A 67-year-old-man with hypertension and hypercholesterolaemia presented with unstable angina. The patient was admitted and studied with exercise echocardiography showing normal left ventricular function and moderate hypokinesia in the posterior wall during exercise. The coronarography showed a severe lesion in the right posterior descending coronary artery.
The patient was informed of the ABSORB II trial and agreed to participate in the study. The QCA-derived proximal and distal maximal luminal diameters of the segment to be scaffolded were 2.79 and 2.87 mm, respectively. After predilatation with a 2.5×14 mm semi-compliant balloon at low pressure, ECG-gated 45 MHz IVUS imaging was performed (Revolution®; Volcano Corp., Rancho Cordova, CA, USA). The greyscale and virtual histology images showed a severely fibro-calcified lesion with important negative remodelling (35% with respect to the proximal and distal healthy regions).
After IVUS imaging, a new predilatation was performed showing appropriate balloon expansion at 8 atm. Then, an Absorb® 3.0×18 mm BVS (Abbott Vascular, Santa Clara, CA, USA) was implanted (14 atm). Immediately after implantation the patient had severe chest pain. The angiography showed an Ellis type III perforation within the scaffolded segment at the site with negative remodelling. Prolonged balloon inflation and reversion of the anticoagulation with protamine was performed. After five minutes, the perforation was sealed and no further interventions were required. The patient indicated no chest pain and the artery had TIMI 3 flow.
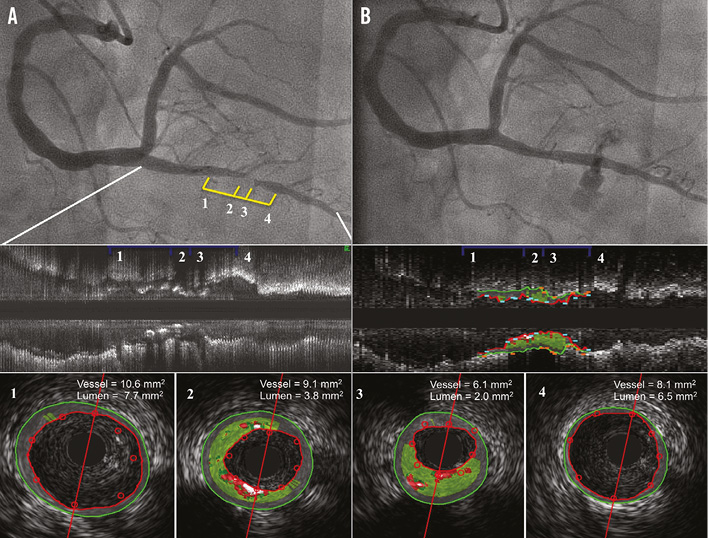
Figure 1. Angiographic and intravascular ultrasound images prior to and after scaffold implantation. A) Severe lesion in the posterior descending coronary artery. B) Coronary perforation immediately after Absorb scaffold implantation. 1) to 4) IVUS images of the posterior descending coronary artery lesion after predilatation.
Conflict of interest statement
The authors have no conflicts of interest to declare.
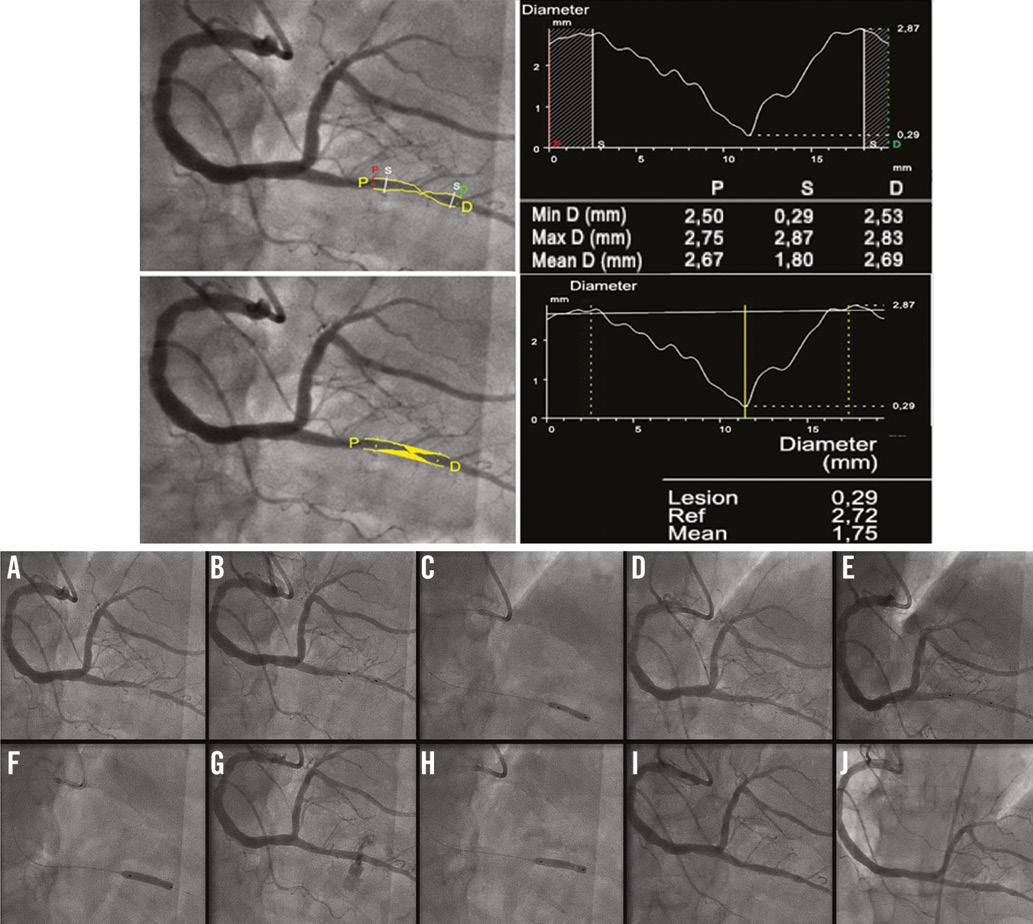
Appendix Figure 1. QCA measurements before scaffold implantation (top) and angiographic images of the coronary intervention and one-month follow-up control (bottom). A) Atherosclerotic lesion located in posterior descending coronary artery. B) Positioning of a compliant balloon 2.5×14 mm. C) Balloon inflation at 8 atm. D) Angiographic result after balloon predilatation. E) Positioning of a 3.0×18 mm bioresorbable scaffold. F) Scaffold implantation at 14 atm. G) Coronary perforation within the scaffolded segment. H) Prolonged balloon inflation (4 mins) and reversion of the anticoagulation with protamine. I) Final angiographic result at index procedure. J) Angiographic control at one-month follow-up.

