A 54-year-old man with non-ST elevation myocardial infarction (NSTEMI) underwent percutaneous coronary intervention (PCI) for a severe stenosis in the first marginal branch of the left circumflex coronary artery (LCx-OM1) (Figure 1).
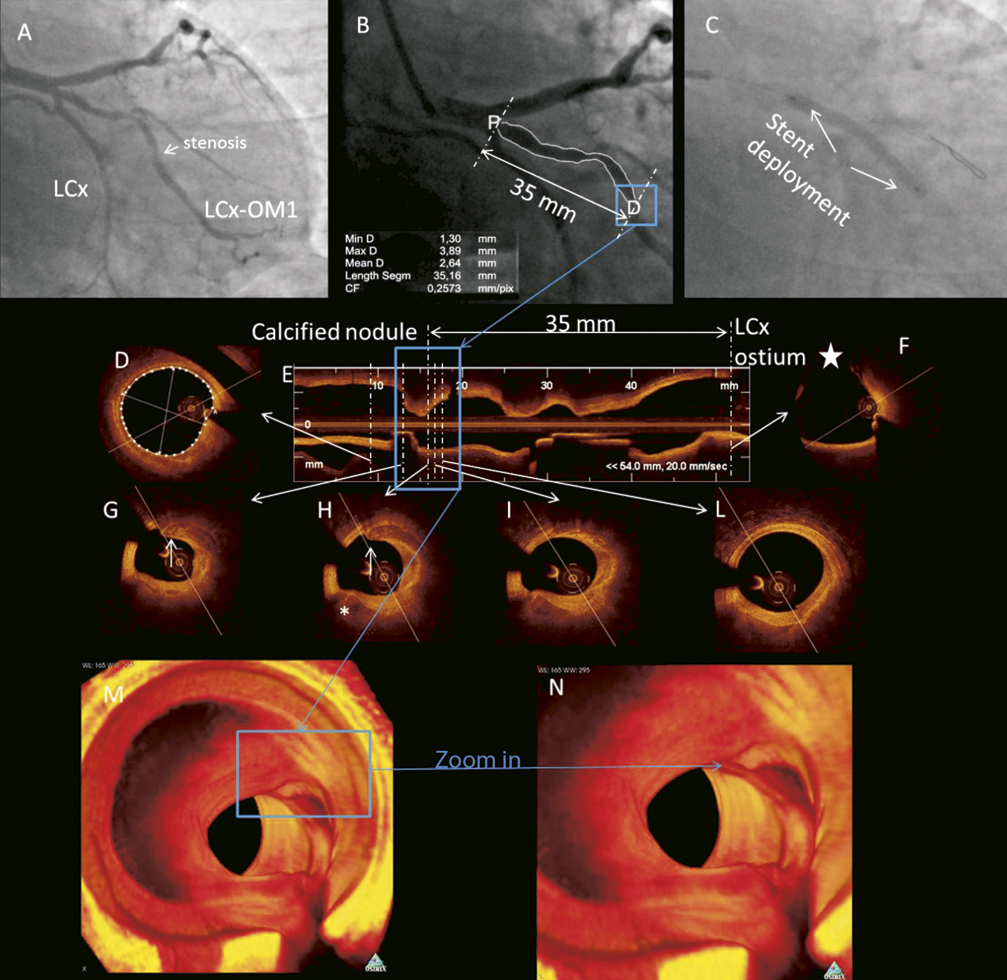
Figure 1. Angiographic and optical frequency domain imaging (OFDI) findings before coronary artery perforation occurred. A) Coronary angiography showing long, severe stenosis (type B of ACC/AHA classification) of the first marginal branch of the left circumflex artery (LCx-OM1). B) Quantitative coronary angiography (QCA) showing that the second area of maximal stenosis is located exactly 35 mm distal from LCx ostium (compare with panel E). C) Coronary angiography shows the inflated 3.5×38 mm XIENCE PRIME (Abbott Vascular, Santa Clara, CA, USA) stent (12 atm) maintaining a balloon/artery ratio of 1.0. D) Distal OFDI cross-section used as reference section had a mean diameter of 3.5 mm. E) Longitudinal OFDI reconstruction showing a long, tandem stenosis with two more severe tracts. Blue box highlights the second most severe tract. Transversal dotted lines and relative arrows show location of specific cross sections (panel D, panels F-L), while two longer transversal lines indicate longitudinal distance (35 mm) between the distal more severe tract with a calcified nodule and LCx ostium (see also panel F and compare with panel B). F) OFDI cross-section showing LCx ostium (star). G) Superficial calcified nodule is imaged, along with another calcified nodule (asterisk) located more deeply in the vessel wall. Minimum lumen area at this point was 2.2 mm2. I-L) The superficial calcified nodule is no longer imaged confirming its limited longitudinal extension (around 2.5 mm). M-N) 3D OFDI reconstruction using volume-rendering techniques by Osirix 3.8.1 (The OsiriX Foundation, Geneva, Switzerland) showing the superficial calcified nodule (blue box) projecting towards the lumen (M). A closer view (N) of the superficial calcified nodule is also shown.
Optical frequency-domain imaging (OFDI) was performed showing a mainly fibrotic plaque with a superficial calcified convex-shaped nodule protruding within the lumen, and located at the level of the most severe stenosis. Direct stenting with an everolimus-eluting stent was successfully conducted.
Angiograms after stent deployment unexpectedly showed coronary blood extravasation through a frank perforation1 (Figure 2). A stent graft was deployed and OFDI was repeated showing that the stent graft perfectly covered the perforation site.
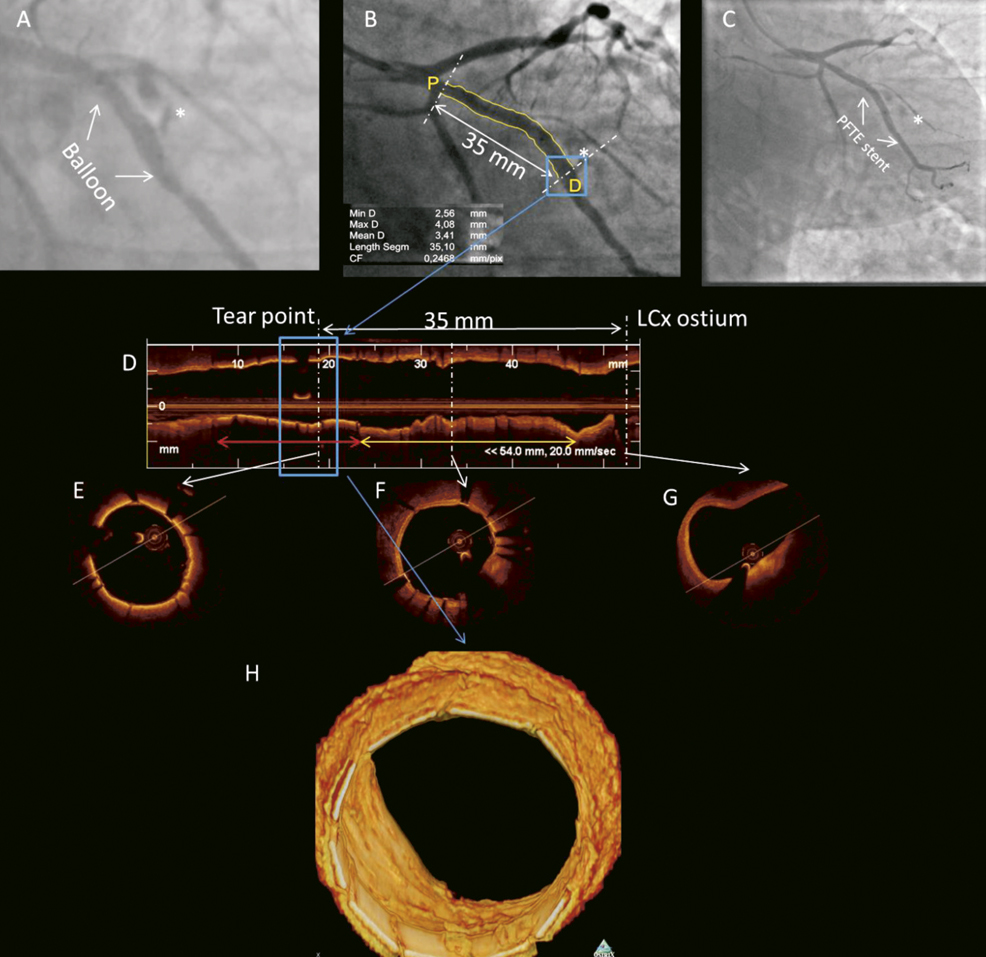
Figure 2. Angiographic and OFDI findings after coronary artery perforation. A) Coronary angiography showing extravasation of blood (asterisk) through a frank perforation (Type III of Ellis Classification). B) QCA analysis showing the perforation site (blue box) located exactly 35 mm distal from LCx ostium. C) Coronary angiography showing deployment of the stent graft (3.5×15 mm Polytetrafluoroethylene-covered Jostent coronary stent graft, Abbott Vascular). D) Longitudinal OFDI view showing the stent graft (red line) and the XIENCE PRIME stent (yellow line). Blue box indicates the perforation site. E) OFDI cross-section showing stent graft. F) OFDI cross-section showing XIENCE PRIME (Abbott Vascular) swtent struts. G) OFDI cross-section showing LCx ostium located 35 mm far from the perforation site. H) 3D OFDI reconstruction using volume-rendering techniques by Osirix 3.8.1 shows stent graft covering the perforation site.
Coronary artery perforation (CAP) is a rare but potentially lethal complication of PCI that occurs in 0.59% of PCIs2,3. The novelty of our findings is that OFDI showed a longitudinally short, superficial, convex-shaped calcified nodule that projected towards the lumen at the site where CAP occurred. Calcified nodules are considered as another type of vulnerable plaque4,5. We speculate that the superficial calcified nodule, protruding significantly into lumen, could have either been dislodged towards deeper vessel layers during stenting, or acted as a fulcrum allowing overexpansion of the stent towards the other side of the artery wall, thus causing CAP.
Conflict of interest statement
The authors have no conflict of interests to declare.

