisation, and they are therefore more forgiving in terms of procedural optimisation. However, with the advent of bioresorbable scaffolds (BRS), a paradigm shift has taken place. Due to their lower radial strength, BRS require thorough lesion preparation as well as systematic post-dilatation to achieve an adequate result. Their thicker and wider struts result in greater protrusion into the vessel lumen, causing loss of laminar flow, with areas of oscillatory shear stress that promote platelet activation1. In addition, if these devices are not completely endothelialised and incorporated into the vessel wall, a non-uniform reabsorption process may cause protrusion of some struts into the lumen of the vessel. In this context, adequate platelet inhibition becomes critical to decrease the risk of ST.
Current European guidelines recommend that, following metallic DES implantation, dual antiplatelet therapy (DAPT) should be prescribed for six months in stable coronary artery disease (Class I, level B) and for 12 months in acute coronary syndrome patients (Class I, level A), although shorter durations may be considered in patients at high bleeding risk (Class IIb, level A)2,3. Such guidelines, however, do not provide specific recommendations on optimal DAPT duration following BRS implantation. Consequently, clinical practice in this important setting is heterogeneous and influenced by several factors. For example, the European experts’ consensus document on BRS4 indicates that a six- to 12-month strategy can be prescribed for simple lesions treated with one BRS, while longer durations (18-24 months) are suggested in complex lesions (e.g., scaffold overlap, bifurcations, etc.).
There is convincing evidence that BRS are associated with a higher risk of ST compared to second-generation DES5,6. The underlying reasons are multifaceted, and have been linked to incomplete lesion coverage, underexpansion, malapposition, rheological disturbances in the proximity of their thick struts, delayed endothelialisation, late structural discontinuity, or device dismantling1,5,7. An important question to be addressed is whether these shortcomings related to the structure of current BRS can be overcome utilising an appropriate implantation technique able to provide an optimal final result. Besides mechanical/procedural factors, DAPT discontinuation is another important cause of ST5,8. DAPT is the only modifiable factor upon which the clinician can act once BRS implantation has taken place. However, the time-dependent interaction of DAPT with the development of ST has been poorly characterised so far.
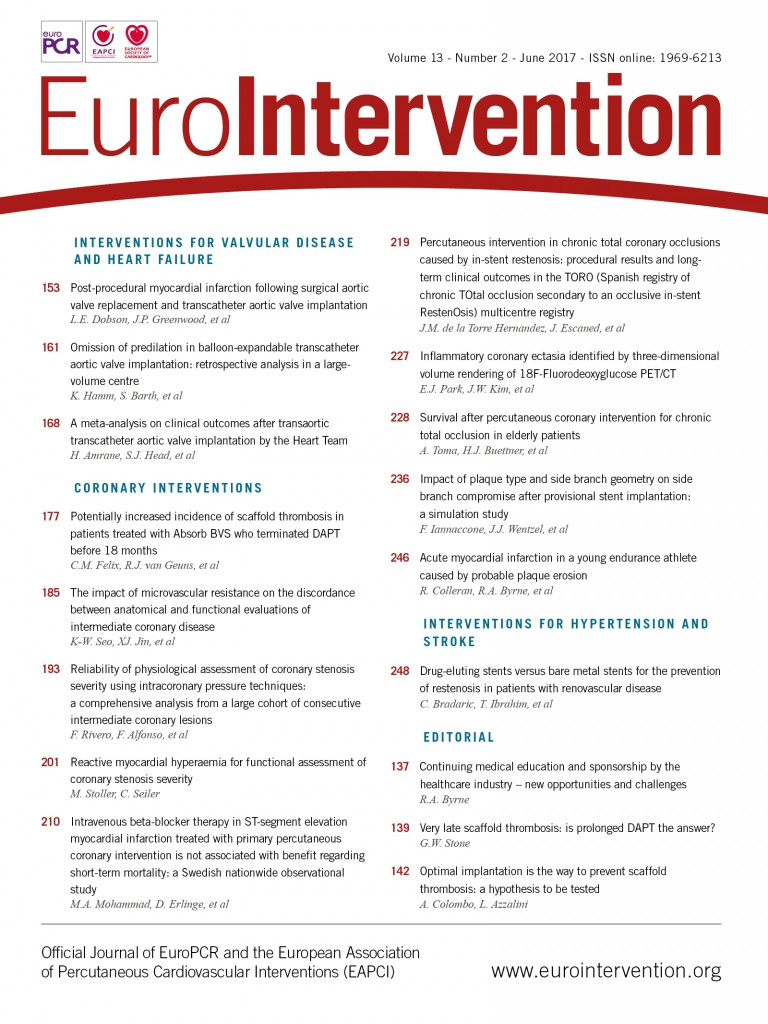
In this issue of EuroIntervention, Felix et al9 utilised data from three regional registries of BRS-treated patients (n=808) to investigate the relationship between DAPT discontinuation and ST.
The study population consisted of 685 patients for whom DAPT status was known and who were treated with DAPT for >6 months after BRS implantation. Subjects taking oral anticoagulants and cases of early ST (n=14/808, 1.7%) were excluded. The authors compared the incidence of definite/probable ST for the period on DAPT versus after DAPT termination. Patient population characteristics are remarkable for a high prevalence of acute coronary syndrome (70%, including 29% of patients with ST-elevation myocardial infarction). Accordingly, >60% of patients were prescribed either prasugrel or ticagrelor in addition to aspirin. Forty-six percent of patients had a type B2/C lesion. A mean of 1.4 scaffolds/patient was implanted; mean total scaffold length was 33.1±21.6 mm. Median follow-up was 730 days. Between six and 18 months, the incidence of ST was 1.8%, or 0.83 ST/100 patient-years. After DAPT termination, ST incidence tended to be higher (1.77/100 patient-years), compared to the incidence on DAPT (0.26/100 patient-years, p=0.12). Additionally, ST incidence increased within the first month after DAPT termination (6.57 ST/100 patient-years, p=0.01), compared with while patients were on DAPT. In this study, no case of very late ST was observed in patients who continued on DAPT for >18 months.
The overall 18-month ST rate was 3.3%, which is quite high, although not surprising, since their data indicate that BRS implantation did not strictly follow optimal implantation guidelines (complete lesion preparation, adequate sizing, systematic high-pressure post-dilatation with a non-compliant balloon, and final invasive imaging assessment)4. In fact, predilatation and post-dilatation were performed in 88% and 57%, respectively. In addition, predilatation and post-dilatation are not dichotomous actions: these techniques need to be tailored (i.e., pressure, inflation time, balloon-to-scaffold ratio, etc.) in order to obtain a specific result. Invasive imaging is the way to confirm achievement of an optimal result, and it was used in only 31% of patients at baseline. While all of these actions are not a must for current metallic stents, they are necessary to overcome the limitations of current BRS. Data from our group10 suggest that, when BRS implantation is performed according to the aforementioned practice, long-term clinical outcomes are acceptable and the rate of ST is low (1.2%) at two-year follow-up, despite higher lesion complexity (75% type B2/C lesions) and longer total scaffold length (53.2±32.5 mm). In our case series, more than 90% of patients were still taking DAPT at two-year follow-up; therefore, we cannot discern the respective contribution of optimal implantation technique versus extended DAPT continuation to our results.
With regard to the timing of ST, Mehran et al11 also demonstrated a time-dependent relationship between DAPT discontinuation and metallic ST, similar to the present study. In the report by Mehran et al, ST risk was highest between zero and seven days after DAPT disruption, and lowest if DAPT was discontinued >30 days after stent implantation, irrespective of stent type (DES vs. BMS).
Taken together, the available evidence suggests that patients undergoing BRS implantation are markedly dependent on platelet inhibition at midterm follow-up if ST risk is to be minimised. Therefore, this patient population might benefit from extended DAPT, possibly until the bioresorption process is completed (24-36 months).
Whether the utilisation of an optimised BRS implantation strategy, verified with intravascular imaging, allows better endothelialisation of the scaffolds avoiding the need for prolonged DAPT is a reasonable hypothesis that needs to be proven.
Conflict of interest statement
The authors have no conflicts of interest to declare.