Abstract
Guidance of percutaneous coronary interventions (PCI) by intravascular ultrasound (IVUS) provides more precise information in terms of quantitative measurement and qualitative assessment of coronary artery disease (CAD) than does conventional angiography.1,2 Several studies have tested the efficacy of IVUS to guide stent implantation.3-9 However, the conflicting results have left behind a continued debate as to whether IVUS-guided PCI has an impact on clinical outcome and angiographic restenosis. IVUS and computed tomography coronary angiography (CTCA) share the ability to evaluate the lumen along with the vessel wall, enabling characterisation of proximal and distal reference segments. Nevertheless, IVUS imaging is expensive and usually precluded in severe stenoses. In the present article, we discuss the potential application of CTCA for the guidance of PCI, particularly of complex lesions such as chronic total occlusions (CTO) and bifurcations.
Invasive and non-invasive coronary angiography
Early studies already demonstrated that the extension and severity of coronary atherosclerosis might be greatly underestimated by invasive coronary angiography (ICA), whereas highly accurate measurements could be obtained using intravascular ultrasound (IVUS).10-12 Quantitative angiographic measurements can be misleading since this technique only allows the evaluation of the profile of the lumen.1 Compensatory expansive remodelled coronaries may allow a significant increase in the burden of atherosclerotic plaque without evident changes in the degree of stenosis.11 Such phenomenon may impair the visual interpretation of this technique, yielding a significant interobserver variability and poor in vitro correlation.13
Coronary atherosclerosis is commonly a diffuse disease of the vessel wall, involving long segments of the coronaries, rarely sparing segments. The diffuse distribution of plaque has led to misinterpretation of ICA, eventually having the appearance of small reference vessels with minimal disease.1 Such masking of the true severity and extension of the disease has been depicted by Mintz et al, who showed that reference segments of treated lesions had a mean plaque burden of 51%.2
ICA provides a two-dimensional (2D) view of a three-dimensional (3D) object. To achieve high procedural success rates, lesions should be visualised in at least two orthogonal projections which clearly display the minimum lumen diameter, reference segments, length and shape of the lesion. Foreshortening or vessel overlap can lead to underestimation of lesion severity or inaccurate selection of the length and diameter of the balloon(s) and/or stent(s) to be used, which might result in suboptimal results or the need for additional stents.
In the instance of chronic total occlusions (CTO), large procedural time, with its inherent contrast and radiation issues, can be spent trying to blindly cross a guidewire through a lesion with scarce information regarding tissue characteristics, morphology, path and length of the occlusion.
Three-dimensional rotational angiography systems have addressed some of the limitations of conventional ICA.14 Rotational angiography is a novel method of coronary angiography that involves high-speed panoramic rotation of the imaging camera, providing images of the left or right coronary tree during a single injection of contrast. Although it allows a more detailed evaluation and accurate measurements of bifurcation angles15, it still provides a limited number of projections and a finite range of movement of the C-arm. Additionally, it remains a lumenogram, providing no information on the vessel wall, or about the path of a CTO.
Computed tomography coronary angiography (CTCA) provides a non-invasive examination with 360 degrees of visualisation of the coronary tree, allowing for vessel interrogation from all possible angles. Each artery is segmented individually and therefore is depicted free from foreshortening or branch/vessel overlap providing optimal views of the coronary lumen and vessel wall.
CTCA techniques have recently been developed that extract information from the 2D projections generating a 3D model of the coronary arteries. This dedicated software (Comprehensive Cardiac Analysis, CT TrueView, Version 3.5) analysed on a CT workstation (Brilliance Workspace; Philips Healthcare, Cleveland, OH, USA), calculates the optimal viewing angles for a target lesion of interest and presents them to the user in the form of a four quadrant colour map (optimal view map), representing areas with various degrees of foreshortening, with red corresponding to regions of increased foreshortening and green representing areas with the least amount of foreshortening (Figure 1).

Figure 1. Dedicated PCI planning software, enabling selection of optimal angiographic views. A left circumflex-obtuse marginal bifurcation is shown using a left anterior oblique 41º, caudal 24 º projection, with 0.1% of vessel foreshortening and a bifurcation angle of 63º.
Each of the four quadrants represents a C-arm gantry orientation (LAO-cranial, RAO-cranial, RAO-caudal and LAO-caudal). This optimal view map gives the user the ability to predict the optimal angiographic projection for an individual segment of a coronary vessel. TrueView also provides the length of the lesion of interest as well as the percent diameter stenosis, although the latter has not been validated so far. By providing these lesion parameters and optimal angles for PCI, this application enables the operator an accurate selection of the material to be used, therefore potentially allowing better postprocedural results.
Bifurcations and chronic total occlusions
Percutaneous treatment of bifurcation lesions is commonly associated with worse acute and late outcomes due to a reduced rate of angiographic success and an increased rate of restenosis. One of the mechanisms involved is the occurrence of plaque shifting with associated compromise of the ostium of a side branch and a higher rate of in-stent restenosis at the ostium of the side branch, even with the exclusive use of drug-eluting stents.16-18 Comprehensive pre-interventional three dimensional reconstruction (Figure 1) of the bifurcation angle, as well as lumen and vessel wall involvement of a diseased coronary bifurcation may be important to better plan a percutaneous strategy in particular when plaque shift with compromise of the lumen may be anticipated.19,20
On the other hand, several novel therapeutic approaches, including dedicated guidewires and innovative devices, have been tested for the treatment of CTOs, generally with disappointing results.21,22 This has led to a decrease in the number of attempts of PCI of these lesions, since success rates have remained relatively unchanged over the last years. In ICA, these lesions appear as a stop in antegrade flow of contrast ending at the point of occlusion, unless collateral circulation is developed leaving a missing segment between two vessel ends. Conventional ICA provides no accurate indication of the length or path through the occlusion unless bridging collaterals are present or a biplane angiography is utilised. Likewise, there is no information regarding composition of the “stump”.
Potential of CTCA for the guidance of percutaneous coronary interventions
CTCA has evolved as a tool to identify the extent, morphology and distribution of atherosclerotic plaques in the coronary tree. During the past decade, several studies have evaluated the diagnostic accuracy of CTCA to identify obstructive coronary lesions compared with conventional angiography and IVUS.23-26
Since IVUS provides more precise information in terms of quantitative measurement and qualitative assessment of CAD than does angiography1, several studies from 1998 to 2003 have tested the efficacy of these devices to guide stent implantation.3-9 However, the conflicting results have left behind a continued debate as to whether IVUS-guided PCI has an impact on clinical outcome and angiographic restenosis.
Earlier reports using 16-slice CTCA have shown a reasonably good sensitivity (ranging between 60% and 80%) for the detection of sufficiently large (i.e., with a minimal plaque thickness of at least 1 mm on IVUS) non-obstructive plaques.23,27 Despite sharing the ability to depict the vessel wall and being highly correlated in terms of geometrical parameters, spatial resolution is significantly higher with IVUS than with CTCA (~250 um vs. ~0.4 mm), thereby precluding accurate plaque quantification and characterisation in small vessels, and in patients with very mild atherosclerosis. In turn, IVUS is usually precluded in severe stenoses, since crossing the lesion with the IVUS catheter in such tight lesions might cause ischaemia or result in dissection. Furthermore, in addition to its inherent invasive nature and cost, it is rather cumbersome and time consuming to fully interrogate the main branch and side branch with IVUS.
CTCA angiography allows accurate evaluation of proximal and distal reference segments since the vessel wall is also visualised, allowing for regions of coronary remodelling to be avoided. The drawbacks of vessel and side branch overlap as well as foreshortening, which are dependent on projection angles in ICA, are avoided in CTCA exams since 3D reconstructions allow all possible angles of each vessel to be tracked independently.
The usefulness of CTCA for the guidance of PCI might be highest for planning difficult procedures such as CTO and bifurcations. Unlike ICA, the path of CTO segments are commonly visible by CTCA (Figure 2), thereby facilitating crossing of the lesion. Except in rare cases of absence of collateral filling, there is usually opacification of the vessel lumen distal to the site of occlusion due to retrograde collateral flow of contrast, consequently providing the total length of the CTO.
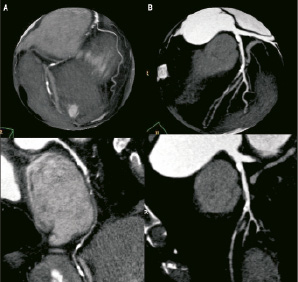
Figure 2. Preprocedural computed tomography coronary angiography of chronic total occlusions might aid discrimination between patients with a low (small reference diameter, very long lesion, calcification and side-branch at entry, diffusely diseased distal coronary bed) and high (short, non-calcified lesion, without side-branch at entry, tortuosisty or angulation and a non-significant calcification 9 mm proximal) likelihood of success.
A recent relatively large CTO registry found that CTCA was more accurate than ICA for defining morphological characteristics of CTOs. Indeed, the only independent predictor of success was the absence of severe calcification estimated by CTCA.28 Besides, preprocedural CTCA can provide information regarding other features related to procedural outcome (although not significant in a multivariate model) such as occluded length, ostial location, stump morphology, side branch at entry, tortuosity, angulation, calcium at entry and exit.
Previous knowledge regarding the anatomy of the aortic root and the coronary arteries, as well as the extent, distribution and characterisation of lesions, might lead to a better selection of catheters and therefore, to shorter procedures. In addition, such a comprehensive preview might aid the interventional cardiologist in the selection of the optimal size and length of stents, therefore resulting in better lesion coverage and larger postprocedural in-stent and reference diameters. Finally, detection of single lesion disease might avoid unnecessary views of non-diseased vessels (Figure 3).
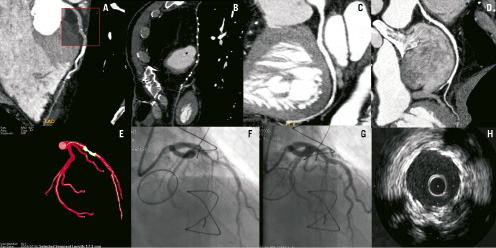
Figure 3. A sixty-one-year-old male with previous CABG and chest pain. Computed tomographic coronary angiography showed an occluded LIMA (Panel B) and a focal mixed lesion at the mid LAD (Panel A). The right coronary artery (RCA) and the left circumflex had mild atherosclerosis (Panels C and D) therefore a single view for the RCA was required and no visualisation of the LIMA was attempted. PCI was planned to revascularise the LAD after selection of the projection with the least foreshortening, without attempting revascularisation of the LIMA. Optimal angiographical and IVUS results were obtained (Panels G and H).
On the other hand, since 6% of PCI patients will undergo non-culprit lesion progression requiring further PCI within the first year of the initial procedure29, the potentially unstable but non-target lesions, commonly deemed non-obstructive by conventional angiography, could also be identified during CTCA and potentially be treated locally or with more efficient systemic therapy to prevent future events.
Limitations
Although CTCA provides a non-invasive method of coronary imaging, the higher radiation dose as compared to ICA still remains a concern. High effective doses for a standard retrospectively gated helical CTCA exam ranging from 12 to 30 mSv have been reported in the literature.30-33 In turn, the effective radiation dose for conventional diagnostic ICA ranges from 5 to 12 mSv.34-37
Radiation exposure of CTCA and its potential association with the risk of cancer has recently been established as a topic of extensive debate. However, cause-effect has never been demonstrated since studies have been performed using Monte-Carlo simulation.38 In addition, it has to be stressed that the lifetime risk of cancer, attributable to CTCA, is similar to the risk related to a stress-rest SPECT or a chest or abdomen CT.39 Radiation issues regarding CTCA are important and indeed radiation doses from CT scans are widely variable between centres. However, significant dose reduction can be achieved using tube modulation (reducing tube current by 80% during the entire R-R interval except from an optimal diastolic window).40 Furthermore, acquisition techniques by means of prospective ECG-gating are currently widely available and allow CTCA acquisitions with similar quality at a minimum radiation expense (1-3 mSv).41 It should be noted that application of CTCA for the guidance of PCI should be only attempted using such low-dose prospective ECG-gating acquisitions.
Other limitations apply to CTCA as well, namely diffuse calcification and lower temporal and spatial resolution compared to ICA. Even with the advent of dual source CT scanners, the presence of diffusely calcified vessels is related to a significant decrease in the positive predictive value.42 Accordingly, luminal diameter measurements by ICA and IVUS remain the gold standard. Nevertheless, current CTCA isotropic spatial resolution of ~0.40 mm allow accurate measurements of “normal” reference diameters and is highly correlated to IVUS measurements. Finally, it should be noted that CTCA data sets should be of optimal quality in order to be applied for the guidance of PCI, without motion artefacts and with a good contrast-to-noise ratio.
Clinical implications
There is enormous potential for CTCA to enhance diagnostic and therapeutic strategies in the management of CAD. Since each artery can be segmented separately eliminating the limitations of foreshortening and vessel overlap, CTCA’s tomographic nature makes it a natural vehicle for pre-planning of coronary and structural heart disease interventions. With its resemblance to IVUS in the capability to assess both the lumen and vessel wall, CTCA provides additional information on the composition of the lesion and reference segments which might allow accurate selection of devices, potentially leading to complete lesion coverage, less incomplete stent apposition, and larger postprocedural diameters.
New techniques such as CT TrueView provide a means to view a 3D reconstruction of the CTCA data and determine the optimal angles and unbiased length of the target lesions(s) before the patient enters the catheterisation laboratory. By integrating this into the interventional suite, the cardiologist can move the C-arm automatically to the desired imaging angle with the least foreshortening, potentially eliminating the need for unnecessary image acquisitions prior to PCI and providing improved device selection. These benefits might potentially appear to be present for the guidance of complex PCI such as CTOs and bifurcations in highly selected patients. In turn, in patients referred to PCI who had a previous CTCA, additional information provided by CTCA might be used at discretion of the operator for PCI guidance. Ongoing research will shed light on whether PCI guidance by low-dose CTCA might be improve procedural and clinical outcomes, and whether its use might be cost effective in selected patients.

