Abstract
Aims: Using the database from the large-scale, prospective, randomised HORIZONS-AMI trial, the authors sought to assess the impact of bifurcation target lesions (BTL) on angiographic, electrocardiographic, and clinical outcomes in patients with ST-segment elevation myocardial infarction (STEMI) undergoing percutaneous coronary intervention (PCI).
Methods and results: In HORIZONS-AMI, bifurcation lesions in which a provisional approach was planned were eligible for enrolment. By angiographic core laboratory assessment of 3,306 patients with STEMI undergoing primary PCI, 333 patients (10%) had ≥1 BTL, and 2,973 patients had no BTL. There were no significant differences in baseline characteristics between the groups, except for lower left ventricular ejection fraction and more frequent left anterior descending infarct artery in the BTL group. BTLs required longer procedural and fluoroscopy times and higher contrast loads, but rates of TIMI 3 flow post PCI were similar in both groups (with vs. without BTL 99% vs. 87%, p=0.25). ST-segment resolution ≥70% by core laboratory analysis was similar in both groups (48% vs. 50%, p=0.47). Importantly, there was no difference between groups in the rate of death (6.1% vs. 6.7%, p=0.72), definite or probable stent thrombosis (4.2% vs. 5.2%, p=0.42), and ischaemic target vessel revascularisation (14.3% vs. 14.0%, p=0.86) during three-year follow-up.
Conclusions: Although the PCI procedure involving BTL was more complex, the acute results and late outcomes in patients with BTLs were comparable to those in patients without BTLs.
Introduction
The development of atherosclerosis in or next to coronary bifurcations is relatively frequent such that 15-20% of patients undergoing a percutaneous coronary intervention (PCI) have a bifurcation target lesion (BTL). PCI involving BTL remains a challenge for interventional cardiologists. Such procedures are technically complex and are often associated with a higher restenosis rate and worse clinical outcomes1-3.
Data on long-term outcomes of BTLs in ST-segment elevation myocardial infarction (STEMI) after primary PCI are limited. We therefore analysed data from the large-scale, prospective, randomised Harmonising Outcomes With Revascularisation and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial to assess the impact of BTL on angiographic, electrocardiographic, and clinical outcomes in patients with STEMI undergoing primary PCI.
Methods
The HORIZONS-AMI trial was a prospective, open-label, randomised, multicentre trial in patients with STEMI undergoing primary PCI. The study protocol was approved by the institutional review board or ethics committee at each centre, and written informed consent was obtained from all patients. The study design and results have been previously described4-7. Briefly, a total of 3,602 consecutive STEMI patients (≥18 years of age, <12 hours from symptom onset) were enrolled. Patients were randomised 1:1 to either a combination of unfractionated heparin plus a glycoprotein IIb/IIIa inhibitor (abciximab or eptifibatide) or bivalirudin alone. Aspirin and a clopidogrel loading dose (300 mg or 600 mg) were administered prior to catheterisation. After patency was restored in the infarct-related artery, selected patients eligible for stenting were randomised in 3:1 fashion to either a paclitaxel-eluting stent (TAXUS® ExpressTM; Boston Scientific, Natick, MA, USA) or an otherwise identical bare metal (ExpressTM; Boston Scientific) stent. For the purposes of the present pre-specified analysis, data on 3,306 patients with ≥1 significantly stenosed epicardial coronary artery undergoing primary PCI were divided into two groups according to the presence or absence of ≥1 BTL based on core laboratory angiographic assessment. Of note, a single-stent strategy was required for all of these BTLs, with provisional use of a second stent in the side branch allowed for suboptimal results. Patients with BTL in whom a definite two-stent strategy was required (n=37) were excluded from enrolment in HORIZONS-AMI.
The primary endpoints for the HORIZONS-AMI trial were: 1) major adverse cardiovascular events (MACE; death from any cause, stroke, reinfarction and unplanned revascularisation for ischaemia) and 2) major bleeding unrelated to coronary artery bypass grafting (CABG). Net adverse cardiovascular event (NACE) was defined as the occurrence of MACE or major bleeding unrelated to CABG. The definitions of endpoint components have previously been reported4-7. Patients were followed for three years. For the purpose of the present analysis three-year mortality, definite/probable stent thrombosis, and ischaemic target vessel revascularisation were selected as primary outcome measures. All primary endpoint events were adjudicated by an independent clinical events committee blinded to treatment assignment, using original source documents.
Quantitative and qualitative coronary analysis was performed using standard definitions. Infarct artery flow was characterised by the thrombolysis in myocardial infarction (TIMI) classification8. Myocardial blush grade (MBG) was assessed according to the densitometric method, which evaluates the maximal intensity of contrast penetrating the infarct zone in comparison to unaffected territories9.
The sum of ST-segment elevation was measured with lens-intensified calipers to the nearest 0.025 mV, 20 ms after the end of the QRS complex from leads I, aVL and V1 to V6 for anterior myocardial infarction and leads II, III, aVF, V5 and V6 for inferior myocardial infarction. Complete resolution was defined as ≥70% resolution of the initial sum of ST-segment elevation10.
Differences in categorical variables were analysed using the chi-square test or Fisher’s exact test, as appropriate. Continuous data are presented as medians (interquartile range) and were compared using the Wilcoxon rank sum test. The difference in the rates of death, definite/probable stent thrombosis, and ischaemic target vessel revascularisation between groups during the three-year follow-up period was assessed by the Kaplan-Meier method using the log-rank test. Additionally, the relationship between presence of BTL and clinical outcomes was examined with the use of both unadjusted and multivariable-adjusted Cox proportional hazards models. The first Cox model made no statistical adjustments for any covariates. The second model included the following covariates: baseline characteristics and demographics (age, sex, race, body mass index, hypertension, hyperlipidaemia, smoking, diabetes mellitus, insulin-dependent diabetes mellitus, previous myocardial infarction, previous coronary bypass grafting, previous angina, previous congestive heart failure, history of peripheral vascular disease, white cell blood count, baseline Killip class 1, baseline thrombocytopenia, baseline anaemia, creatinine clearance, left ventricular ejection fraction, symptoms onset to first balloon inflation time), pharmacotherapy (randomisation: bivalirudin vs. unfractionated heparin plus glycoprotein IIb/IIIa inhibitor, clopidogrel loading dose, pre-randomisation heparin, baseline aspirin, baseline thienopyridine), and angiographic parameters (left anterior descending artery disease, baseline TIMI flow, baseline reference vessel diameter, presence of thrombus, vessel ulceration, aneurysm, calcification, number of lesions treated, number of vessels treated, lesion length, final TIMI 3 flow). All tests were two-tailed, and a p-value of <0.05 was considered statistically significant. All statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, NC, USA).
Results
Of 3,306 patients enrolled in the study, 333 patients (10%) had ≥1 BTL and 2,973 (90%) did not. Baseline characteristics of the patient population according to the presence of BTL are shown in Table 1. There were no significant differences in baseline characteristics between groups, except for a higher prevalence of left ventricular ejection fraction <40%, a shorter time from symptom onset to hospital arrival, and less frequent presence of diabetes mellitus treated with insulin in the BTL group.
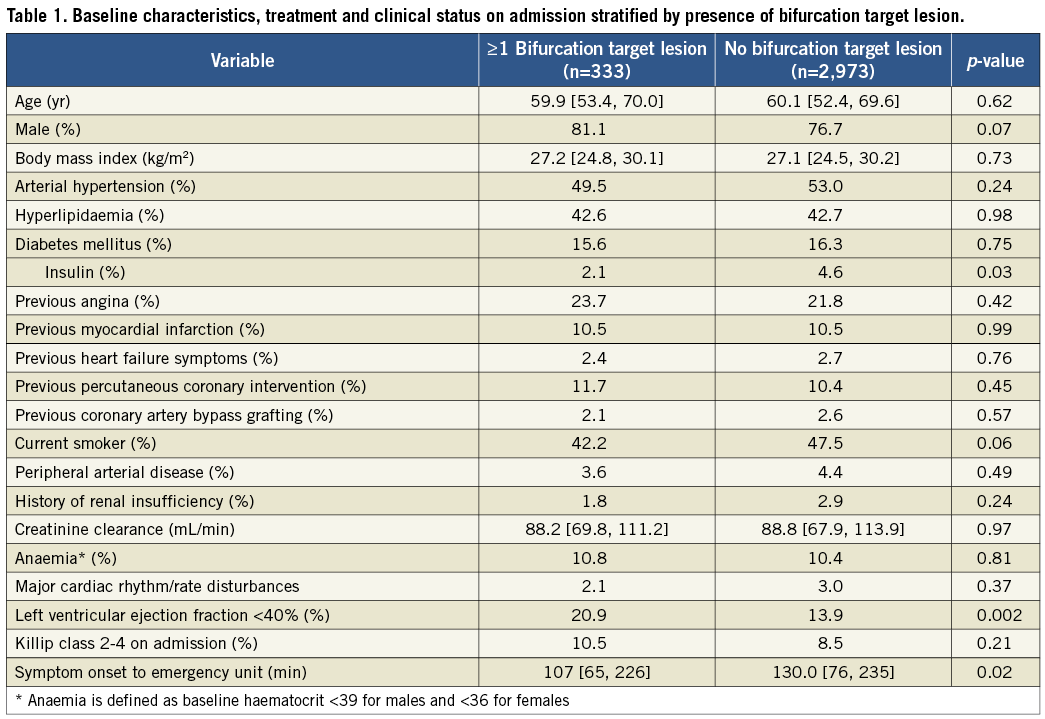
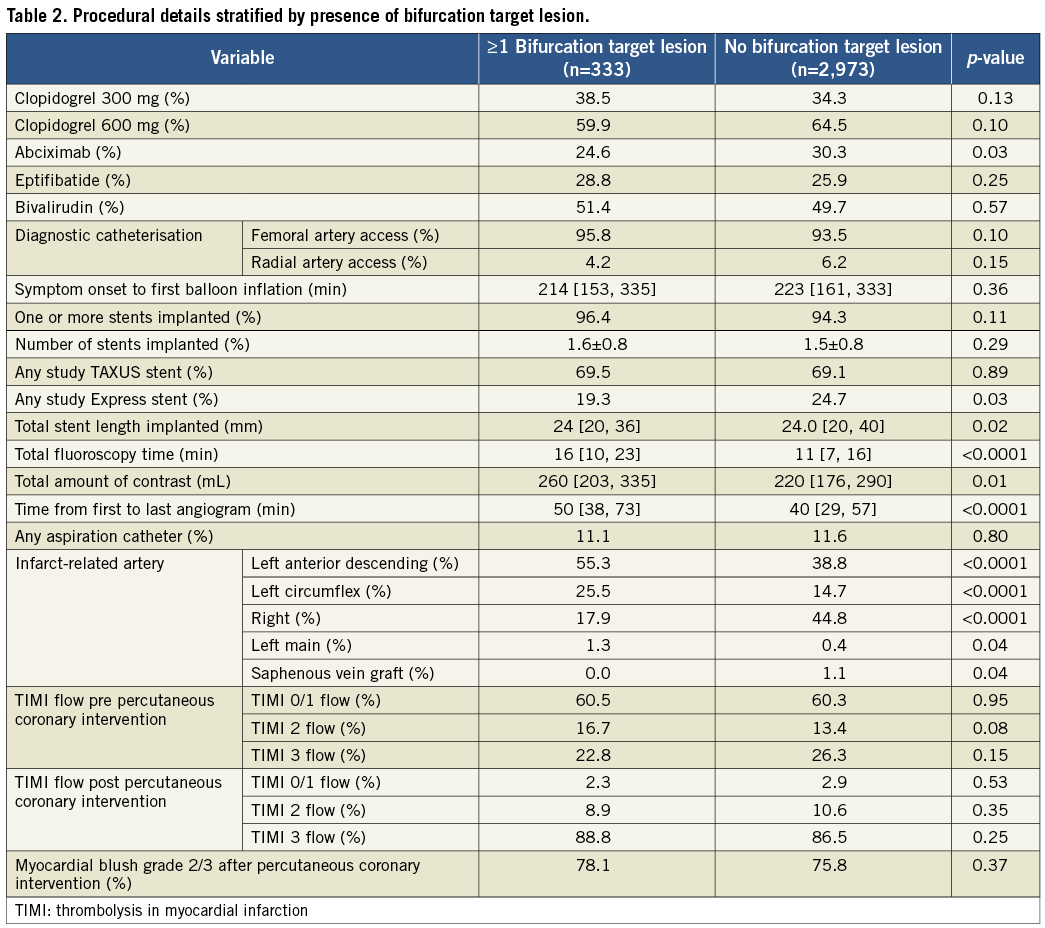
As shown in Table 2, the left anterior descending artery was the infarct-related artery significantly more frequently in patients with BTL. Overall ischaemic time was similar in the two groups. BTLs were treated with mean 1.6±0.8 stents, not different from the non-BTL group. Primary PCI within BTL required longer procedural and fluoroscopy times and higher contrast load, but rates of TIMI 3 flow post PCI were similar in both groups. There was no difference in the rate of final MBG 2/3 after primary PCI between groups (78% vs. 76%, p=0.37).
Complete (≥70%) ST-segment resolution 60 minutes after primary PCI by electrocardiographic core laboratory analysis was similar between the two groups (with vs. without BTL, 48% vs. 50%, p=0.47). As confirmed by both unadjusted and multivariable-adjusted Cox proportional hazards models, there were no significant differences in clinical outcomes during the three-year follow-up period in patients with vs. without BTL (Table 3 and Figure 1). There was no difference in all-cause mortality at 30 days (with vs. without BTL 1.2% vs. 2.5%, p=0.13) or between 30 days and three years (5.0% vs. 4.3%, respectively, p=0.48). Overall three-year mortality did not differ between groups (Table 3).
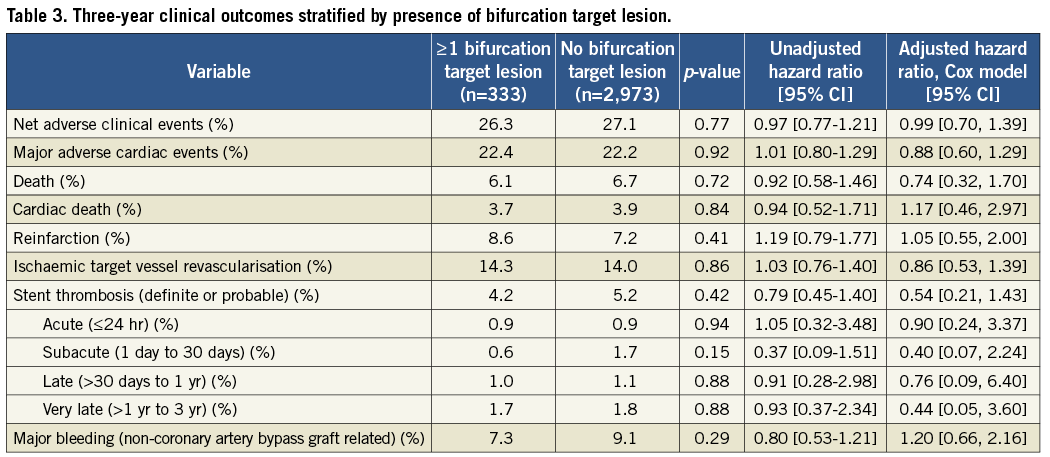
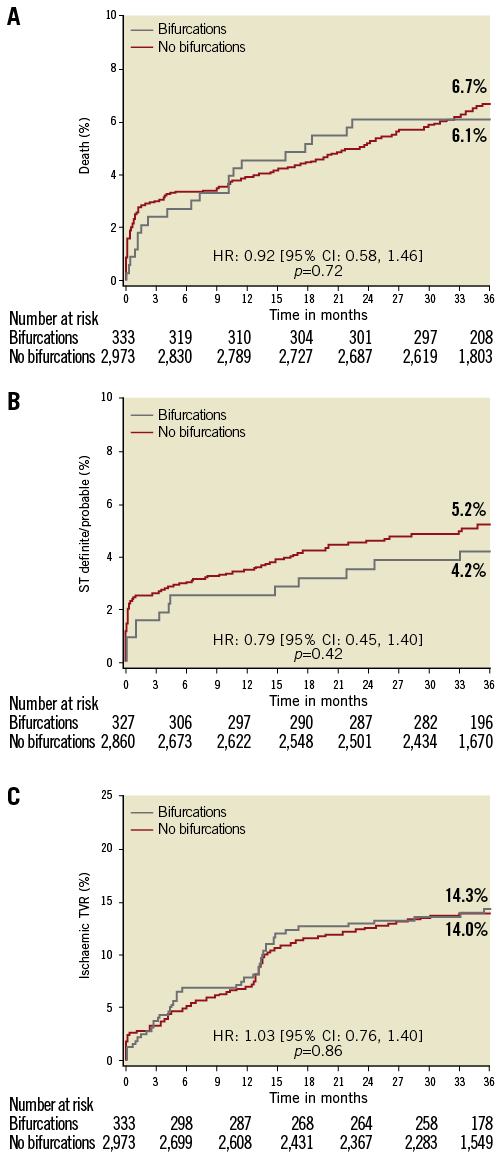
Figure 1. Three-year Kaplan-Meier event-free survival curves for A) death; B) definite/probable stent thrombosis; and C) ischaemic target vessel revascularisation (stratified by bifurcation target lesion presence). ST: stent thrombosis; TVR: target vessel revascularisation
There were 192 patients (60%) with BTL treated with one stent and 129 patients (40%) with BTL treated with >1 stent. At 30 days, there were no differences in the rates of all-cause mortality (1 vs. >1 stent implanted 0% vs. 1.6%, p=0.08), definite/probable stent thrombosis (1.6% vs. 1.6%, p=1), or the rate of ischaemic target vessel revascularisation (1.6% vs. 1.6%, p=1). At three years there were still no significant differences in the rates of all-cause death in BTL patients with 1 vs. >1 stent implanted (5.3% vs. 6.3%, p=0.69), definite/probable stent thrombosis (3.8% vs. 4.9%, p=0.64), or ischaemic target vessel revascularisation (11% vs. 18%, p=0.10).
Discussion
This is the largest study to date specifically assessing the impact of BTL presence on outcomes of patients undergoing primary PCI for STEMI. In contrast to the results from prior series of patients undergoing elective PCI, primary PCI of BTL in the present large-scale STEMI study was associated with outcomes comparable to those observed in patients undergoing non-BTL primary PCI.
The impact of BTL on primary PCI outcomes was previously assessed in two studies. Abdel-Hakim et al11 reported the outcomes of 646 patients undergoing primary PCI from a single-centre database. BTL were found in 23% of patients and the provisional T-stenting technique was used in the majority of cases (89%). The frequency of TIMI 3 flow after PCI was 92% for BTL compared with 93% for non-BTL (p=0.65). There were no differences in the in-hospital (13% vs. 11%, p=0.72) or one-year MACE rates (23% vs. 20%, p=0.56)11 . Frangos et al12 reported data from 114 patients with BTL and 114 patients without BTL, matched according to age, sex, and infarct-related artery. A provisional T-stenting technique was used in 93% of patients. Angiographic success rates (residual stenosis ≤30% and TIMI 3 flow in main branch) were similar in BTL and non-BTL patients (97% vs. 99%, p=0.18). There was no difference in acute complications at <24 hours.
The observed frequency of BTL in our study (10%) was somewhat lower than reported in the previous trials of primary PCI11,12 and planned PCI13,14.This difference may in part be related to the protocol-required exclusion of patients who, in the opinion of the investigators, required the implantation of two stents for treatment of BTL. Also, the definition of BTL may vary across the studies (core laboratory vs. investigator assessment). In line with a previous report11, the main difference between patients with and without BTL from the present study was the more frequent involvement of the left anterior descending artery in patients treated with primary PCI within BTL. This difference in infarct location may be the main reason for the lower ejection fraction observed in such patients. Importantly, STEMI related to the left anterior descending artery15 is often responsible, together with other concomitant factors like diabetes mellitus16 and multivessel artery disease presence17,18, for worse outcomes. The frequency of final TIMI 3 flow and complete ST-segment resolution after PCI were similar in both groups. The rates of TIMI 3 flow were lower than reported in the previous studies (with or without BTL), as the present trial used independent core laboratory evaluation rather than investigator assessment.
Similarly to Frangos et al12, we found no differences in mortality and major adverse events rates at 30 days between patients with vs. without BTL. Also, the overall three-year mortality did not differ between groups. The impact of BTL on long-term outcomes is probably small compared to that of other factors (i.e., infarct size, time to reperfusion). The presence of BTL was identified as an independent predictor of stent thrombosis in patients undergoing primary PCI with drug-eluting stent implantation in other series19,20; however, this was not confirmed by the results of our study (in STEMI) as the rates of acute, subacute, late, and very late stent thrombosis were similar in patients with and without BTL. Surprisingly, in contrast to studies assessing the impact of BTL in patients with stable angina, there was no significant difference in ischaemic target vessel revascularisation rates between groups, although a weak trend was present towards a higher rate of revascularisation when more than one stent was implanted. However, there was no impact of stenting technique (1 vs. >1 stent implanted) on other clinical outcomes. The risk of ischaemic target vessel revascularisation in patients after STEMI is frequently lower than in patients without infarction, as the infracted territory may be clinically silent when restenosis occurs. Also, up to 70% of patients in the present study were treated with drug-eluting stents, which are known to reduce the risk of target vessel revascularisation when used for BTL treatment3.
The primary PCI procedure (time from first to last contrast injection) was approximately 10 minutes longer in patients with compared to without BTL, even though door-to-balloon time was similar, suggesting that BTL requires additional interventions after restoration of flow, such as kissing balloon inflation or rewiring of the side branch. Fluoroscopy time was also longer12 due to more complex techniques being required. Despite a higher contrast load in BTL patients, no difference in the risk of contrast-induced nephropathy was observed between the groups.
Limitations
The main limitation of the study is its non-randomised design, as the study is a subanalysis from a large, multicentre trial. In HORIZONS-AMI, bifurcation lesions in which a provisional approach was planned were enrolled, but the technique of bifurcation treatment was not standardised. This was left to the discretion of the operator, and we were unable to assess the impact of BTL treatment strategy on clinical outcomes properly. However, since a two-stent strategy was reserved by protocol for suboptimal results, a bias toward worse outcomes in the two-stent group would have been expected, which was not seen.
Conclusions
In this large-scale multicentre trial of patents with STEMI, primary PCI in BTL was performed in 10% of cases. Although the PCI procedure of BTL was more complex, the acute results and late outcomes in patients with BTL were comparable to those without BTL.
Funding
The study was supported by the Cardiovascular Research Foundation (New York, NY, USA) and with grant support from Boston Scientific (Natick, MA, USA) and The Medicines Company (Parsippany, NJ, USA).
Conflict of interest statement
D. Dudek has grant support from Boston Scientific Corporation, St. Jude Medical and Volcano Corporation. He is also a consultant with Boston Scientific Corporation and St. Jude Medical. R. Mehran has received research grants (institutional) from The Medicines Company, BMS/Sanofi and Lilly/Daiichi Sankyo. She is also a consultant for Abbott Vascular, AstraZeneca, Boston Scientific, Covidien, Janssen Pharmaceuticals, Regado Biosciences, Maya Medical, Merck & Co. and The Medicines Company. G.W. Stone is a consultant with Boston Scientific Corporation. The other authors have no conflicts of interest to declare.

