Abstract
Aims: Coronary perforation during percutaneous coronary intervention (PCI) is associated with a high risk of mortality and morbidity. However there has been little data on perforation in the current era despite significant changes in PCI practice. We set out to identify incidence, risk factors and management strategies of coronary perforation in the current era.
Methods and results: We performed a retrospective analysis of the Manchester Heart Centre PCI database from June 2004 to May 2008. Detailed analysis of all cases of suspected perforation was undertaken by case note and angiographic review. Demographic data was collected regarding all patients undergoing intervention. A total of 12,729 coronary lesions were treated in 7,903 patients over four years, during which drug-eluting stent (DES) uptake was 77%. The incidence of perforation was 0.56% (44/12,729). Perforation was associated with an inpatient mortality of 15.9% (7/44). Factors associated with perforation were female sex (p=0.003), increasing age (p<0.01), coronary calcification (p=0.003), use of a cutting balloon (p<0.001) or atheroablation (p<0.001), and treatment of a chronic total occlusion (p<0.01). Factors associated with death after perforation were non-elective procedure (p=0.036) and pericardial drain insertion (p<0.001).
Conclusions: Despite treatment of more complex disease, the incidence of coronary perforation has not increased. Major perforations (Ellis class III) are associated with a high rate of emergency coronary artery bypass graft (CABG) and death. Endovascular treatments allow sealing of the perforation in most cases and deaths occur primarily as a result of cardiogenic shock due to occlusion of the culprit artery. Patient risk factors associated with perforation should be considered when planning or performing PCI.
Introduction
Coronary artery perforation is a potentially life-threatening complication of percutaneous coronary intervention (PCI). Historical data reports an incidence of 0.1-0.48%, with a mortality ranging from 7-17%1-6. The treatment of coronary disease has evolved, and percutaneous intervention is now the treatment of choice for increasingly challenging and complex disease. Target vessel calcification and the use of rotational atherectomy have been associated in some reports with perforation6,7. Additionally, the risk of malapposition of drug-eluting stents (DES) leading to stent thrombosis has given rise to the routine application of very high deployment and post-dilatation pressures, which may also increase the risk of perforation. The management of perforation has also changed with the introduction of new interventional techniques and devices.
Given this change in practice, we present the experience of a high volume tertiary centre in the United Kingdom over a four year period in which there was a high rate of DES usage. We also provide a brief review of the literature and discuss the contemporary management of this condition.
Methods
A retrospective analysis of all procedures recorded in the Manchester Heart Centre PCI database between June 2004 and May 2008 was undertaken. The database contains detailed clinical and demographic data and conforms to the standards required by the British Cardiovascular Intervention Society (BCIS)/Central Cardiac Audit Database (CCAD). A search for patients with coronary perforation was done, which is listed as a specific complication in the BCIS-CCAD database (version 5.5.6). To ensure capture of all incidences of perforation, records of all cases of tamponade, coronary dissection and PCI-related deaths were also reviewed. Detailed case note and angiographic review of the patients found to have perforation was then performed by a single experienced observer (CH). For the control group, we analysed demographic and procedural data for all patients undergoing PCI over the study period.
Demographic data including age, gender, diabetic status and renal dysfunction (serum creatinine concentration of ≥200 μmol/L) was recorded for all patients. Other details collected for all patients included procedural urgency, treatment of a chronic total occlusion, target vessel calcification, drug-eluting stent, rotational atherectomy and cutting balloon use, and whether thrombolysis had been administered within 24 hours of the procedure. Additional data collected for the perforation group included the vessel treated, lesion complexity (as automatically calculated by the database) and vessel tortuosity.
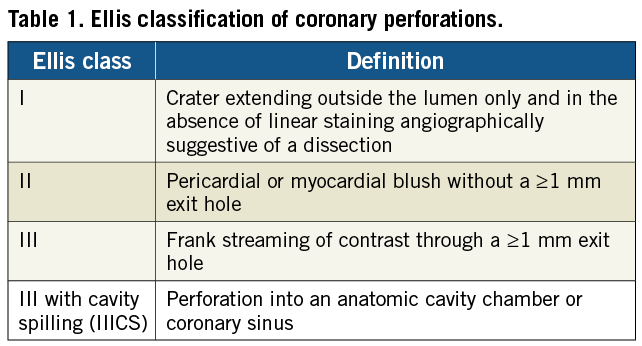
The Ellis classification system8 was used to grade the severity of perforation (Table 1). As class I perforations have been repeatedly demonstrated to be of a benign nature, and do not adversely affect clinical outcomes2,4,9,10, they were not included in our analysis. The timing of perforation was defined as immediate (identified during the procedure) or late (identified post-procedure as a result of hypotension and/or a pericardial effusion) and the device causing perforation and subsequent management were recorded.
Outcomes were recorded in terms of need for urgent CABG, delayed discharge from hospital or death during the index admission.
Statistics were calculated using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). To establish the relationship between categorical variables, the chi-square test was used and where the criteria for chi-square were not met, the Fisher’s exact test was substituted. To compare continuous variables the Student’s t-test was used.
Results
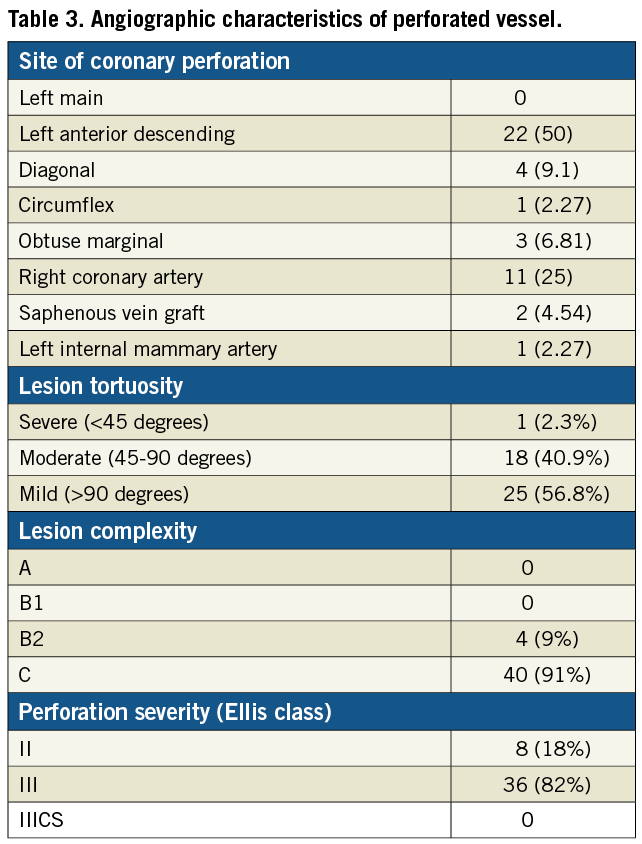
A total of 12,729 lesions were treated in 7,903 patients between 1 June 2004 and 31 May 2008. The overall incidence of coronary artery perforation of Ellis classification II- III during this period was 0.56%, which represented a total of 44 cases. There were no Ellis class IIICS perforations. The medical records, angiogram films, and procedural and clinical data were available for all 44 patients.
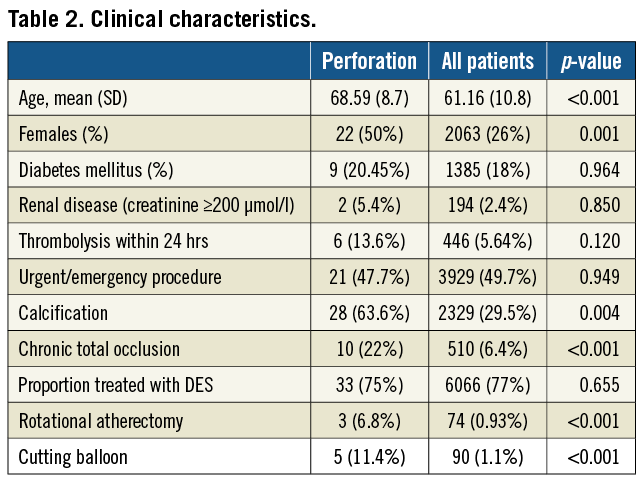
The baseline clinical characteristics are detailed in Table 2.
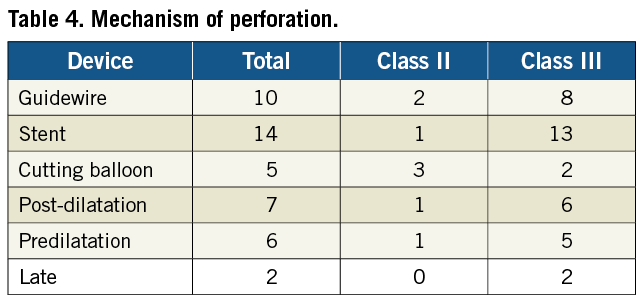
The cases encountered in our tertiary referral centre are predominantly complex and technically challenging. Less than 1% of all cases treated in our centre over the study period were of class A complexity according to the American College of Cardiology/American Heart Association (ACC/AHA) guidelines, whereas 86% were class B2 or class C lesions. All perforations involved lesions classified as class B2 or C. Table 3 shows the angiographic characteristics of the perforated vessels and Table 4 shows the mechanisms of perforation.
FACTORS ASSOCIATED WITH PERFORATION
The patient factors that were associated with an increased risk of perforation were female sex (p=0.003), increasing age (p<0.001), treatment of a chronic total occlusion (p<0.0001) and the presence of coronary calcification (p=0.003). The use of either cutting balloons or rotational atherectomy was also found to be strongly associated with the occurrence of perforation (p<0.0001 for both). However rotational atherectomy itself was not directly responsible for perforation in any patient in this series. In the three cases in which rotational atherectomy were used, perforation occurred during stent deployment in two cases and during cutting balloon inflation in the other. There was no relationship between the use of DES and perforation (p=0.655).
MANAGEMENT OF PERFORATION
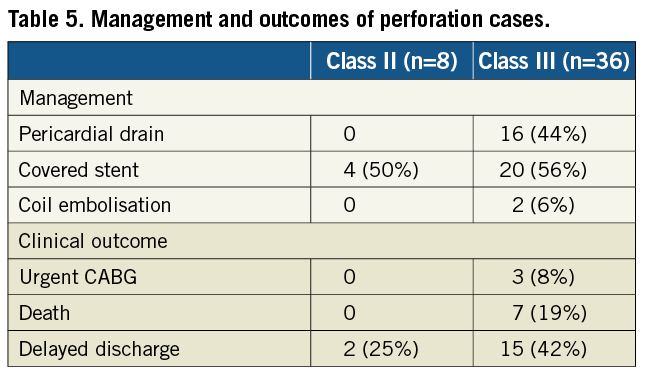
Table 5 shows the management and outcomes for the perforation cases. In our series, 24 patients with perforation received covered stents (55%) and two underwent coil embolisation. The remainder of the patients were treated with prolonged balloon inflation and standard bare-metal or drug-eluting stent implantation. Sixteen patients received pericardial drains; these cases were all Ellis class III in severity.
CLINICAL OUTCOME
Three patients underwent urgent CABG. The overall inpatient mortality in our series of coronary perforations was 15.9% (7/44), as compared with a mortality of 0.40% (32/7,859) for patients who did not suffer a perforation. Discharge from hospital was delayed in seventeen patients (39%) with perforation.
The factors associated with death after perforation were a non-elective procedure (p=0.028) and insertion of a pericardial drain (p<0.001).
Details of the seven fatal perforation cases are shown in Table 6. All deaths occurred in patients with Ellis class III perforations and all patients received a pericardial drain. There was a high frequency of other supportive measures including temporary pacing wire (4/7) and intra-aortic balloon pump insertion (4/7). Most (6/7) of the cases were in patients with acute coronary syndromes. Although attempts were made to deliver covered stents in all of the cases, successful deployment was only possible in five patients. In the other two cases it was not technically possible to deliver the covered stent to seal the perforation; one of these patients underwent emergency CABG because of ongoing bleeding and died three days later of multi-organ failure. In the other patient thrombotic occlusion of the culprit vessel occurred sealing the perforation. Six of the deaths occurred despite sealing of the perforation. In five of these, the culprit vessel thrombotically occluded and the patient died of cardiogenic shock. One patient developed rapidly progressive disseminated intravascular coagulation (DIC) and died of internal haemorrhage. This patient had received a significant volume of auto transfused blood from the pericardial drain and several units of blood before a covered stent could be deployed.
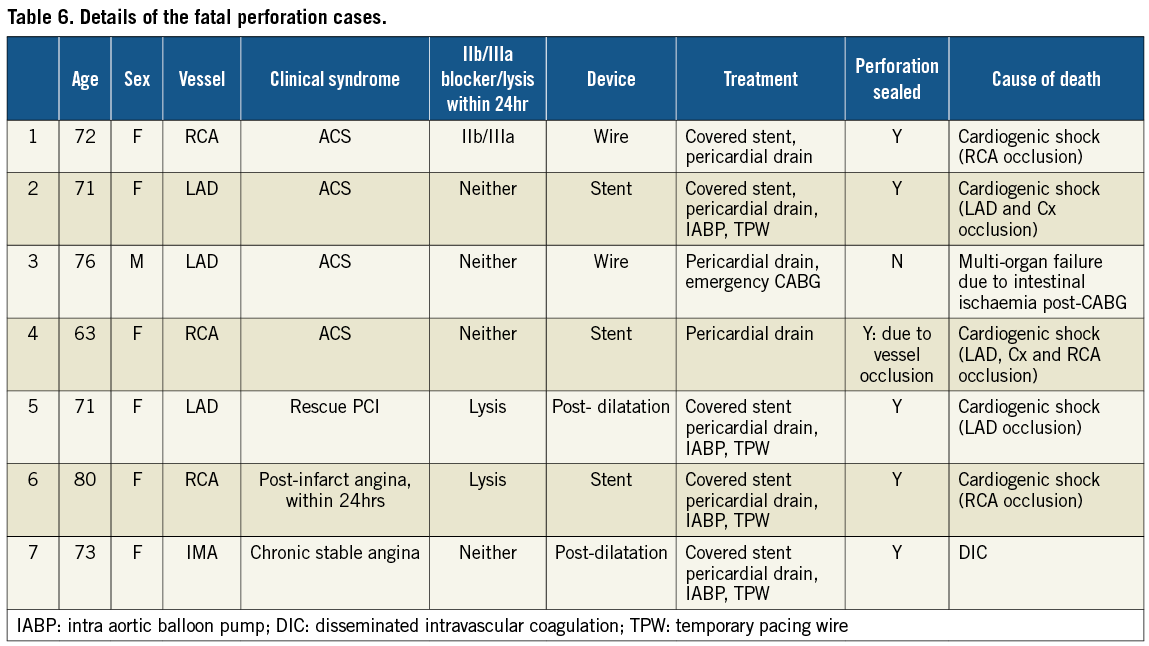
In two patients, occlusion of multiple coronary arteries occurred. An example is patient 4 who underwent angiography following an acute coronary syndrome (ACS) that showed two vessel disease. PCI to the proximal left anterior descending (LAD) artery with a single stent was uncomplicated but perforation occurred during treatment of the second lesion in the right coronary artery (RCA). It was not possible to deliver a covered stent but thrombotic occlusion of the proximal RCA occurred sealing the perforation. The patient rapidly developed cardiogenic shock and visualisation of the left coronary artery showed that the LAD stent had also occluded. Attempts to open this were unsuccessful with thrombus propagating back into the left main stem (LMS) occluding the circumflex, and resulting in death.
Discussion
In this study we report the incidence, management and outcomes of coronary perforation complicating PCI at a large UK tertiary referral centre over a four-year period. The incidence of significant (Ellis class II or III) perforation in our study was 0.56% with a mortality rate of 15.9% after perforation, which is comparable to that of previous published series (Table 7). The high rate of DES usage during this period (77%) and complex lesions (86% class B2 or C) reflects the fact that this study accurately represents the challenging case mix encountered in tertiary centres in the modern “DES era” of interventional cardiology.
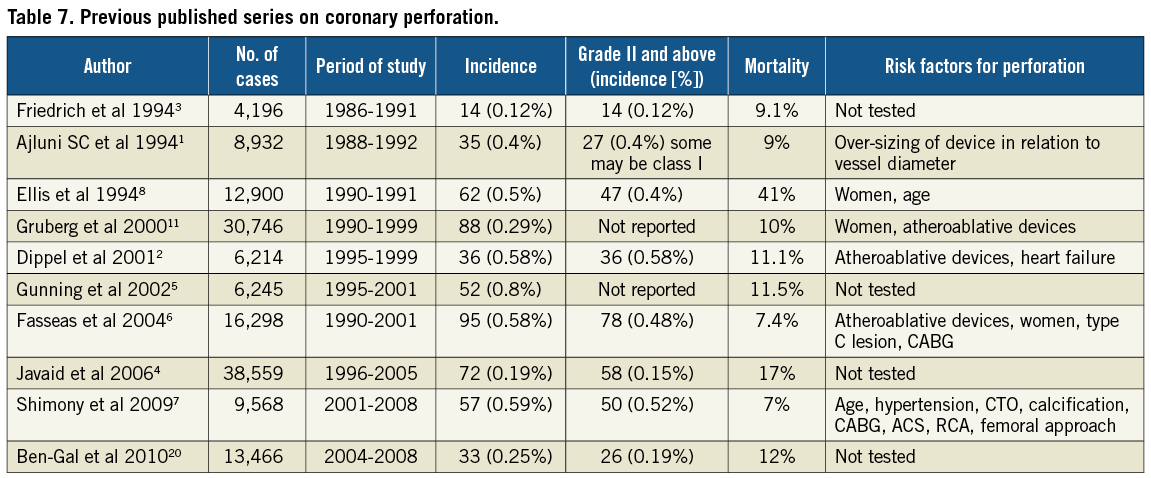
In this study female gender, increasing age, treatment of a chronic total occlusion, angiographic evidence of calcification, and use of a cutting balloon or rotational atherectomy were all associated with an increased risk of coronary perforation. These findings are broadly in keeping with those published studies that have examined risk factors (Table 7). Female gender and increasing age, for instance, have consistently been identified as risk factors for perforation since the original paper by Ellis and colleagues from the balloon angioplasty era6-8,11.
The association of cutting balloon atherotomy with coronary perforation in our study is in keeping with the Cutting Balloon Global Randomised Trial in which the rate of perforation with cutting balloons was 0.8% in comparison to a 0% rate in those treated with balloon angioplasty alone12. Interestingly, although use of rotational atherectomy was associated with perforation in our series, perforation only occurred during subsequent balloon dilatation and stent deployment. Therefore, operators should be aware that coronary perforation may occur during lesion treatment following apparently successful rotational atherectomy.
We have confirmed the serious nature of class III perforation, which carried a mortality rate of 19%. Additionally, in our series no patient died directly as a result of ongoing bleeding from an unsealed perforation. This has not been reported previously.
With the widespread utilisation of primary PCI for treatment of acute myocardial infarction it is reassuring to note that wire tip perforation did not occur in any of these patients in our series. This is of particular relevance as front-loading with antithrombotic drugs is desirable in the primary PCI setting. Seventy percent of wire tip perforations (n=7) occurred in occluded vessels with six of these representing chronic total occlusions.
High pressure post-dilatation following stent deployment is routine practice in our centre (stents are commonly deployed at 16-18 atmospheres and post dilated with pressures of 20 atmospheres) and atherectomy devices are used as part of our extended practice. It is therefore reassuring that the incidence of perforation and overall mortality does not appear to have increased compared to previous series, which have largely assessed practice prior to the DES era.
Many previous studies of perforation have not included a control group and have not attempted to identify risk factors. A recent paper by Shimony and colleagues examined risk factors for perforation between 2001 and 2008, using a randomly-assigned case control group. They found that the mortality rate after perforation was 7%, and that the strongest predictor of perforation was treatment of a chronic total occlusion7. Their series differed from ours in that it represented a lower risk cohort, with 12% of patients having type A lesions, and included patients treated prior to the widespread introduction of DES. This study also did not include any patients treated with atherectomy devices.
Additional data provided by the large European dual centre analysis by Al-Lamee et al13 identified a cohort with similar lesion characteristics to those treated in our centre and demonstrated medium- to long-term outcomes after perforation, with a 41% major adverse cardiac events (MACE) and 15% death rate at follow-up. It follows therefore, that patients surviving perforation are at high risk of events and should be closely monitored.
Management of coronary perforation is aimed at stopping coronary extravasation and treating any resultant haemodynamic compromise. The initial management in all cases is usually immediate balloon inflation at or proximal to the site of perforation. In mild cases prolonged balloon inflation and deployment of a standard stent (if perforation occurred prior to stent deployment) may be sufficient to seal the perforation. Specific percutaneous treatments directed at the site of extravasation include coil-induced occlusion of the site of the leak and deployment of covered stents, which are usually manufactured from polytetrafluouroethylene (PTFE)14-17.
In our series, covered stents were used after perforation in 55% of cases. Unfortunately PTFE-covered stents are bulky and notoriously difficult to deliver, particularly in tortuous, calcified vessels and, of the seven fatalities, there were two cases in which the operator was unable to deliver a covered stent. An additional limitation of PTFE-covered stents is the higher rate of stent thrombosis compared to both bare-metal and drug-eluting stents18. There are recent reports of successful use of a novel pericardial-covered stent (Over and Under®) to seal the site of perforation, and these stents have been reported to have improved deliverability in comparison to PTFE coated stents19. The Over and Under® (ITGI Medical, Or Akiva, Israel) stents are deliverable through a 6 Fr sheath, and are available in a variety of sizes.
In cases with haemodynamic compromise, insertion of a pericardial drain to relieve tamponade should be promptly performed and general supportive measures, including intravenous fluids and inotropic support may be required. Blood and coagulation factors to reverse the effect of antiplatelet and anticoagulant agents can be given. Urgent CABG is indicated for an ongoing leak despite percutaneous treatment. In our study all pericardial drains were inserted for class III perforations and unsurprisingly drain insertion was a strong risk factor for subsequent death.
One recent publication from the United States has suggested treating severe perforation by use of a dual catheter approach to enable rapid insertion of a covered stent with minimum time elapsed from deflation of the balloon. Although this did not show a significant improvement in outcomes it represents a welcome addition to the techniques that can be used in the setting of perforation20. One of the patients in our series was managed with this technique, which is illustrated in Figure 1.
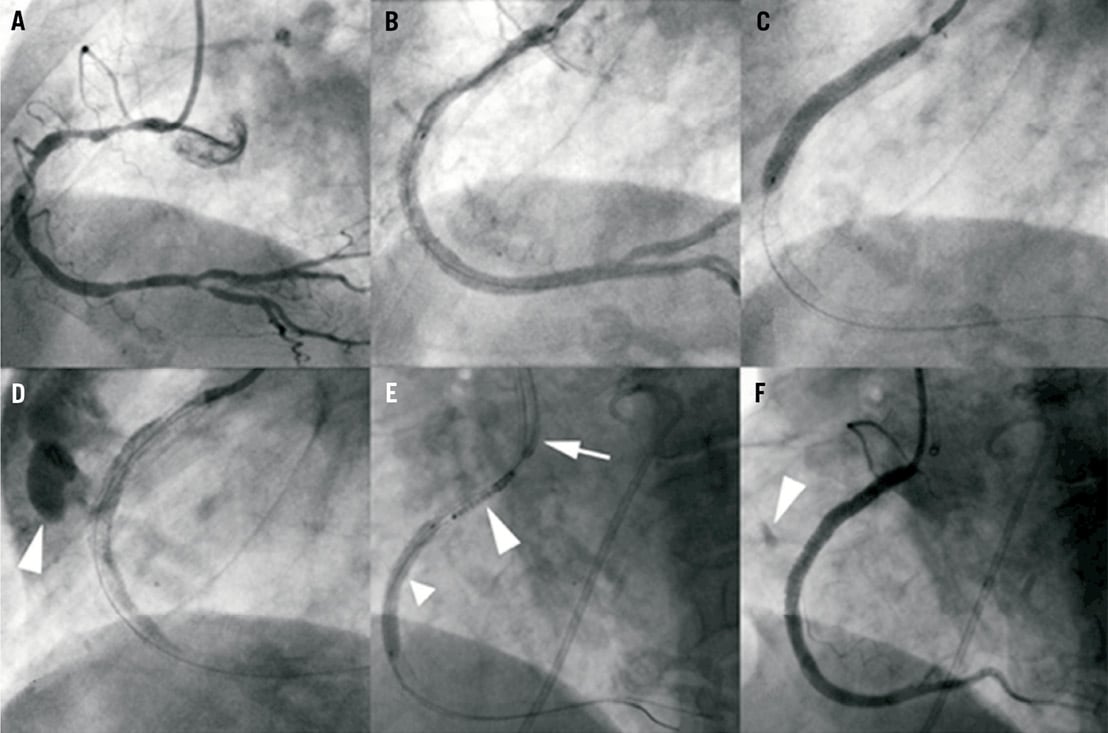
Figure 1. Diagnostic angiography of the right coronary artery (RCA) reveals diffuse severe disease (panel A). Following stenting of the distal and mid-vessel, a 4×38 mm TAXUS® drug-eluting stent (Boston Scientific, Natick, MA, USA) is positioned in the proximal vessel overlapping the distal stent (panel B) and deployed (panel C). Immediately post deployment there is frank contrast streaming into the pericardial space (arrowhead) representing an Ellis grade III perforation at the distal end of the stent (panel D). The stent balloon is immediately re-inflated to seal the leak and a pericardial drain is inserted because of haemodynamic compromise. A dual catheter technique is utilised for further treatment (panel E): a second guide catheter is placed outside the RCA ostium (arrow), the stent balloon (small arrowhead) is briefly deflated, a second guidewire is passed into the distal vessel and the balloon is re-inflated. A covered stent is then positioned in the vessel on this wire (large arrowhead) proximal to the inflated balloon. The balloon is deflated and withdrawn with the initial guidewire, and the covered stent is positioned at the site of perforation and deployed. The final angiogram following covered stent deployment (panel F) shows the leak has been sealed although there is some minor contrast staining still visible (arrowhead).
OUTCOME
Previous studies have shown class I perforations have a good outcome2,4,9,10 and these were therefore not included in this study. Our study did confirm the relatively benign consequences of class II perforations, with no deaths or need for a pericardial drain or urgent CABG. This concurs with the majority of previously published series2,7,9 but contrasts with the series of perforations reported by Javaid4 in which 12% required pericardiocentesis and 27% emergency bypass surgery4. This disparity may well be due to differences in classification of perforations using the Ellis system, which is to some extent subjective.
Our study confirmed the serious nature of class III perforations6,7. All cases of pericardial drain insertion, urgent CABG and all deaths occurred in these patients and the mortality within this group was 19%. Urgent CABG has been previously reported to carry an operative risk of death of up to 15%21. In our study three (8%) of patients with class III perforation underwent CABG, one of whom died.
Insertion of a pericardial drain and a non-elective procedure were identified as risk factors for death following perforation. An important finding of our study, which has not been reported previously, is that no patient died directly as a result of ongoing bleeding from an unsealed perforation. In most cases the major contributor to death was acute occlusion of the target vessel resulting in cardiogenic shock, which occurred in some cases despite successful stenting.
Hypotension secondary to tamponade and blood loss is likely to be a major driver of this phenomenon and this lends more import to the rapid insertion of a pericardial drain and maintenance of an effective circulating blood pressure with supportive measures. As most of the deaths (6/7) were in patients who had suffered an ACS, the prothrombotic milieu of this condition may also have contributed. In two patients, occlusion of multiple coronary arteries occurred with predictably grave consequences.
It is possible that routine administration of protamine to reverse procedural anticoagulation may exacerbate the problem of coronary thrombosis, and may not be necessary given the ability to seal perforation in almost all cases with modern interventional techniques. As a result, protamine is no longer routinely used in our centre in cases of perforation due to the problems described with acute thrombotic vessel occlusion. Al Lamee et al recommend the use of protamine “as necessary” in the setting of coronary perforation if heparin or glycoprotein inhibitors have been administered13.
In terms of future treatment for perforation, pericardium-covered stents (e.g., Over and Under®) have been developed, which are more deliverable than PTFE-covered stents19. However these were not available during our study period and there are currently no published outcome data available on these devices.
Limitations
Our report has a number of limitations. It is a retrospective study and this raises the possibility that some less severe cases may have been missed. However it is unlikely we missed any clinically important cases given that perforation is a mandatory field for completion in the BCIS-CCAD database and all cases of tamponade, dissection and PCI-related deaths were also reviewed. Data was not available on vessel and balloon sizing, use of direct stenting or stent deployment and balloon dilatation pressures for this cohort. As coronary perforation is rare, numbers were low despite the large number of overall cases and this limits the statistical power. For the control group the limiting factor is that data are limited to the specifics of the BCIS-CCAD database and to aid further analysis we have amended the data fields recorded in our centre to include characteristics of interest to us in future.
Conclusions
This retrospective study was carried out in a single high volume tertiary centre in the United Kingdom, during a period of four years when the treatment of severe coronary artery disease was constantly evolving. The incidence of perforation and subsequent mortality is similar to previously published data, which is reassuring given the trend to more aggressive percutaneous treatment strategies for very severe coronary disease. Groups at high risk include the elderly, females, those with coronary calcification or receiving treatment for a chronic total occlusion (CTO), and those undergoing treatment with rotational atherectomy or cutting balloons. These factors should be taken into account when assessing individual risk and treatment should be tailored accordingly, with particular attention being paid to lesion preparation and device sizing. We also challenge the widespread belief that administration of protamine is mandatory in the setting of coronary perforation in view of the deaths resulting from acute coronary occlusion.
The authors strongly believe that in a condition with such high mortality, which occurs so infrequently, it is essential to continue to report the data of individual centres so that we may learn from patient risk, procedural factors and treatments of perforation, in order to attempt to improve outcomes and ultimately save lives.
Conflict of interest statement
The authors have no conflict of interest to declare.

