Abstract
Aims: Despite the use of rotational atherectomy (RA) in interventional cardiology for over three decades, data regarding factors affecting the clinical outcomes of the RA procedure remain scarce. The aim of the present study was to describe the contemporary use and outcomes of RA in Europe.
Methods and results: We conducted, for the first time, a prospective international registry in 8 European countries and 19 centres and included patients treated by percutaneous coronary intervention with RA. Between October 2016 and July 2018, 966 patients with complete data were recruited. Mean age was 74.5 years, 72.4% were male and 43.4% had diabetes. Initial presentation was an acute coronary syndrome (ACS) for 25.1% of the patients. Clinical success was observed in 91.9% of the procedures. The rate of in-hospital major adverse cardiac events (MACE) – defined as cardiovascular death, myocardial infarction, target lesion revascularisation, stroke and coronary artery bypass grafting – was 4.7%. At one year, the rate of MACE was 13.2%. Factors independently associated with the occurrence of MACE at one year were female gender, renal failure, ACS at admission, depressed left ventricular ejection fraction (LVEF) and presence of a significant left main coronary artery (LMCA) lesion.
Conclusions: Despite the high level of complexity of the studied population, RA turned out to be an effective procedure with a low rate of in-hospital complications and demonstrated good immediate and midterm results.
Introduction
With the expansion of percutaneous coronary intervention (PCI) indications to more challenging anatomies, and considering the ageing of the population, the proportion of patients with calcified coronary lesions treated by PCI has increased over the past decade. Nowadays, around 20% of patients who are candidates for PCI present with moderate to severe coronary calcifications1. In spite of technological advances, PCI of complex calcified coronary lesions remains a challenge. Indeed, coronary calcification increases the technical difficulties of the procedure, hampering the delivery and expansion of coronary angioplasty balloons and stents, leading to stent underexpansion or malapposition: both conditions increase the risk of in-stent restenosis and thrombosis2. Moreover, coronary calcification also increases the risk of dissection3 and perforation4 during PCI.
Rotational atherectomy (RA) is an adjunctive tool in the armamentarium of interventional cardiologists introduced in 1987 for the treatment of calcified coronary lesions5. In Europe, RA is used in 0.8 to 3.1% of PCI6. The principle of this device is to ablate the calcified atherosclerotic coronary plaque by advancing a high-speed diamond-incrusted elliptical burr in the vessel. RA is nowadays performed to achieve “plaque modification”, using small burrs that facilitate optimised stenting. Randomised trials have demonstrated that an aggressive debulking (i.e., a burr/vessel ratio >0.70) yielded no benefits in terms of procedural success or target lesion revascularisation (TLR) and was associated with more immediate complications7,8. Thus, in most RA procedures, the passage of the burr in the vessel allows the deliverability of a coronary balloon followed by a stent implantation.
However, although RA has been performed for over three decades, data regarding the contemporary use of this technique in daily practice, and its clinical outcomes, remain scarce. We conducted, for the first time, a prospective multicentric international observational registry of patients treated by PCI with RA in order to describe the contemporary use and outcomes of RA in Europe.
Methods
STUDY DESIGN AND POPULATION
The Euro4C registry was a prospective, observational and multicentric European registry conducted in 19 centres, based in eight European countries (France, Poland, Germany, Spain, Italy, Greece, Austria and Russia). Patients included in the study were aged 18 or older and were treated with coronary PCI using RA for at least one lesion, between October 2016 and July 2018. The decision to use RA was left to the discretion of the operator. The study protocol was approved by the institutional review board of each participating centre and all patients gave their written consent to participate in the study. Follow-up was performed by phone call at day 30 and at one year.
DATA COLLECTION
Data at baseline and during follow-up were collected through an electronic case report form (e-CRF). Initial clinical presentation and angiographic data describing the topography and the extent of the coronary disease were recorded.
ROTATIONAL ATHERECTOMY PROCEDURE
RA procedures were performed using the Rotablator™ system (Boston Scientific, Marlborough, MA, USA). Characteristics of the RA procedure were extensively recorded. According to the definition of the European Bifurcation Club consensus9, a lesion was considered a bifurcation lesion if occurring at, or adjacent to, a significant division of a major epicardial coronary artery. In this study, RA, in a calcified bifurcation lesion, could be used in any segments, single or combined, of the bifurcation. The technical parameters of rotablation were accurately recorded. Patients were treated exclusively with drug-eluting stents (DES) in 98.2% of cases.
OUTCOMES
The primary endpoint was defined as a composite of the cumulative incidence of cardiovascular death, myocardial infarction (MI), TLR, stroke and coronary artery bypass grafting (CABG) up to one year following the procedure.
The secondary endpoints were the clinical success rate of the RA procedure (defined as a successful revascularisation of all treated lesions [residual stenosis <50%] and no periprocedural complications) and the incidence of in-hospital complications including coronary perforation, coronary dissection, coronary low flow or no flow, emergency CABG, tamponade, MI, stroke or transient ischaemic attack (TIA), bleeding events (according to the Bleeding Academic Research Consortium [BARC] classification10) and death.
Detailed definitions of these endpoints are presented in Supplementary Appendix 1.
STATISTICAL ANALYSIS
Statistical analysis was performed using Stata statistical software, release 14.1 (StataCorp, College Station, TX, USA). Continuous variables were summarised as means and standard deviations for normal distribution, and as medians and interquartile ranges when not normally distributed. Categorical variables are presented as proportions. In order to identify factors associated with the occurrence of the primary and secondary endpoints, differences between groups were tested using the chi-square test for qualitative data and means comparisons for continuous data. Non-parametric tests were used when necessary. Multivariate analyses were performed using logistic regression and the Cox model.
Results
Between October 2016 and July 2018, 1,016 consecutive patients were included in the study. The distribution of patients according to their country of inclusion is shown in Supplementary Table 1. Fifty patients were excluded because of missing data; thus, 966 patients were included in the final analysis. The follow-up was complete for 950 patients (98.3%) and 891 patients (92.2%) at 30 days and one year, respectively.
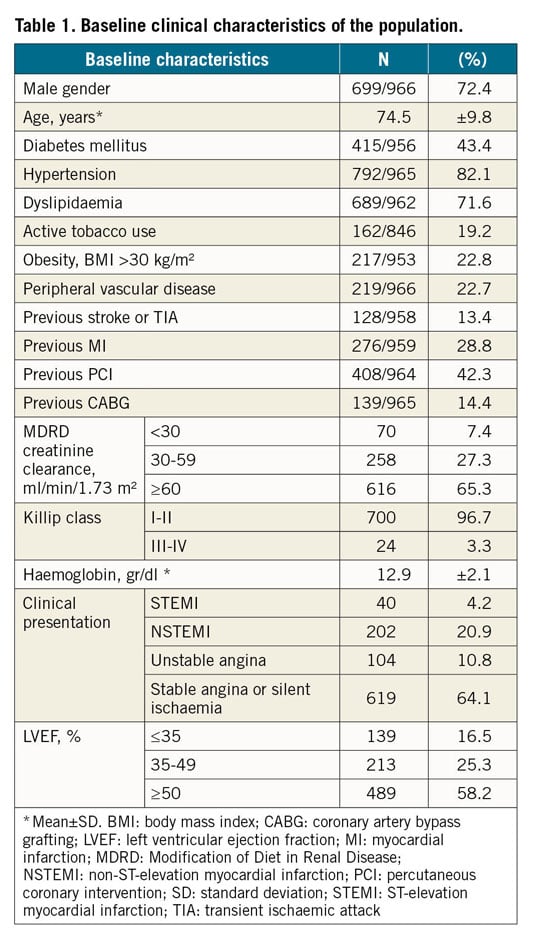
BASELINE PATIENT CHARACTERISTICS
Mean age was 74.5 years and 72.4% were male. The presentation was stable for 64.1% of the patients, 4.2% presented with ST-elevation myocardial infarction (STEMI), 20.9% with non-ST-elevation myocardial infarction (NSTEMI) and 10.8% with unstable angina. Baseline clinical features are summarised in Table 1.
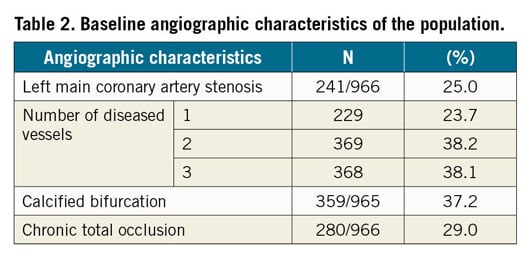
BASELINE ANGIOGRAPHIC CHARACTERISTICS
Two hundred and forty-one patients (25%) presented with a significant lesion (i.e., ≥50%) on the left main coronary artery (LMCA), 368 (38.1%) had three-vessel disease, and 280 (29%) had a chronic total occlusion of an epicardial coronary trunk (treated or not with RA). Baseline angiographic characteristics are described in Table 2.
ROTATIONAL ATHERECTOMY PROCEDURE
The vascular approach was radial for 71.8% of procedures, and the sheath size <7 Fr in 75.1% of cases. Only one lesion was treated with RA in 725 patients (75%). When several lesions were treated with RA, one single procedure was sufficient in 86% of cases. Regarding the rotablation itself, the maximal burr size was 1.5 mm in 51.7% of cases and the maximal burr speed was set between 160,000 and 180,000 rpm in 55.9% of procedures. Intracoronary imaging guidance by intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was used in only 6.9% of procedures. RA procedure characteristics are detailed in Supplementary Table 2. Procedural characteristics according to the country of inclusion (for countries which included a minimum of 30 RA procedures) are summarised in Figure 1.
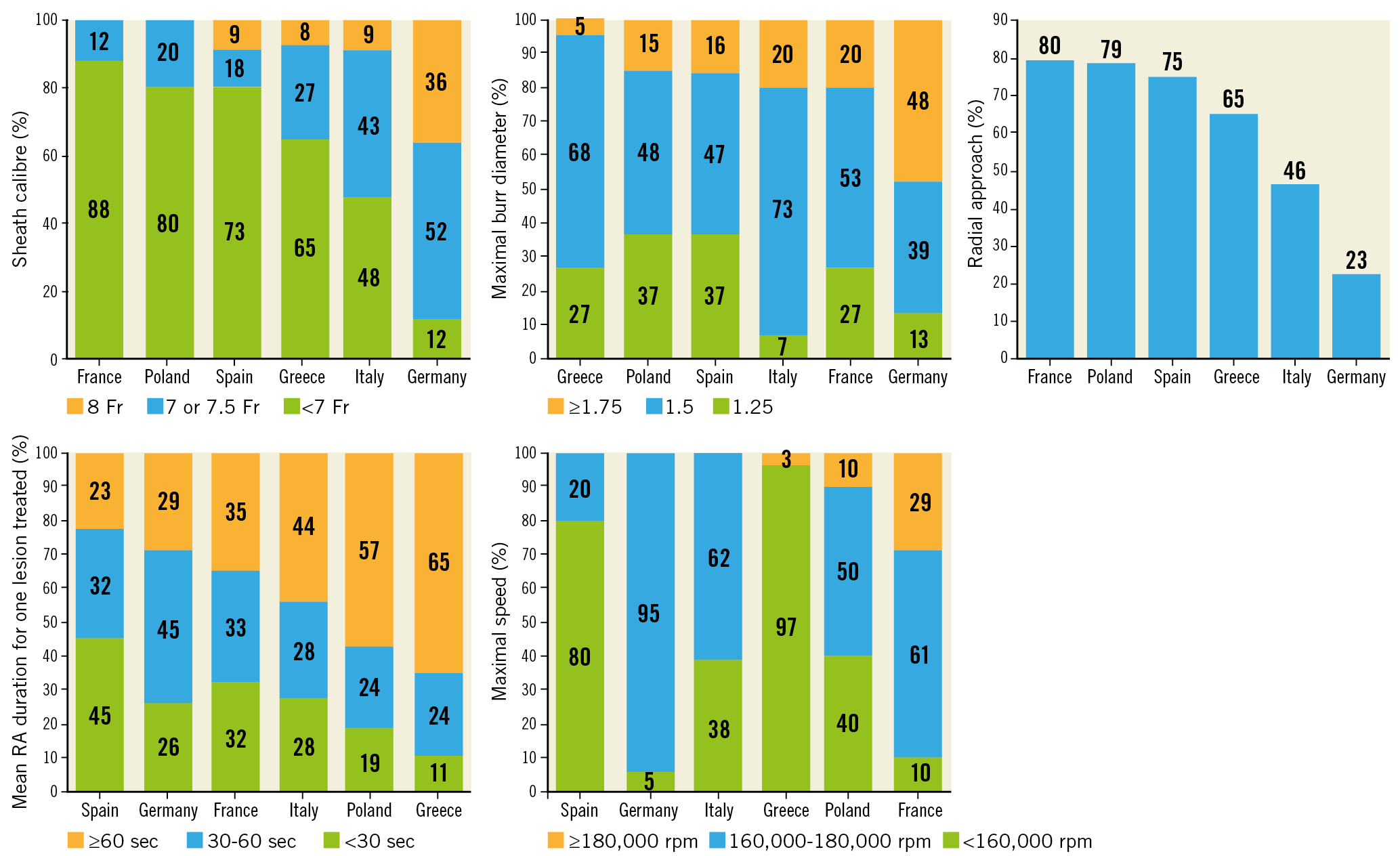
Figure 1. Technical characteristics of the RA procedure according to the country of inclusion.
IN-HOSPITAL OUTCOMES
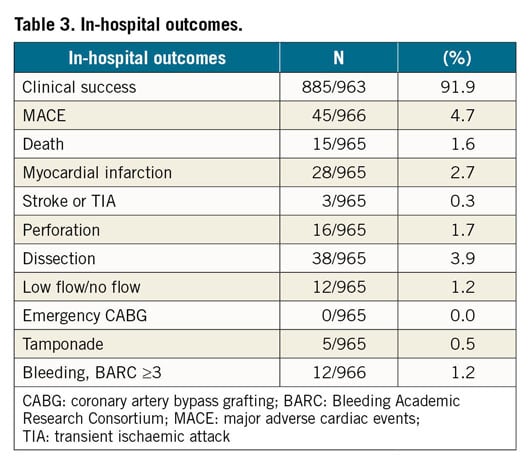
The rate of clinical success, defined as an angiographic success and no post-procedure complications within 24 hours, was 91.9%. In-hospital major adverse cardiac events (MACE) occurred in 45 patients (4.7%). Rates of death and post-procedure MI were 1.6% and 2.9%, respectively. Coronary perforation occurred in 16 patients (1.7% of cases), leading to a cardiac tamponade in five patients (0.5%). No cases of emergency CABG were recorded.
Severe bleeding (BARC ≥3) occurred in 12 patients during hospitalisation. No differences were observed between radial and femoral access (7 patients [1%] in the radial group vs 5 patients [1.8%] in the femoral group, p=0.33). Among patients treated by femoral approach who presented a bleeding, no differences were found according to the size of the sheath (2 subjects [1.6%] in the <7 Fr group vs 3 subjects [2.1%] in the ≥7 Fr group, p=1.00). In-hospital outcomes are summarised in Table 3.
MEDICAL THERAPY AT DISCHARGE
Nine hundred and three patients (96.6%) had dual antiplatelet therapy (DAPT) at discharge and 188 (20.1%) had an oral anticoagulant therapy. Beta-blockers and statin therapy were prescribed to 81.7% and 88.5% of patients, respectively. The medical treatment prescribed at discharge is detailed in Supplementary Table 3.
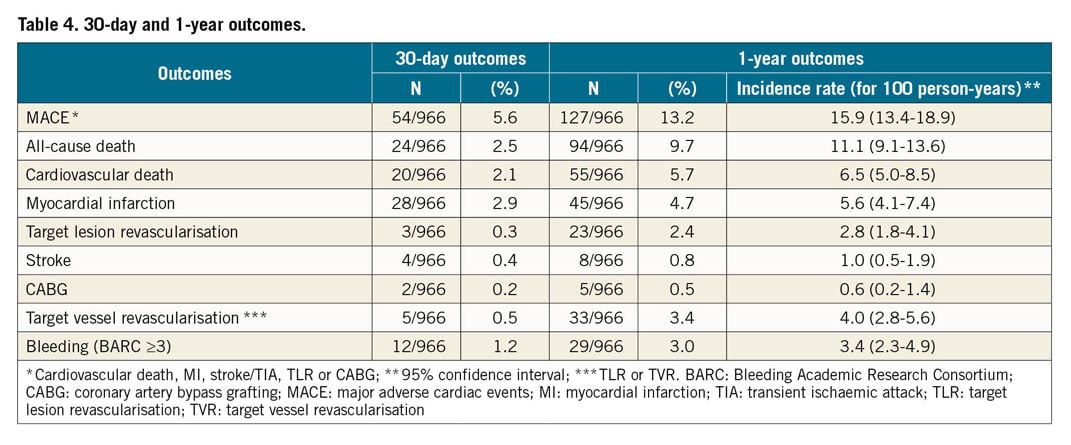
FOLLOW-UP OUTCOMES
The rate of MACE (defined as cardiovascular death, MI, stroke or TIA, TLR or CABG) was 5.6% and 13.2% at 30 days and one year, respectively. The rate of all-cause death was 2.5% at 30 days (2.1% for cardiovascular death) and 9.7% at one year (5.7% for cardiovascular death). The 30-day and one-year outcomes are detailed in Table 4.
PREDICTORS OF MACE
Multivariate analysis identified Killip class III/IV (odds ratio [OR] 4.86, confidence interval [CI]: 1.47-16.10; p=0.010) and LMCA stenosis (OR 2.66, CI: 1.38-5.12; p=0.003) as predictors of in-hospital MACE, whereas past medical history of CAGB remained associated with a “protective” effect (OR 0.21, CI: 0.05-0.91; p=0.037) (Supplementary Table 4).
At 30 days, the multivariate analysis identified Killip class III/IV (OR 2.99, CI: 1.05-8.56; p=0.041), acute coronary syndrome (ACS) (OR 2.12, CI: 1.20-3.75; p=0.010) and a number of burr runs ≥3 (OR 4.27, CI: 1.03-17.70; p=0.046) as predictors of 30-day MACE (Supplementary Table 5).
At one-year follow-up, the factors independently associated with the occurrence of MACE at one-year follow-up were female gender (OR 1.70, CI: 1.18-2.47; p=0.005), glomerular filtration rate (GFR) <30 ml/min/1.73 m² (OR 1.77, CI: 1.01-3.12; p=0.048), ACS at admission (OR 1.59, CI: 1.09-2.31; p=0.016), depressed left ventricular ejection fraction (LVEF) <35% (OR 1.61, CI: 1.02-2.55; p=0.040), and LMCA stenosis (OR 1.62, CI: 1.12-2.35; p=0.011) (Figure 2, Supplementary Table 6).
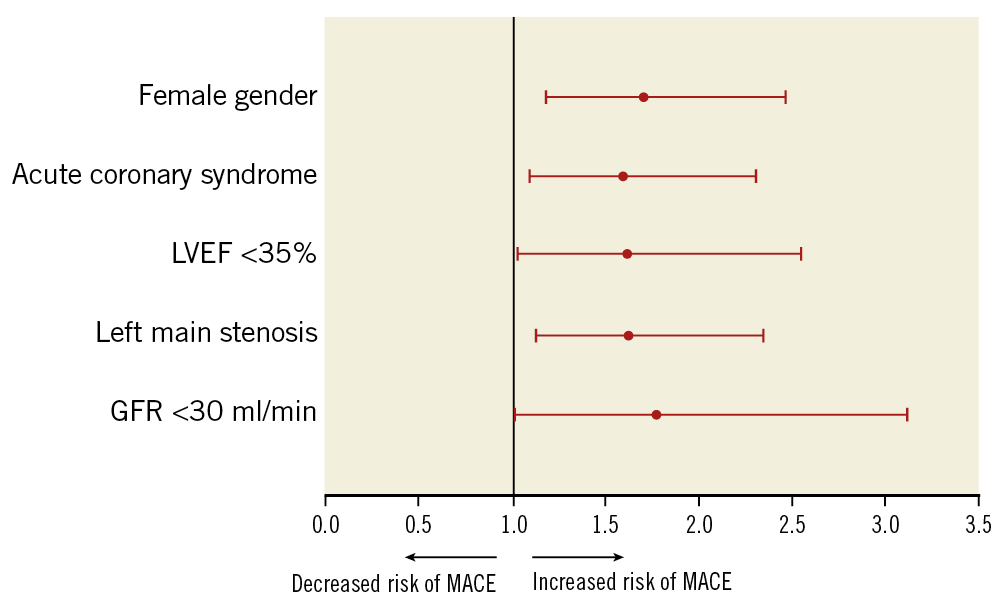
Figure 2. Independent predictors for midterm major adverse cardiovascular events.
Discussion
The Euro4C registry is the first international multicentric prospective registry investigating prognostic factors of clinical outcomes in PCI with RA. The main findings of this observational study are the following.
1. The rate of clinical success of RA was high and the rate of in-hospital complications was low, with a rate for in-hospital MACE of 4.9%.
2. The one-year rate of MACE was 13.2%, probably reflecting the high-risk level of patients rather than the consequences of the RA procedure itself.
3. The factors independently related to the occurrence of one-year MACE are common clinical factors in coronary artery disease (CAD), e.g., renal failure, ACS at admission, low LVEF, and LMCA stenosis. Interestingly, female gender was also independently associated with worse midterm outcomes.
This registry allows the assessment of the current practice and use of RA in experienced European centres. It is noteworthy that the radial approach was chosen in 71.8% of cases. This preferential vascular approach is in line with the highest standards of care and is in contrast with the largest available registry conducted on RA to date, the retrospective ROTATE registry, performed between 2002 and 2013, in which the femoral approach was used in 71.6% of cases11. The high rate of radial approach in our study allowed a wide use of 6 Fr guiding catheters (75.1% of procedures with sheaths ≤6 Fr), with burrs of up to 1.75 mm used in nearly 80% of the procedures reported. This preferential utilisation of small burrs is in line with the concept of plaque modification described previously. Although the access site was not independently related to short and midterm MACE in our cohort, it is well known that the radial approach allows a reduction of access site-related complications in PCI12,13.
The low flow and no flow rate was relatively low in our cohort (1.2%). As centres participating in the study are very familiar with RA, this probably reflects that the procedures were carried out in accordance with a recent expert consensus document6 which recommends using small burrs, short runs of ablation, speed of rotation below 180,000 rpm, pecking motion of the burr against the plaque, and liberal use of intracoronary nitrates between runs.
A certain degree of disparity among countries regarding the technical approach of RA was observed, although these disparities were not independently related to midterm outcomes. Similarly, such technical parameters were not identified as independent predictors of MACE in previous studies11,14. However, it is noteworthy in the present study that a number of runs >3 was independently associated with the occurrence of MACE at 30 days (hazard ratio [HR] 4.27, p=0.046), and a trend was noticeable for in-hospital MACE.
This finding might be explained by the presence of more severe or widened calcifications – requiring a higher number of runs to obtain a satisfactory debulking – responsible for a higher MACE rate.
The one-year MACE rate observed in this registry was 13.2%, mainly related to cardiovascular death (5.7%) and MI (4.7%). In a recent meta-analysis that pooled 18,441 subjects included in 18 trials treated by PCI with DES, Kedhi et al reported a one-year MACE rate of 9.4% and 13.9% for patients without and with diabetes, respectively15. Thus, the outcomes of this study appear acceptable when considering the high anatomical and clinical complexity of the recruited patients. Moreover, these outcomes are concordant with previous registries focusing on RA. In the Melbourne Interventional Group registry16, the ROTATE registry11, and in the Mount Sinai Hospital cohort17, the one-year MACE rates were 15.6%, 16%, and 21.6%, respectively. The improvement observed in our study could, at least partially, be the result of a greater use of second-generation DES (98.2% vs 69.3% in ROTATE). In the ROTATE study, the MACE rate at one year was mainly driven by TLR (11.3%), whereas this rate was much lower in our cohort (2.4%), which appears to be a good result for such complex lesions.
Interestingly, in our study, female gender was independently associated with the occurrence of one-year MACE. To date, only one study has addressed the question of gender difference in outcomes following RA18. In this Scottish retrospective monocentric cohort that included 765 subjects treated with RA, the authors reported a similar incidence of MACE between female and male patients at 4.5-year follow-up, but a higher rate of procedural and in-hospital complications among females. In our cohort, we observed the same phenomenon in disfavour of female patients regarding in-hospital MACE (OR 1.87 [1.01-3.47]; p=0.047). Just as in this recent report, we observed a tendency, although non-significant, towards a higher number of perforation and dissection events in female patients (data not shown). These events explain the differences observed between male and female subjects in procedural outcomes, and are probably, at least partially, due to smaller-sized and more fragile arteries in women.
ACS as the initial presentation is, in the present study, related to the occurrence of one-year MACE. This result was expected, as ACS is known to have a worse prognosis than stable presentation of coronary disease, with, in particular, a high rate of events in the year following the ACS19,20. Previous studies have assessed the use of RA in the context of ACS21,22. They demonstrated that RA is feasible in this setting with safety outcomes similar to those in the context of stable CAD, but worse outcomes at midterm follow-up. Renal failure was also identified as an independent predictor of one-year MACE in our registry. This finding is consistent with the literature, as kidney disease is known to be a strong prognostic factor in CAD in general23,24, and in particular in patients treated by RA11,14. Unsurprisingly, depressed LVEF and LMCA stenosis (treated with RA or not) were independently associated with the occurrence of MACE at one year. The prognostic importance of these simple parameters in CAD was first described four decades ago in the CASS registry25 and has been confirmed since then, despite the critical advances achieved in the management of this pathology.
Limitations
The main limitation of this study is its observational design. The decision to use RA was left to the discretion of each centre and no central core lab analysed the procedures for endpoint definition. Thus, no preprocedural or post-procedural systematic quantitative coronary angiography (QCA) analysis was performed. Data regarding the global complexity of the coronary anatomy and on the level of risk of the patients in our population were not available.
Conclusions
Our study, focused on the contemporary approach of rotational atherectomy, demonstrates that this technique is safe and efficient, with low procedural and hospital complications and a high clinical success rate. During follow-up, we observed a low one-year TLR rate, and the rate of one-year MACE appeared very acceptable in this high-risk population. The prognosis of these patients is driven by the usual clinical and paraclinical parameters in CAD.
|
Impact on daily practice Our data demonstrate that the RA procedure has a good clinical success rate and a low in-hospital complication rate in experienced centres. Multivariate analysis identified female gender, poor renal function, low left ventricular ejection fraction, ACS (with or without ST-elevation at admission) and the presence of unprotected left main stenosis as independent predictors of one-year MACE. |
Acknowledgements
The authors acknowledge all the physicians and their teams in the participating centres across Europe (Supplementary Table 1).
Funding
The study was conducted with the financial support of Boston Scientific.
Conflict of interest statement
F. Bouisset reports grants from Boston Scientific, during the conduct of the study, and personal fees from MSD, Abbott, Bayer, and Amgen, outside the submitted work. E. Barbato reports personal fees from Abbott Vascular and Boston Scientific, outside the submitted work. K. Reczuch reports personal fees from Boston Scientific, outside the submitted work. G. Cayla reports research grants and/or personal fees from Amgen, AstraZeneca, Abbott, Bayer, Boston Scientific, Biotronik, Bristol-Myers Squibb, Pfizer, and Sanofi-Aventis, outside the submitted work. T. Lhermusier reports personal fees and non-financial support from Boston Scientific, outside the submitted work. J. Palazuelos Molinero reports personal fees from Abbott, Boston Scientific, Biotronik, IHT, Bayer, Medtronic, Daichii Sankyo, and Novartis, outside the submitted work. M. Ferenc reports personal fees from Boston Scientific, Medtronic, Terumo, Teleflex, Biotronik, and OrbusNeich, outside the submitted work. D. Carrié reports grants from Boston Scientific during the conduct of the study, and personal fees from Alvimedica, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.