In this chapter of Tools and Techniques Clinical, management of coronary perforation in the cardiac catheter laboratory is discussed. The following is a summarised overview of this technique. The complete, unabridged version with images is available online at: http://www.pcronline.com/eurointervention/76th_issue/111.
Background
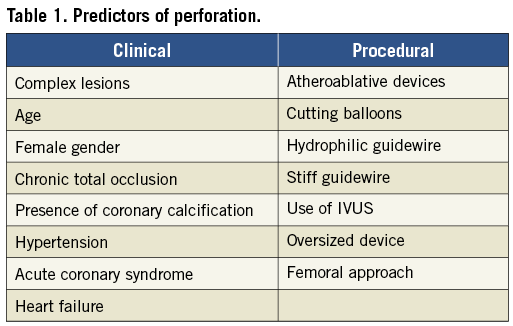
Coronary perforation is a rare (pooled incidence: 0.43%, 95% confidence interval: 0.35-0.52%)1 but serious complication of percutaneous coronary intervention (PCI) that is associated with significant morbidity and mortality (Figure 1). Clinical and procedural predictors of coronary perforation are well described (Table 1).

Figure 1. Ellis classification of perforations2.
Management
Management is dependent upon the Ellis classification. The primary aim is to seal the perforation and prevent cardiac tamponade.
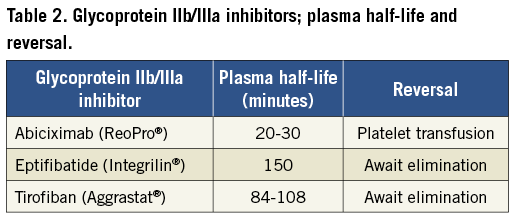
Haemodynamic compromise should be treated with resuscitation; evidence of cardiac tamponade should be sought. If tamponade is confirmed, pericardiocentesis should be performed, preferably guided by transthoracic echocardiography. European Society of Cardiology guidelines describe signs, symptoms and management of cardiac tamponade4. Glycoprotein IIb/IIIa inhibitors should be discontinued on recognition of coronary perforation because their use may be associated with increased risk of major adverse cardiac events (MACE) and greater difficulty in achieving haemostasis5. Intravenous heparin can be reversed with intravenous protamine sulphate (1 mg of intravenous protamine sulphate neutralises 80-100 units of heparin [max. dose 50 mg]).
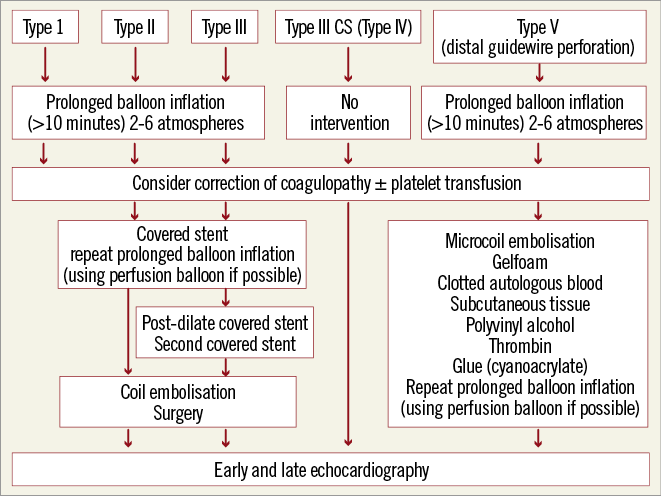
Figure 2. Algorithmic management of coronary perforation3.
Conflict of interest statement
The authors have no conflicts of interest to declare.

