Bioresorbable scaffolds (BRS) were developed as an alternative to metallic drug-eluting stents (DES) for use during percutaneous coronary intervention to overcome the lifelong risk of complications that arises from the permanent metallic implant long after the hazards of vessel recoil and constrictive remodelling have passed1. BRS also address other inadequacies of metallic DES, including the permanent jailing of side branches, the consequences of full metal jacket treatment of diffuse disease eliminating late surgical options, the detrimental space-occupying effects of an additional metal layer when treating in-stent restenosis, and blooming artefacts precluding use of CT imaging for non-invasive follow-up. However, for the long-term benefits of BRS to be realised (a yet unproven hypothesis being tested in the ABSORB IV trial with up to 10-year follow-up), BRS should ideally be as safe and effective as contemporary metallic DES within the first few years, until the time of their complete bioresorption. In this regard, randomised trials with the first and most widely used BRS, the poly-L-lactic acid (PLLA)-based everolimus-eluting Absorb BVS (Abbott Vascular, Santa Clara, CA, USA), have demonstrated increased rates of device-related adverse events within the first several years after implantation, compared to the cobalt-chromium everolimus-eluting XIENCE stent (also Abbott Vascular)2-4. Most of these events have consisted of scaffold thrombosis (ScT) and target vessel myocardial infarctions (MI) during the follow-up period. This risk has been attributed mainly to two factors: 1) Absorb is a first-generation BRS, with substantially thicker and wider struts than contemporary metallic DES; and 2) the lesion selection and scaffold implant technique employed in these early trials was suboptimal, with a high rate of Absorb use in vessels smaller than intended for the device (leading to excessive polymer load and vessel surface area coverage), and without routine high-pressure post-dilatation to ensure maximal scaffold expansion and apposition. Indeed, in several non-randomised studies optimal technique has been associated with low rates of adverse events after Absorb implantation5-7.
Surprisingly, despite extensive investigation in patients receiving metallic DES, little is known about the optimal duration of dual antiplatelet therapy (DAPT) after BRS. In the ABSORB randomised trials, DAPT was required for six to 12 months, and was optional thereafter, although 58% of patients remained on DAPT at two years (Stone GW, unpublished data). A detailed study of the potential impact of prolonged DAPT from these studies has not been reported.
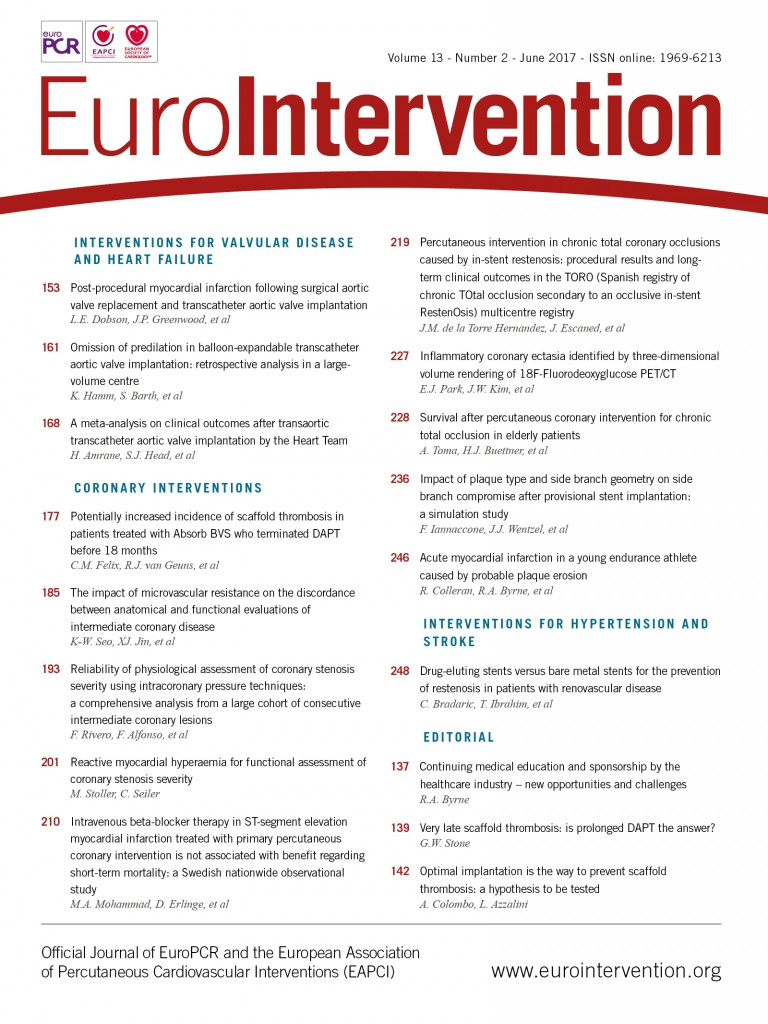
In the present issue of EuroIntervention, Felix and colleagues report an analysis of the impact of DAPT duration after BRS from a pooled study of registries from three Dutch centres8.
A total of 658 treated patients had at least six months of DAPT treatment without ScT in this period, and no use of oral anticoagulants. Patient outcomes were examined from this point until 18 months, with median DAPT duration of 367 days. Most patients had one non-complex lesion treated, with mean scaffold diameter and length 3.1±0.4 and 20.9±5.8 mm, respectively. Of note, intravascular imaging was used in 31.3% of cases, and post-dilatation was performed in only 56.7% (pressure unreported). Five cases of ScT occurred between six and 18 months (0.83/100 patient-years [95% CI: 0.34-1.98]). The incidence of ScT was 0.26/100 patient-years on-DAPT vs. 1.77/100 patient-years off-DAPT, a non-significant difference (p=0.12). However, four of the five ScT cases occurred after one year; none of these four patients was taking DAPT at the time of the event, and in three patients DAPT was discontinued between 10 and 35 days prior, suggesting a temporal relationship. ScT was significantly increased in the first month after DAPT discontinuation compared to the month before (p=0.01).
Should routine DAPT duration after BRS be prolonged to 18 months (or longer) based on these data? Certainly, the present study has limitations that leave several critical questions unanswered. First, this report is a post hoc analysis of registries not designed to address the DAPT duration issue. Some inaccuracies in the timing of DAPT discontinuation are no doubt present. Second, the number of patients and number of ScT events are modest, leading to wide CIs around the point estimates for the event rates on-DAPT and off-DAPT. Indeed, off-DAPT was not significantly associated with increased ScT risk, other than in the first month after DAPT discontinuation. Third, the reasons for DAPT discontinuation were not recorded and are unknown. DAPT “disruption” due to bleeding or non-compliance after metallic DES has been associated with metallic stent thrombosis, but not if DAPT discontinuation was physician-directed in otherwise stable patients9. Thus, although the fact that the ScT risk was particularly increased within one month after DAPT discontinuation suggests that maintenance on DAPT was suppressing these thrombotic events (a phenomenon also seen with metallic DES)10, the same reasons that prompted DAPT stoppage (e.g., bleeding or trauma) may also have increased platelet reactivity leading to ScT. Fourth, the baseline patient and lesion characteristics in those with vs. those without ScT, and on-DAPT vs. off-DAPT were not reported, and no attempt at multivariable adjustment was made to correct for the inevitable imbalances that are almost certain to be present between these groups. Thus, while it is reassuring that the rate of ScT in patients on DAPT between six and 18 months was low (~0.3% per year), was this because of continuous DAPT usage or because patients who tolerate prolonged DAPT represent a low-risk stable cohort? In this regard, 60.3% of patients in the DAPT cohort presented with STEMI or NSTEMI, subgroups in whom at least 12 months of DAPT is indicated regardless of treatment11, and in whom even more prolonged DAPT may be useful12. Did the very late ScT cases off-DAPT cluster in these patients? An apt question would be whether prolonged DAPT after BRS is necessary in stable patients, in whom DAPT for only six months has become the standard of care with metallic DES11. Unfortunately, results are not provided according to presentation with acute coronary syndromes vs. stable ischaemic heart disease. Similarly, anatomic lesion complexity can affect the benefit-risk ratio of prolonged DAPT after metallic DES13, and likely after BRS. Unfortunately, subgroup analysis based on lesion-related factors was not provided. We are also not informed whether an interaction was observed between technique-related factors and DAPT duration. It may be that prolonged DAPT is only beneficial in patients in whom vessel or device sizing is not optimal or in whom high-pressure post-dilatation is not performed, increasing the risk of acute malapposition with subsequent intraluminal scaffold dismantling (ILSD) during the bulk erosion process14. This worthy hypothesis requires validation in future studies. As a fifth limitation, the rates of bleeding in the two groups are not reported, the “dark side” of prolonged DAPT that may offset its beneficial effects15. Finally, the 18-month follow-up duration may not be long enough to characterise the risk period of Absorb bioresorption, which continues for ~3 years, at which time all polymer has been replaced by a provisional matrix.
Thus, while the authors are to be congratulated for the first publication to address whether prolonged DAPT reduces ischaemic complications after coronary BRS implantation, what are the practical implications? Prolonged DAPT clearly reduces thrombosis arising from coronary segments treated with metallic stents, as well as MI from untreated remote sites, and there is no reason to believe that these effects would be any less after BRS. Indeed, given novel failure modes of BRS (ILSD, and in rare cases late recoil), a strong case can be made for three years of DAPT (the time of complete Absorb bioresorption) in patients without excessive bleeding risk16. However, the evidence base for this recommendation is not as strong as I would like, and confirmation is required from larger, prospective studies in which the causes of DAPT discontinuation are tracked and outcomes are adjusted by confounding variables, including implantation technique. Finally, second-generation BRS are being introduced with markedly thinner struts and improved expansion and ease-of-use characteristics that promise to improve the intermediate-term benefit-risk profile of BRS, and which may alter the DAPT duration equation1. Given the rapid pace with which BRS technology is evolving, and the non-trivial risks of prolonged DAPT, vigilance and a willingness to adapt as new data emerge are required to ensure the best outcomes for our patients.
Conflict of interest statement
G. Stone is Chairman of the global Absorb clinical program (uncompensated) and a consultant to Reva.