Abstract
Aims: To investigate the prognostic value of coronary dominance for various adverse clinical events following the implantation of drug-eluting stents.
Methods and results: We assessed two-year follow-up data of 1,387 patients from the randomised TWENTE trial. Based on the origin of the posterior descending coronary artery, coronary circulation was categorised into left and non-left dominance (i.e., right and balanced). Target vessel-related myocardial infarction (MI) was defined according to the updated Academic Research Consortium (ARC) definition (2x upper reference limit of creatine kinase [CK], confirmed by CK-MB elevation), and periprocedural MI (PMI) as MI ≤48 hours following PCI. One hundred and thirty-six patients (9.8%) had left and 1,251 (90.2%) non-left dominance. Target lesions were more frequently located in dominant arteries (p<0.005). Left dominance was associated with more severe calcifications (p=0.006) and more bifurcation lesions (p=0.031). Non-left dominance tended to be less frequent in men (p=0.09). Left coronary dominance was associated with more target vessel-related MI (14 [10.3%] vs. 62 [5.0%], p=0.009). Left dominance independently predicted PMI (adjusted HR 2.19, 95% CI: 1.15-4.15, p=0.017), while no difference in other clinical endpoints was observed between dominance groups.
Conclusions: In the population of the TWENTE trial, we observed a higher incidence of periprocedural myocardial infarction in patients who had left coronary dominance.
Abbreviations
ARC: Academic Research Consortium
DES: drug-eluting stents
LAD: left anterior descending artery
LCX: left circumflex artery
MACE: major adverse cardiac events
MI: myocardial infarction
PCI: percutaneous coronary intervention
PDA: posterior descending artery
PMI: periprocedural myocardial infarction
RCA: right coronary artery
STEMI: ST-elevation myocardial infarction
TLF: target lesion failure
TLR: target lesion revascularisation
TVF: target vessel failure
TVR: target vessel revascularisation
Introduction
Left coronary artery dominance is a variant of the normal coronary anatomy, in which the left circumflex artery reaches the crux and supplies both posterior descending and posterolateral branches1,2. A recent post-mortem analysis showed a decreasing prevalence of left dominance with the increase of age, suggesting a worse prognosis for subjects with this dominance pattern3. The database of a registry of patients undergoing cardiac catheterisation for acute coronary syndromes has demonstrated higher all-cause mortality in patients with left dominance4. In addition, a non-invasive study with computed tomography coronary angiography screening of the coronary arteries in a heterogeneous group of patients with chest pain (with or without coronary artery disease) showed left dominance to be an independent predictor of non-fatal myocardial infarction (MI) and all-cause mortality2.
However, there is limited knowledge about the relation between coronary dominance patterns and the risk of various adverse clinical events that can occur following percutaneous coronary interventions (PCI) with contemporary drug-eluting stents (DES). The aim of this study was to investigate the prognostic value of left dominance in relation to post-PCI outcome –in particular the rate of periprocedural MI (PMI), which in current DES studies has the highest incidence of all adverse clinical events5-7. We performed the analyses in patients in the prospective, randomised TWENTE trial5,8, which assessed a population of PCI patients with broad inclusion and only few exclusion criteria, treated with second-generation DES9.
Methods
STUDY POPULATION
The study assessed patients enrolled in the TWENTE trial (ClinicalTrials.gov NCT01066650), which has previously been described in detail5,8. In brief, TWENTE is an investigator-initiated, patient-blinded, randomised non-inferiority study with broad inclusion and limited exclusion criteria in a study population with a majority of complex lesions and “off-label” indications for DES use. The study was performed between June 2008 and August 2010 at the Thoraxcentrum Twente, Enschede, The Netherlands. Patients with an indication for PCI with DES, who were capable of providing informed consent, were randomised for treatment with one of two types of second-generation DES – Resolute (Medtronic Inc., Minneapolis, MN, USA) or XIENCE V (Abbott Vascular, Santa Clara, CA, USA). There was no limit for lesion length, reference vessel size, and number of target lesions or vessels to be treated. As a consequence, in a high proportion of study patients there was advanced coronary disease requiring treatment of multiple vessels, bifurcation lesions, long lesions, and lesions in small vessels5. A total of 52% of patients presented with an acute coronary syndrome but, as a very recent ST-elevation myocardial infarction (STEMI) was the most important exclusion criterion, patients requiring primary PCI were not enrolled. The TWENTE trial has demonstrated a similar clinical outcome for both DES5. The study was approved by the institutional ethics committee and complied with the Declaration of Helsinki. All patients provided written informed consent. The study population of the present analysis consisted of all TWENTE patients except four patients who withdrew their consent during follow-up.
ANGIOGRAPHIC ASSESSMENT OF CORONARY ARTERY DOMINANCE
Coronary dominance was classified into left and non-left by two experienced analysts who inspected the coronary angiography of all TWENTE patients. A coronary artery system was classified as right dominant when the PDA originated from the right coronary artery (RCA), while left dominance was defined when the PDA originated from the left circumflex artery (LCX). A balanced dominant coronary system was categorised when the PDA rose from the RCA in combination with a large posterolateral branch originating from the LCX reaching near the posterior interventricular groove2. Right and balanced were referred to as non-left dominance. Any potential disagreement between analysts was resolved by jointly inspecting all angiographic runs available in order to achieve consensus.
QUANTITATIVE CORONARY ANGIOGRAPHY
Quantitative coronary angiographic analyses were performed offline with the use of edge-detection software (QAngio XA version 7.1; Medis, Leiden, The Netherlands) by angiographic analysts from the Thoraxcentrum Twente5.
FOLLOW-UP AND DEFINITION OF CLINICAL ENDPOINTS
Details of the clinical follow-up have been reported previously5,8. In brief, in the TWENTE trial follow-up data were obtained during two-year follow-up after the index procedure. For any events triggered, all available relevant clinical information was gathered. Clinical event adjudication (follow-up information was available for all patients) was performed by a core laboratory and an external independent research organisation (Cardialysis, Rotterdam, The Netherlands). Clinical endpoints were classified according to the Academic Research Consortium (ARC) definitions10,11. Cardiac death was defined as any death due to proximate cardiac cause (e.g., MI, low-output failure, fatal arrhythmia). MI was defined by any creatine kinase concentration of more than double the upper limit of normal with elevated values of a confirmatory cardiac biomarker (creatine kinase myocardial band fraction or troponin), based on the updated ARC definition of MI. Periprocedural MI (PMI) was defined as MI within 48 hours after PCI10,11. Further classification of MI and MI location was based on laboratory information, electrocardiogram, and/or clinical data. Laboratory information included determination of creatine kinase before PCI and cardiac markers six to 18 hours after PCI, with subsequent serial measurements in case of relevant biomarker elevation or complaints (97% of the cases had at least one blood sampling performed between 12 and 18 hours after PCI). Stent thrombosis was defined according to ARC as definite or probable.
The composite endpoint of target vessel failure (TVF) was defined as cardiac death, target vessel-related MI, or clinically driven target vessel revascularisation (TVR). Target lesion failure (TLF) was defined as the composite of cardiac death, target vessel-related MI, and clinically indicated target lesion revascularisation (TLR); major adverse cardiac events as the composite of all-cause death, any MI, emergent coronary artery bypass surgery, or clinically indicated TLR; and a patient-oriented composite endpoint as the composite of all-cause mortality, any MI, and any repeat (target and non-target vessel) revascularisation5.
STATISTICAL ANALYSIS
Categorical data were presented as frequencies and percentages whereas continuous variables were expressed as mean±standard deviation (SD). To assess potential differences in the prevalence of dominance patterns between younger and older patients, age was categorised using the mean of the total population as the cut-off value. The baseline characteristics were compared using the chi-square test or Fisher’s exact test for categorical variables and one-way analysis of variance (ANOVA) for continuous variables including age, BMI, minimum reference diameter and total stent length, as the data were distributed normally. The Kruskal-Wallis test (non-parametric data) was used to compare the total number of stents placed between dominance patterns, and results presented as median and interquartile range (IQR). Univariate and Cox regression analysis was performed to assess coronary dominance as an independent predictor with respect to the predefined endpoints. Potential confounding was identified if p-values were <0.10 at univariate analysis of the relations between tested parameter and both dominance and predefined clinical endpoints. A multivariate Cox regression analysis was then performed to adjust for potential confounders. The time to MI was assessed according to the Kaplan-Meier method, in which the log-rank test was applied to compare the coronary dominance patterns. Analyses were performed using SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Unless otherwise specified, confidence intervals and p-values were two-sided. A p-value <0.05 was considered statistically significant.
Results
PATIENT CHARACTERISTICS
A total of 1,387 patients were analysed, of whom 136 (9.8%) had left dominance and 1,251 (90.2%) non-left dominance, consisting of 1,077 (77.6%) right and 174 (12.5%) balanced dominance. In all 1,387 patients, follow-up data were available. Baseline characteristics are shown in Table 1. Male gender tended to be more frequent in the left than in the non-left dominance group (78.7% vs. 71.8%, respectively; p=0.087). There was no difference in the prevalence of dominance patterns between patients aged ≤64 and older (p=0.79). Patients with left dominance tended less often to have a previous PCI (p=0.11).
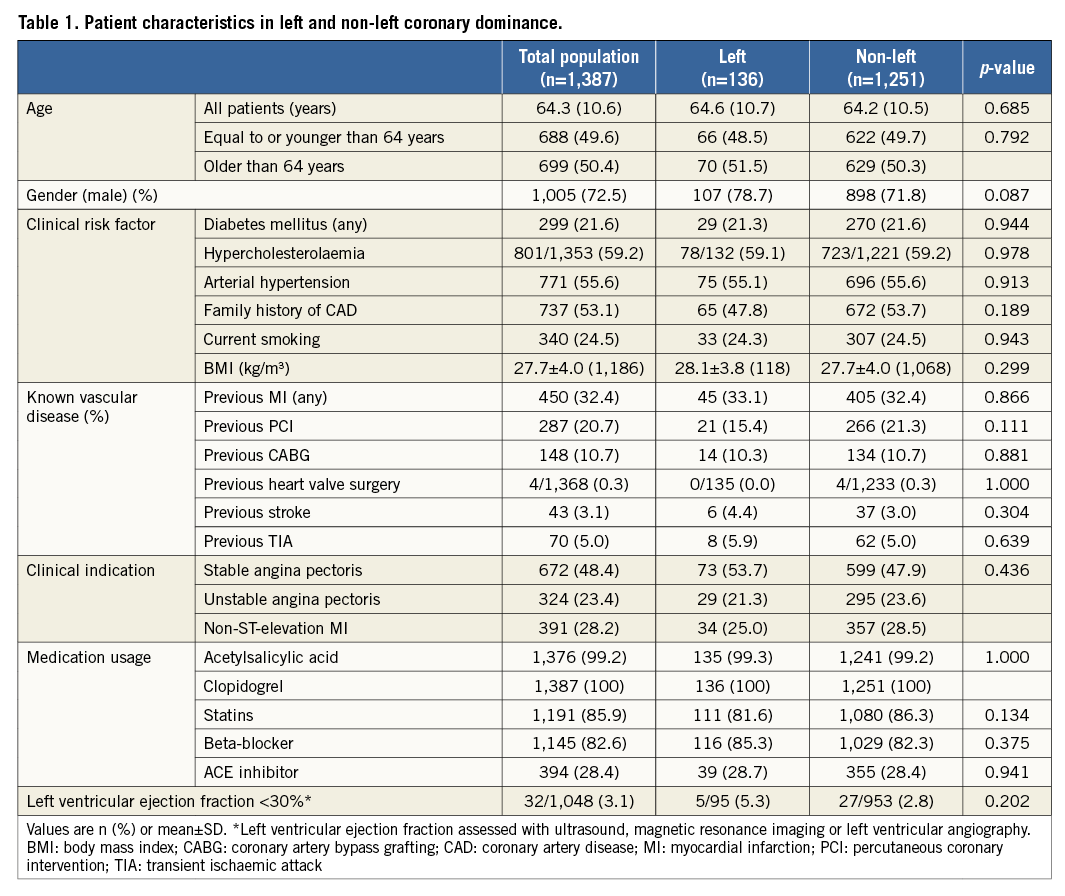
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic analysis revealed that target lesions were more frequently located in the dominant artery (Table 2): left and non-left dominance were present in 64.0% vs. 50.8% if target lesions were located in the left anterior descending artery (LAD; p=0.004), 50.7% vs. 29.4% if target lesions were located in the LCX (p<0.001), and 6.6% vs. 39.4% if target lesions were located in the RCA (p<0.001).
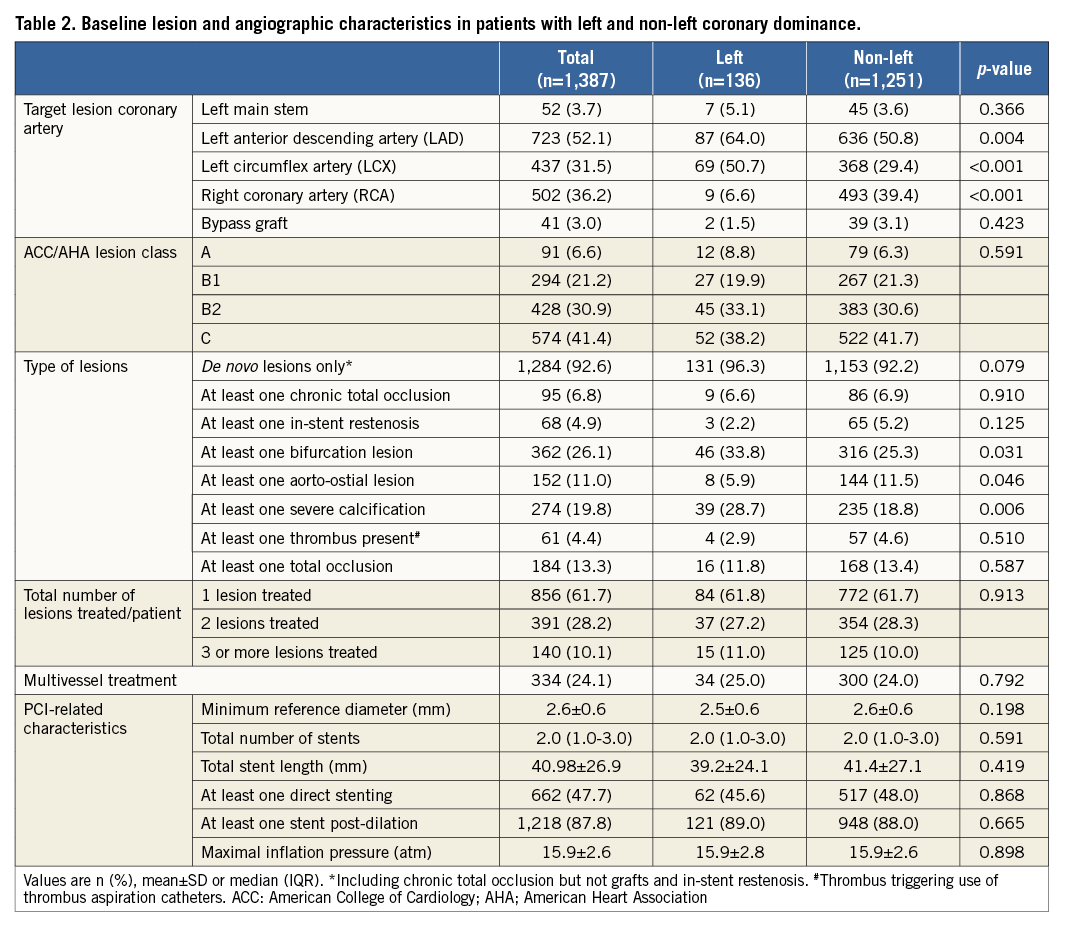
The ACC/AHA lesion types did not differ in complexity between dominance groups (p=0.6). Left dominance was associated with more severe lesion calcification (p=0.006), more bifurcation lesions (p=0.031), and showed a trend towards more de novo lesions (p=0.079). Between dominance groups, there was no significant difference in minimum reference vessel size, the number of lesions treated, and other procedural details.
ADVERSE CLINICAL EVENTS DURING TWO-YEAR FOLLOW-UP
Left dominance was associated with a higher incidence of target vessel MI (p=0.009) (Table 3), in particular non-Q-wave MI (p=0.001) and PMI (p=0.004). For all other adverse cardiac events and composite endpoints, there was no significant difference between dominance groups. Definite or probable stent thrombosis was non-significantly more frequent in patients with left dominance than in non-left dominance (2.2% vs. 1.2%, respectively).
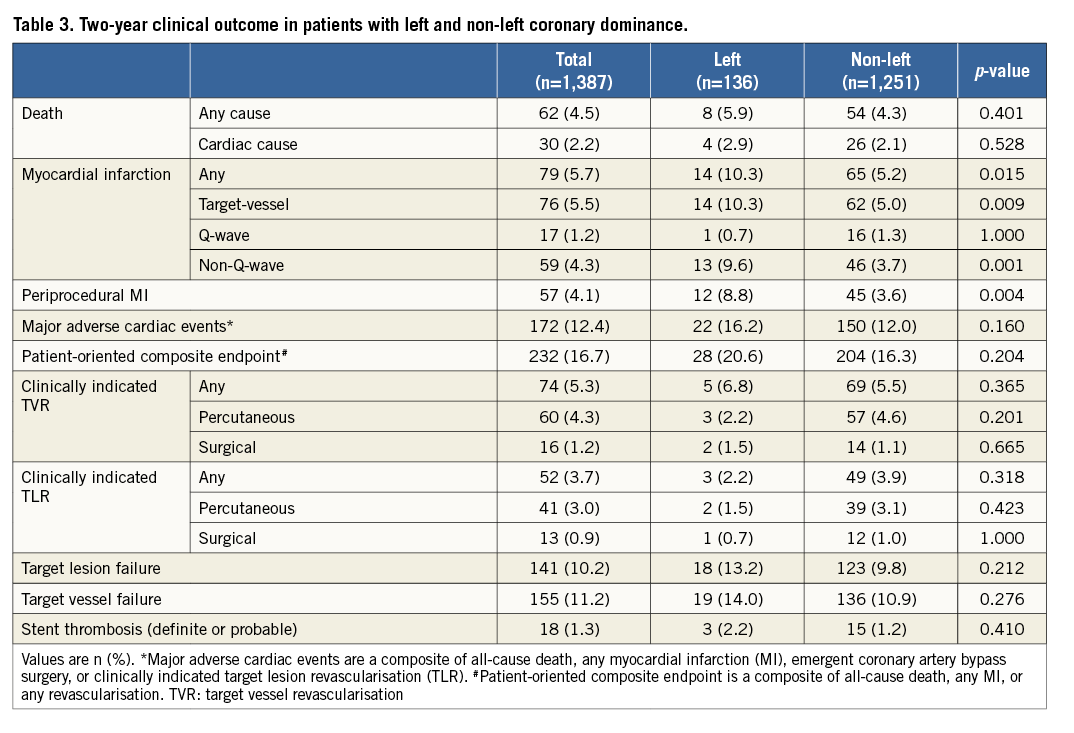
MULTIVARIATE ANALYSIS OF CORONARY DOMINANCE AND MYOCARDIAL INFARCTION
Severe lesion calcification and at least one bifurcated lesion were considered as potential confounders and were therefore included as covariates in a multivariate model. Using the largest group with non-left dominance as a reference, left coronary dominance was shown to be a significant independent predictor of target vessel MI (adjusted HR 1.88, 95% CI: 1.05-3.37, p=0.034) - mainly non-Q-wave MI (adjusted HR 2.35, 95% CI: 1.26-4.36, p=0.007) and PMI (adjusted HR 2.19, 95% CI: 1.15-4.15, p=0.017). In addition, severe lesion calcification and at least one bifurcated lesion were independent predictors for target vessel MI (adjusted HR 2.16, 95% CI: 1.35-3.46, p=0.001, adjusted HR 1.60, 95% CI: 1.00-2.55, p=0.048, respectively) and for non-Q-wave MI (adjusted HR 1.81, 95% CI: 1.05-3.14, p=0.034, adjusted HR 2.00, 95% CI: 1.19-3.56, p=0.009, respectively). For PMI, severe lesion calcification tended to predict PMI (adjusted HR 1.75, 95% CI: 0.99-3.07, p=0.051) and at least one bifurcated lesion was an independent predictor (adjusted HR 2.13, 95% CI: 1.26-3.59, p=0.005). Kaplan-Meier MI-free survival analysis stratified for the dominance groups demonstrated a higher incidence of MI in patients with left dominance (p=0.009) (Figure 1). The MI occurred most frequently as PMI – that is, within the first two days, after which both survival curves showed hardly any change.
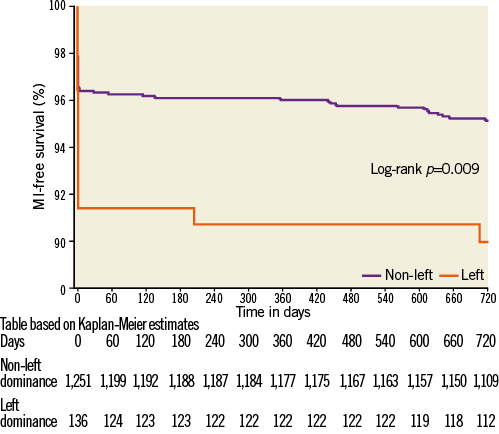
Figure 1. MI-free survival in patients with non-left and left coronary dominance (2-year follow-up).
Discussion
Within the 1,387 patients of the prospective randomised TWENTE trial, left coronary dominance was an independent predictor of PMI following the implantation of contemporary second-generation DES and was associated with a higher MI rate at two-year follow-up. The relation between left coronary dominance and both MI and PMI remained after correcting for confounders, including severe lesion calcification and at least one bifurcated lesion. Despite significant differences in PMI and MI rates at two-year follow-up, no difference in other clinical endpoints was observed between dominance groups. While the present study adds novel information on the relation between coronary anatomy and clinical outcome following PCI, the limited power of the analysis requires that the findings of this study should be considered as hypothesis-generating.
PERIPROCEDURAL MYOCARDIAL INFARCTION
This study demonstrated that left dominance is associated with a 2.2-times higher risk of PMI. The relation between anatomical features such as the coronary distribution pattern and PMI had not been assessed until now. In DES trials, the MI rate is a component of several combined clinical endpoints; the PMI rate represents the vast majority of the MI rate which is an endpoint in both stent trials and pathophysiological studies12-15. The mechanism underlying the increased PMI risk in left coronary dominance is still unclear. Previous studies have demonstrated that complex plaque morphologies and greater atheroma volumes bear a greater risk of significant plaque (micro)embolisation which can lead to microvascular injury16-20. Furthermore, PCI-related (stent-induced) closure of epicardial arteries may lead to blood flow reduction or occlusion in side branches with subsequent myocardial injury16. Both microembolisation and stent-induced closure of very small side branches may not be visible on the angiogram but can lead to cardiac marker release and PMI.
CLINICAL OUTCOME
A few registries and studies have shown relations between left dominance and inferior clinical outcome2-4, but the patient populations of these studies differed significantly from that of the TWENTE trial5. A recently published post-mortem angiography study showed that the prevalence of left and balanced dominance decreased with increasing age3, while we found no relation between age and dominance pattern in the population of TWENTE trial patients, who were on average at a younger age (being normally distributed) than the population of the aforementioned post-mortem study that also comprised a wider age range (with non-Gaussian distribution). In a heterogeneous group of patients with chest pain, computed tomography coronary angiographic screening revealed left dominance to be an independent predictor of non-fatal MI and all-cause mortality2. In addition, in a registry of patients with acute coronary syndromes, left dominance was associated with higher all-cause mortality4.
Our present study in a population of PCI patients with broad inclusion and only few exclusion criteria, consisting almost equally of patients with acute coronary syndromes and stable angina5,9, adds further information on the prognostic impact of left coronary dominance with regard to various aspects of clinical outcome following PCI. Although we did not observe an inferior outcome in terms of higher mortality, treatment failure, or major adverse cardiac events, we found an independent association between left dominance and PMI which, in the presence of major cardiac marker release, may be related to increased mortality16,21-24. Furthermore, in patients with left dominance we observed more bifurcated and severely calcified coronary lesions, lesions with characteristics that are known to be associated with inferior clinical outcome25. While our data may not have direct clinical implications, our findings suggest that further research may be warranted to clarify the role of coronary dominance. Left coronary dominance in the presence of left main disease and a proximal LAD stenosis may sometimes lead to surgical revascularisation or, if PCI is performed, may trigger a more aggressive pharmacological antiplatelet and/or anticoagulation therapy, as the occlusion of a dominant CX artery may induce serious complications. This impact of a dominant circumflex coronary artery on PCI procedural risk is also reflected in the SYNTAX score26,27.
Limitations
The present study is a non-pre-specified post hoc analysis of the TWENTE trial with two-year clinical follow-up. Nevertheless, any prolongation of follow-up would have had no effect on the difference in PMI between dominance groups (PMI may only occur during the first 48 hours after PCI), which was the main finding of this study. In addition, none of the other clinical outcome parameters (i.e., other than MI and PMI) showed a trend towards significant difference between coronary dominance groups. While the adjudication of MI was performed according to the ARC definitions, we did not stratify events for different levels of CK-MB elevation (e.g., >5x or >10x the upper reference limit of CK-MB). In future assessments of this issue, it may be valuable to stratify the CK-MB value to certain levels in order to define the severity of MI better. In addition, we cannot completely exclude that during follow-up a subclinical MI might have been missed, especially if it did not lead to hospitalisation, revascularisation by PCI or CABG, and/or if ECG changes were not recognisable. Because of the limited power of the present post hoc analysis, no definite conclusion can be drawn and findings should be considered hypothesis-generating. Nevertheless, the current findings add novel information on the relation between coronary anatomy and clinical outcome following PCI.
Conclusion
In the population of the TWENTE trial, we observed a higher incidence of periprocedural myocardial infarction in patients who had left coronary dominance.
| Impact on daily practice Revascularisation of a significant lesion in a left-dominant coronary system may be associated with an increased risk of periprocedural myocardial infarction. In such lesions, additional measures to prevent this adverse event may be considered (e.g., more aggressive pharmacological therapy). In the presence of significant left main and proximal LAD disease with unfavourable anatomies, left coronary dominance may sometimes suggest serious consideration of surgical coronary revascularisation. |
Conflict of interest statement
C. von Birgelen was consultant to, and has received lecture fees or travel expenses from Abbott Vascular, Boston Scientific and Medtronic; he received travel expenses from Biotronik and a lecture fee from MSD. The institution has received research grants from Abbott Vascular, Biotronik, Boston Scientific and Medtronic. The other authors have no conflicts of interest to declare.