Abstract
Aims: Conventional quantitative coronary angiography approaches are limited to quantify complex aorto-ostial stenosis. Multislice CT was able to detect and classify coronary plaques, compared with intravascular ultrasound (IVUS). The aim of the present study was to determine the accuracy of multislice computed tomography (CT) in addition to conventional angiography to identify aorto-ostial coronary stenosis characteristics before revascularisation.
Methods and results: Patients with coronary ostial stenosis were selected for the study. All patients had selective coronary angiography and retrospectively ECG-gated multislice CT (Siemens AG, Munich, Germany). IVUS was performed in patients with ambiguous ostial stenosis revealed by angiography. Forty significant aorto-ostial lesions (38 patients) were analysed by two independent observers in comparison with an expert consensus blinded or not to the coronary CT data sets. Using CT in addition to angiography permitted observers to obtain a strong agreement for assessment of calcified lesions (kappa value 0.75), a good agreement for aortic plaques location and ideal stent position in aorto-ostial coronary stenosis.
Conclusions: This study shows that CT associated with an angiogram allows a better identification of aorto-ostial plaques morphology and ideal stent position in aorto-ostial coronary stenosis before angioplasty.
Introduction
Aorto-ostial coronary stenosis is a particular vessel obstruction of >50% in diameter involving the ostium of a coronary artery within 3 mm from the orifice of the aorta1. Angiographic analysis of aorto-ostial stenosis is limited, particularly by the catheter position. It begins with the limitations of the visual interpretation of the angiogram to assess plaque morphology, principally the stenosis location, either coronary, aortic or aorto-ostial such as is seen in atherosclerotic renal lesions. Differentiation between aorto-ostial and ostial lesion appears to be warranted to make a proper decision on angioplasty2. Multislice computed tomography (CT) was able to visualise the wall of the aorta and its relationship with a stenosis in the proximal renal artery3. CT has shown the possibility of detecting and classifying calcified and non-calcified coronary plaques, compared with intravascular ultrasound (IVUS)4-8. Therefore, the aim of the present study was to determine the accuracy of CT in addition to angiography to identify plaque calcifications, plaque location and ideal stent position in aorto-ostial coronary stenosis.
Methods
We performed a contrast-enhanced CT investigation as part of a prospective research protocol in 40 consecutive significant aorto-ostial stenosis on angiography in 38 patients. The protocol was approved by the institutional review committee and patients gave written informed consent. Procedures were in accordance with institutional guidelines. Inclusion criteria was the presence of an angiographic aorto-ostial stenosis >50% in diameter by visual estimation. Exclusion criteria were atrial fibrillation, iodine allergy, renal insufficiency or an unstable clinical condition.
All patients underwent coronary angiography and CT.
To determine the accuracy of the CT scanner to identify aorto-ostial plaques characteristics, a two-step analysis was performed by two independent observers experienced with angioplasty, in comparison with an expert consensus. The expert consensus was composed of two experienced operators with more than four years experience in cardiac CT, and more than 10 years in coronary angioplasty. The expert consensus determined the plaque characteristics and the angioplasty strategy of each aorto-ostial lesion with coronary angiography and CT data sets. The two independent observers firstly assessed the anonymous coronary angiograms blinded to the CT data sets, and secondly assessed the anonymous coronary angiograms with the CT data sets.
Study criteria were: 1) the location of the stenosis, classified as aortic, aorto-ostial or coronary, 2) plaque calcium graded as; 0, none or moderate; 1, important; and 3) the need for aortic stent protrusion to obtain optimal plaque coverage.
Selective coronary angiography (Coroskop; Siemens Medical Systems, Siemens AG, Munich, Germany) was performed. At least two orthogonal views of the target lesion were performed. IVUS was performed in patients with ambiguous ostial stenosis revealed by angiography (Boston Scientific Corp. Cardiovascular Systems, Natick, MA, USA) using a 40-MHz transducer. The CT was performed one to three days after coronary catheterisation. In patients with heart rates > 70 beats/min, a beta-blocker (metoprolol 100 mg) was administered orally 60 min before the CT scan. In the presence of contraindications for a beta-blocker or an unsatisfactory lowering of the heart rate, the scan was performed at even greater heart rates. The CT angiography was performed using a Sensation 16 or 64-slice CT scanner (Sensation; Siemens Medical Solutions, Forcheim, Germany). Contrast test was not performed. A bolus of 80 ml of contrast agent (Iomeron) was injected intravenously. Bolus-tracking technique was used to trigger the MSCT scanning with the region of interest placed at the ascending aorta. A saline chaser was used after the contrast bolus.
The Sensation 64-slice CT scanner acquires 64 overlapping 0.6 mm slices per rotation. The helical pitch was 4 mm/0.5 s, rotation time was 330 ms, and total breath-hold was about 12 seconds (respectively 420 ms and 20 seconds for 16-slice) with simultaneous recording of the electrocardiogram (ECG)-trace. Using retrospective ECG-gating, the optimal ECG-phase providing best image quality was chosen. CT data were transferred to an off-line image analysis workstation (Leonardo; Siemens Medical Solutions, Forcheim, Germany). Based on the original axial images, reconstructions were rendered perpendicular and parallel to the vessel course of each respective coronary artery lesion. Revascularisation decision was performed after both CT and angiogram analysis on all patients.
In-hospital outcomes and follow-up were analysed: >6 month follow-up was performed in case the patient underwent percutaneous coronary intervention (PCI). Data were ascertained through review of hospital notes. Patients with clinical symptoms and abnormal stress tests were referred for a new coronary angiography.
Statistical analysis
Data are presented as mean value±standard deviation. Data analysis was performed using the Statview version 5 statistical software package. The 95% confidence intervals for the kappa statistics were calculated. The kappa values were interpreted on the basis of reports in the literature. A kappa (K) test was used in the present analysis to quantitatively measure the degree of agreement between the consensus and the independent observers with and without the coronary CT. Using this test, concordance may be considered as very satisfactory for values >0.75. It has a maximum of 1 when agreement is perfect, 0 when agreement is no better than chance, and negative values when agreement is worse than chance. Other values can be roughly interpreted as: values less than 0.40 indicate low association; values between 0.40 and 0.75 indicate medium association; and values greater than 0.75 indicate high association between the two variables.
Results
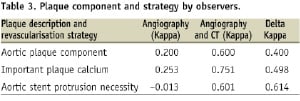
Demographic and main clinical data are summarised in Table 1.
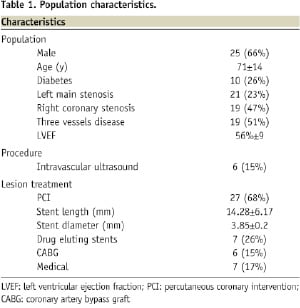
Table 2 presents the different plaque components and angioplasty strategy assessed by the expert consensus for each patient.
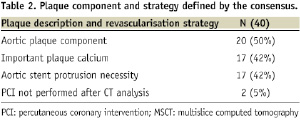
Diagnostic CT image quality was obtained in 35 patients and 37 vessels. Three lesions (7.5%) had motion artefacts but were not excluded. IVUS was performed in six ambiguous lesions (15%), a perfect agreement was obtained with CT for assessment of calcified plaques (K=1). A total of 20 lesions (50%) were classified as aortic or aorto-ostial. Plaque calcium was important in seventeen stenosis (42%). Stent position should protrude into the aorta in 17 (42%). With angiography used by observers (Table 3), a fair agreement was obtained for assessment of aortic and calcified plaques (K=0.20 and 0.25) and no agreement for stent position (K=–0.013).
However, using CT in addition to angiography permitted to obtain a strong agreement for assessment of calcified lesions (K=0.75), good agreement for aortic plaques location (K=0.60) and aortic stent placement (K=0.60).
In this study, the additional mean radiation dose that patient received was respectively 11±4 and 14±5 mSv using a 16 or 64-slice CT scanner.
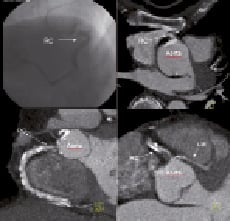
Figure 1 shows angiography and CT of two different patients before stent placement.
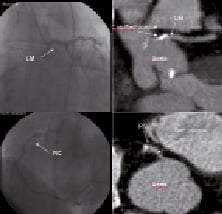
Patient A
Patient B
Figure 1. Coronary angiogram (top left), 16-slice CT longitudinal (top right) of patient A. Longitudinal CT reconstruction showing an aorto-ostial calcified plaque of the left main coronary with aortic component and the necessity for partial aortic stent placement. Coronary angiogram (bottom left), 64-slice CT longitudinal (bottom right) of patient B. Longitudinal CT reconstruction shows an ostial soft plaque of the right coronary without the necessity for partial aortic stent placement. LAD: left anterior descending artery; LM, left main; RC: right coronary
PCI was not performed after CT analysis by all observers in this study, except for two patients (5%). The first case (Figure 2) was a significant right coronary aorto-ostial lesion, angiography underestimated severe calcification of the aortic wall and ostium with a theoretical high risk of aortic dissection during angioplasty.
Patient C
Patient D
Figure 2. Coronary angiogram (top left), 16-slice CT longitudinal (top right) of patient C. Angiography underestimated a severe calcification of the aortic wall and ostium of a right coronary, with a high risk of aortic dissection during angioplasty. 64-slice CT longitudinal reconstructions (bottom left and bottom right) of patient D. Significant right coronary aorto-ostial lesion. CT reveals the proximity of the anomalous origin of the left main coronary artery from the right sinus of Valsalva with a high risk of compression resulting after stenting. RC: right coronary; LM: left main
The second case concerned another significant right coronary aorto-ostial lesion, CT showed the proximity of the anomalous origin of the left main coronary artery from the right sinus of Valsalva with a high risk of compression resulting after stenting9. In-hospital outcome was uneventful when PCI with stent was performed: success was achieved in 100% of the cases. Concerning out-of-hospital outcome, the mean follow-up was 33.4 months (range, six to 48 months). Cardiac-event free survival was 76% (Table 4).
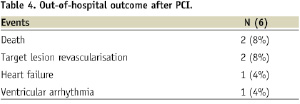
Mortality was 8% (two deaths, one was due to sudden death and the other one was a non-cardiac cause). The rate of target lesion revascularisation was 8%, heart failure associated with supra-ventricular arrhythmia was 4% and ventricular arrhythmia was also 4%.
Discussion
This study shows that CT associated with angiogram allows for a better assessment of aorto-ostial plaques morphology. CT was able to identify different types of coronary aorto-ostial stenosis regarding the plaque location, aortic or exclusively coronary, the degree of calcification with a better reproducibility than angiography10,11. Moreover, ideal stent position could be determined with a better reproducibility than angiography alone (Kappa test values=0.60 or values >0.75).
Angioplasty of aorto-ostial stenosis is associated with lower procedural success and a higher complication rate, a high risk of vessel closure and late restenosis12. Furthermore, the greater possibility of stent misplacement in ostial PCI may contribute to increased rates of restenosis. However, precise stent placement can be difficult. Proximal misplacement may jeopardise the neighbouring coronary ostium by creating a stent “jail”, with or without “plaque shift”. Distal misplacement may result in incomplete coverage of the ostium, resulting in restenosis. Mavromatis et al2 recently reported that distal stent misplacement in ostial angioplasty may have contributed to increased rates of restenosis. The use of CT by observers provides better visualisation of both the angle formed by the junction between the aorto-ostial coronary artery and the aortic wall, as well as aortic plaque position. This information may decrease the difficulty of stent placement, and the possibility of restenosis at this point. The lesion appeared to be a coronary ostial stenosis with angiography, but had an aortic location on CT. We can assume that a reduction in geographic miss for stent placement using CT may improve long- term results. Hence, the visualisation of both calcified and non-calcified plaques is desirable to know if rotational atherectomy is necessary13,14. The use of CT with angiography enabled the observers to classify “massive calcified” and “none or moderate” calcified lesions (Kappa value 0.75).
Figure 3 shows a CT scan of a patient before angioplasty and rotational atherectomy.
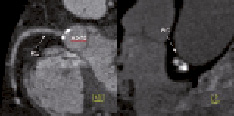
Patient E
Figure 3. 16-slice CT, longitudinal (left) and cross section reconstructions (right) of patient E. CT shows an aortic calcified circular plaque in front of the right coronary ostium. In this case, the consensus and the observers agreed on an aortic stent protrusion. The PCI was performed using rotational atherectomy. During follow-up, a new CT performed for atypical chest pain showed the complete coverage of the stenosis and stent protrusion. RC: right coronary
The rate of drug-eluting stent implantation is low in accordance with French guidelines that consider aorto-ostial lesions as off-label use.
In the case of restenosis and stent protrusion, new catheterisation of the ostium may be challenging. By selecting patients that really need stent protrusion for plaque coverage, CT may decrease the incidence of catheterisation difficulties after stent implantation. However, the catheter has to be very carefully manipulated in order to not damage the stent.
Limitations of the study
The major limitation of this study is the small sample size. In the study, the CT radiation dose was in accordance with Hausleiter et al15. Regarding the high risk lesion, with an expected 31% major adverse cardiac outcome at one year, the long-term radiation-induced risk associated with cardiac CT (0.03% life time cancer risk16) is acceptable.
In practice, the aorto-ostial coronary lesions constitute a major limitation of IVUS, because the catheter is rarely parallel and well centred in the vessel resulting in incorrect plaque assessment. Because high frequency ultrasound does not penetrate the calcium, IVUS can detect only the leading edge and cannot determine the volume of the calcium deposit. However, the arc of calcium and semi-quantitative grading can also be obtained17. In this study, IVUS was performed in six patients and a perfect agreement with CT was obtained for assessment of calcified lesions.
The present study reveals that CT may be a valuable tool for coronary aorto-ostial stenosis analysis before PCI.

