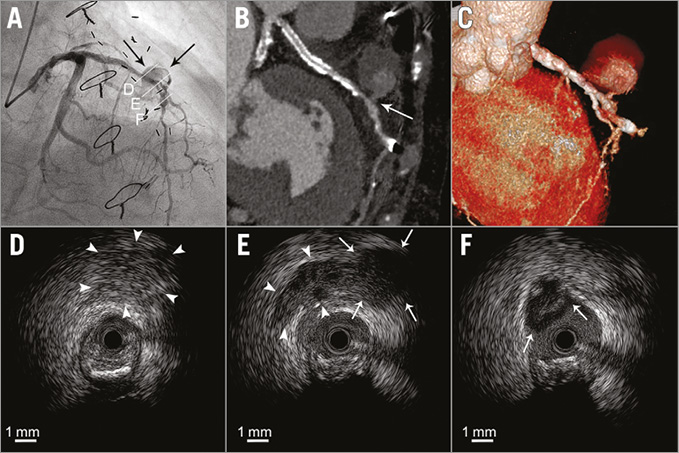
An 85-year-old female with a history of coronary artery bypass graft (CABG) surgery underwent PCI of the mid LAD due to an occluded graft. The 1.75 mm burr was suddenly entrapped in the severely calcified and tortuous lesion after rotational atherectomy with a 1.5 mm burr. Ellis type III coronary perforation occurred after retrieval of the burr with manual pullback. Prolonged balloon inflation resulted in successful haemostasis. However, recurrent coronary perforation occurred the following day, and angiography revealed a pseudoaneurysm (arrows) connected to the LAD via a narrow neck with massive contrast extravasation (Panel A, Moving image 1). MDCT (Panel B, Panel C) clearly described the 19.2×21.0 mm pseudoaneurysm connected to the LAD by a narrow neck (arrow) with contrast enhancement (light grey) and some thrombus (dark grey) (Panel B). IVUS imaging (Moving image 2) could visualise an extravascular heterogeneous high-echoic lesion suggestive of partial thrombus formation (Panel D, arrowheads), an extravascular low-echoic lesion suggestive of active blood inflow (Panel E, arrowheads), encapsulated pericardial fluid (Panel E, arrows), and the interrupted external membrane at the perforated site (Panel F, arrows). Finally, we implanted a 2.8×19 mm polytetrafluoroethylene (PTFE)-covered stent, which completely sealed the pseudoaneurysm (Moving image 3, Moving image 4).
Although the stuck rotablator led to delayed coronary perforation, the accumulation of free pericardial fluid was precluded because of the development of pericardial adhesions following previous CABG, and a pseudoaneurysm was consequently formed.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Initial coronary angiography revealed recurrent coronary perforation and the pseudoaneurysm connected to the left anterior descending artery via a narrow neck with massive contrast extravasation.
Moving image 2. Initial intravascular ultrasound clearly visualised the interrupted external membrane at the perforated site, active blood inflow into the pseudoaneurysm, encapsulated pericardial fluid, and an extravascular heterogeneous high-echoic lesion suggestive of partial thrombus formation.
Moving image 3. Coronary angiography after PTFE-covered stent placement confirmed the sealing of the pseudoaneurysm with no contrast extravasation.
Moving image 4. Intravascular ultrasound after PTFE-covered stent placement demonstrated the complete apposition of the covered stent and exclusion of the pseudoaneurysm with no blood inflow.
Supplementary data
To read the full content of this article, please download the PDF.
Initial coronary angiography revealed recurrent coronary perforation and the pseudoaneurysm connected to the left anterior descending artery via a narrow neck with massive contrast extravasation.
Initial intravascular ultrasound clearly visualised the interrupted external membrane at the perforated site, active blood inflow into the pseudoaneurysm, encapsulated pericardial fluid, and an extravascular heterogeneous high-echoic lesion suggestive of partial thrombus formation.
Coronary angiography after PTFE-covered stent placement confirmed the sealing of the pseudoaneurysm with no contrast extravasation.
Intravascular ultrasound after PTFE-covered stent placement demonstrated the complete apposition of the covered stent and exclusion of the pseudoaneurysm with no blood inflow.