Abstract
Aims: The aim of this study was to determine the feasibility of rotational atherectomy (RA) in chronic total occlusion (CTO) PCI and compare the success and complication rates of RA in CTO lesions versus non-occluded lesions. Data on RA in CTO are rare and it is unknown how procedural success and risk of RA in CTO lesions compare to RA in non-CTO lesions.
Methods and results: RA was performed in 392 out of 17,919 PCI procedures (2.2% of the PCI cohort) and classified as RA CTO (n=75) and RA non-CTO (n=317). Procedural success and MACCE in both groups were assessed by two investigators. All RA procedures were analysed for dissections prior to RA, which were defined according to the NHLBI classification. Baseline characteristics were not significantly different in the two groups but, in RA CTO, lesion type was more complex (p<0.001), stented segments were longer (35.0±22.7 vs. 46.0±24.8 mm, p<0.001) and mean burr size was smaller (1.61±0.17 vs. 1.49±0.18 mm, p<0.001). Procedural success and complications were not different (RA non-CTO 96.2% and RA CTO 94.7%, RA non-CTO 2.5% and RA CTO 4.0%, respectively). RA performed in dissection planes had a 100% procedure success rate in CTO and a 92% success rate in non-CTO.
Conclusions: RA in CTO is as safe and as effective as RA in non-CTO. The presence of dissections prior to RA in CTO lesions as well as in non-CTO lesions does not seem to have a negative impact on outcome.
Abbreviations
CTO: chronic total occlusion
MACCE: major adverse cardiovascular and cerebral events
NHLBI: National Heart, Lung, and Blood Institute
OTW balloon: over-the-wire balloon
PCI: percutaneous coronary intervention
RA: rotational atherectomy
RA CTO: rotational atherectomy in a CTO lesion
RA non-CTO: rotational atherectomy in a non-occluded lesion
TIMI: Thrombolysis In Myocardial Infarction
TVR: target vessel revascularisation
Introduction
Operators are dealing with an increasing number of elderly patients presenting with complex, often calcified coronary artery lesions including chronic total occlusions (CTO)1. The amount of CTO burden in the future is expected to grow due to an ageing population suffering from diabetes mellitus and renal failure and an increasing number of post-coronary artery bypass graft (CABG) patients who show significantly more CTOs after graft failures2. The operators’ strategy in clinical practice must adapt to these new challenges. Due to improvement of CTO equipment, wiring occlusive lesions often works, but balloon crossing or balloon expansion fails3,4. Rotational atherectomy (RA) is a valuable and resurgent technique to overcome this frustrating situation.
However, the outcome of CTO rotablation has not been sufficiently investigated and it is unknown how the risk and procedural success of RA in CTO lesions compare to RA in non-CTO lesions. Thus, the objective of the present study was to evaluate the feasibility of CTO rotablation and to compare success and complication rates of RA in CTO versus non-CTO PCI.
Methods
PATIENT POPULATION
In this single-centre retrospective study, 17,919 consecutive PCIs in 11,393 patients from February 2004 to October 2017 were screened. PCIs were performed in 14,947 non-occlusive and in 2,972 (17%) occlusive lesions. In 317 non-occlusive lesions (2.1% of total non-occlusive cohort) and in 75 occlusive lesions (2.5% of total occlusive cohort), rotational atherectomy (RA) was performed prior to stent implantation because of severely calcified stenoses that were not balloon crossable or dilatable, despite prior application of basic interventional techniques such as buddy wire, wire cutting or other support strategies for increased back-up.
ROTATIONAL ATHERECTOMY
The indication for RA was balloon failure, which was defined as failure to cross or dilate a lesion. Wire exchange was performed by using a microcatheter or low-profile over-the-wire (OTW) balloon catheter, which either crossed the lesion or was advanced as far as possible into the lesion. A procedure was regarded as an RA procedure as soon as a RotaWire (Boston Scientific, Marlborough, MA, USA) was advanced through the target lesion. RA was performed with the Rotablator® system (Boston Scientific) according to standard protocol as previously described5. Burr size was chosen up to 0.7 vessel ratio for non-CTO and up to 0.5 vessel ratio for CTO lesions, following the recommendation of the European expert consensus on rotational atherectomy5 to use smaller burr sizes in CTO lesions.
DEFINITIONS
CTO was defined as a coronary occlusion with Thrombolysis In Myocardial Infarction (TIMI) 0 flow for ≥3 months. In accordance with the CTO consensus document, the duration of CTO was either certain (angiographically confirmed) or likely (clinically confirmed)6. The type of target lesion was defined according to the ACC/AHA classification. For CTO lesions the J-CTO score was applied7. One point was assigned to each of the following variables: previously failed attempt, blunt stump, calcification, bending >45°, occlusion length ≥20 mm. Lesion calcification was assessed angiographically.
Technical success was defined as RA followed by stent implantation with residual stenosis <30% and TIMI 3 flow in the target vessel. Procedural success was defined as technical success without severe in-hospital complications.
Severe complications were defined as death, emergency surgery, vessel perforation, cardiac tamponade requiring intervention, in-hospital myocardial infarction (type IV, according to the ESC guidelines)8, in-hospital stroke, cardiac decompensation, and acute target vessel reintervention. Technical and procedural success as well as in-hospital complications were examined by two investigators. Angiograms were examined by two investigators for the presence of dissections in the target segment prior to RA. Dissections were defined according to the NHLBI classification9.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±SD and categorical variables as frequencies and percentages for each group. For comparison of continuous variables, the Student’s t-test was used. Chi-square and Fisher’s exact tests were used to compare differences between proportions. Statistical analysis was performed using SPSS v.16 software (SPSS Inc., Chicago, IL, USA).
Results
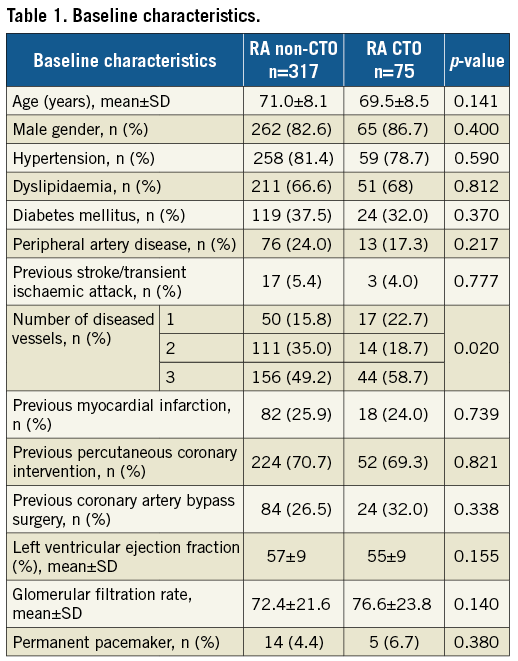
BASELINE CHARACTERISTICS
The study population comprised 317 RA procedures in non-CTO lesions (RA non-CTO, 81%) and 75 RA procedures in CTO lesions (RA CTO, 19%). Baseline characteristics are listed in Table 1. There were no significant differences between the two groups.
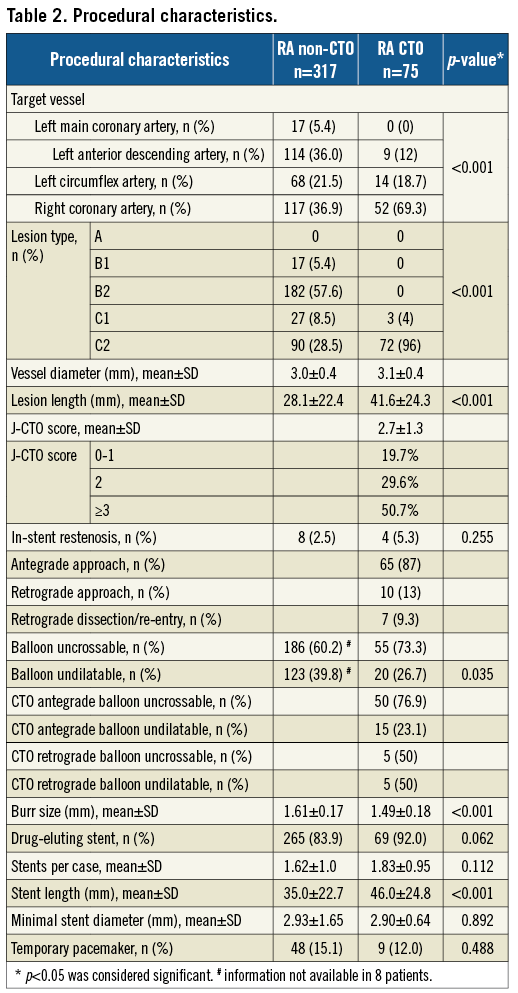
PROCEDURAL CHARACTERISTICS
RA was performed in non-CTO lesions, because the lesion was balloon uncrossable in 60.2% and balloon undilatable in 39.8% of the procedures. In CTO lesions the lesion was balloon uncrossable in 73.3% and undilatable in 26.7% (Table 2). Regarding the procedural characteristics, in RA CTO patients the lesion type was significantly more complex (p<0.001), the lesion as well as the stented segment was longer (28.1±22.4 vs. 41.6±24.3 mm and 35.0±22.7 vs. 46.0±24.8 mm, respectively, p<0.001), the burr size was smaller (1.61±0.17 vs. 1.49±0.18 mm, p<0.001) and the target vessel more often the right coronary artery (36.9% vs. 69.3%, p<0.001). The mean J-CTO score was 2.7±1.3 (score 0-1 in 19.7%, 2 in 29.6%, ≥3 in 50.7%). The target vessel diameter and the minimal stent diameter were similar in both groups (3.0±0.4 vs. 3.1±0.4 mm and 2.93±1.65 vs. 2.90±0.64 mm, respectively). Temporary pacemakers were used in 15.1% in non-CTO vs. 12.0% in CTO lesions (n.s.), while a permanent pacemaker was found in 4.4% vs. 6.7% of the patients, respectively.
IN-HOSPITAL OUTCOME
In every case the RotaWire was able to pass the target lesion. Procedure success was achieved overall in 376 out of 392 cases (95.9%), in RA non-CTO in 305 out of 317 (96.2%) and in RA CTO in 71 out of 75 (94.7%). Technical success was achieved in 379 out of 392 procedures (96.7%), in RA non-CTO in 308 out of 317 (97.2%) and in RA CTO in 71 out of 75 procedures (94.7%) (Table 3).
Procedure failure was noted in 16 cases (4.1%), 12 in RA non-CTO (3.8%) and four in RA CTO (5.3%). Procedural failure in non-CTO comprised eight complications. In addition, four patients had reduced flow at the end of the procedure (Table 3).
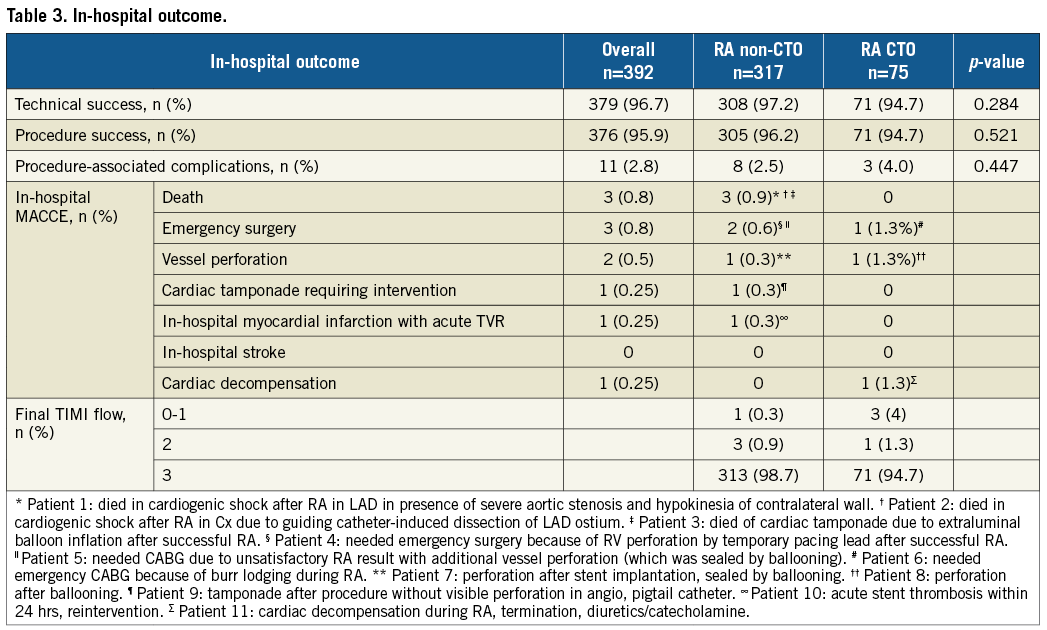
Procedural failures in RA CTO comprised three complications, and one patient had slow flow at the end of the procedure; flow normalised at follow-up.
Severe complications occurred in 11 out of 392 procedures (2.8%). Three patients died (0.8%). One patient died in cardiogenic shock after RA in the LAD in the presence of severe aortic stenosis and contralateral hypokinesia (RA-related); emergency valvuloplasty could not save him. One patient died in cardiogenic shock after RA in the CX due to guiding catheter-induced dissection of the LAD ostium (not RA-related). One patient died after an extraluminal balloon inflation in a non-RA vessel after successful RA in a different vessel with resulting tamponade (not RA-related).
Three patients underwent emergency surgery (0.8%). One patient suffered from an RV perforation with cardiac tamponade caused by a temporary pacing lead after successful RA (RA-related). One patient needed CABG due to an unsatisfactory RA result with additional vessel perforation (which could be sealed by ballooning, RA-related). One patient needed CABG because of a burr entrapment (RA-related).
Two patients showed vessel perforations (0.5%). One patient had a perforation after stent implantation in a non-RA segment that could be sealed by ballooning (not RA-related). One patient had a perforation after ballooning with myocardial contrast staining and did not require further treatment (RA-related).
One patient suffered from a cardiac tamponade (0.25%) hours after a successful procedure that could be treated interventionally (pigtail); a perforation could not be identified angiographically (not RA-related).
One patient had an in-hospital myocardial infarction due to an acute stent thrombosis (0.25%) in the target lesion within 24 hours after a successful procedure (not RA-related).
One patient went into cardiac decompensation (0.25%) during RA with termination of the procedure (treatment with diuretics and catecholamine, RA-related).
COMPLICATIONS IN RA NON-CTO VERSUS RA CTO (Table 3)
Eight complications occurred in RA non-CTO (2.5%), and three complications in RA CTO (4.0%). All deaths were found in RA non-CTO (0.9%). Further complications in RA non-CTO were emergency surgery (0.6%), vessel perforation (0.3%), cardiac tamponade (0.3%), and in-hospital myocardial infarction with target vessel reintervention (0.3%).
Complications in RA CTO were burr entrapment (1.3%), vessel perforation (1.3%) and cardiac decompensation (1.3%). In-hospital stroke did not occur in any procedure.
PRESENCE AND ABSENCE OF DISSECTIONS PRIOR TO RA IN NON-CTO AND CTO LESIONS
Dissections prior to RA were found in 25 of 309 non-CTO procedures (8%) (Table 4), in 19 procedures (76%) after predilation and in six procedures were wire-induced. Angiograms were not available in eight procedures. We saw 4 Type A, 4 Type B, 14 Type C, 2 Type D, and 1 Type F dissections. Procedure success in patients with RA in non-CTO lesions with dissection was achieved in 23 of 25 cases (92%); a complication occurred in one patient (patient no. 5 in the footnotes of Table 3). Dissections prior to RA were found in 15 of 74 (20%) CTO procedures (Table 4), in 10 procedures (66.7%) after predilation and in 5 procedures were wire-induced. We saw 7 Type B, 6 Type C and 1 Type F dissections. Overall dissections prior to RA were found more often in the CTO group (p=0.002); an example is shown in Figure 1. Information about possible dissection was missing in one patient. Procedure success in patients with RA in CTO lesions with dissection was achieved in 15 of 15 cases (100%); no complications occurred.
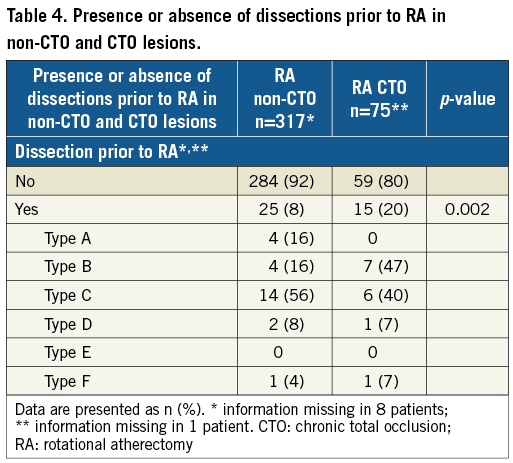
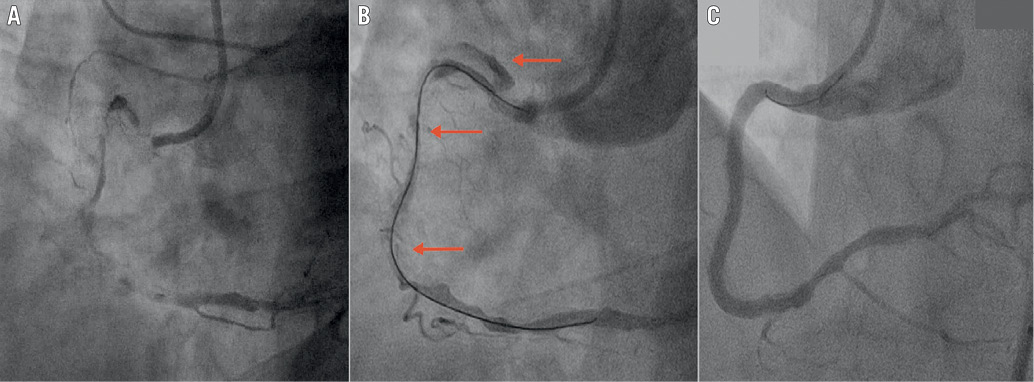
Figure 1. RA CTO in dissection plane. A) RCA CTO at baseline. B) RCA CTO after successful antegrade wire crossing with type C dissection (red arrows) before RA. C) Final result after RA and stent implantation. RCA: right coronary artery
Discussion
The main findings of the present study are:
1) There were no significant differences in technical and procedural success of RA in non-occluded coronary artery lesions compared to RA in CTO.
2) The composite of in-hospital complications was low in RA in CTO lesions and comparable to RA in non-occluded lesions.
3) Dissections occurred significantly more often in CTO lesions.
4) RA in the presence of a dissection was not associated with a higher risk.
Most data available on RA focus on its application in non-occlusive coronary artery disease with a procedure success rate of 93-98% and a procedure MACE rate of 4-6%10. Compared to non-occlusive coronary artery lesions, CTOs have different characteristics.
With increasing CTO age, the intimal plaque transforms from a cholesterol and foam cell-laden to a fibro-calcified plaque with neovascular channels arising from the adventitial space11. Due to the improvement of recanalisation technology in CTO PCI, wire crossing is increasingly facilitated but balloon crossing or dilation often fails. Alongside different techniques and devices (cutting balloon, Tornus [Asahi Intecc, Aichi, Japan], etc.), RA is an attractive technique to open these lesions5, but data on RA in CTO lesions are rare.
Information on feasibility and outcome in this setting is based only on small patient numbers from registries and case reports3,4,12-14.
The procedure success rate for RA in CTO varies in the published literature from 77% in a cohort of 35 patients12, 95.6% in a cohort of 45 patients4 to 96.2% in a cohort of 26 patients13. How this procedure success compares to the success rate of RA in non-occluded lesions is unknown, as previous studies have only compared success rates between rotablated versus non-rotablated CTOs. This is not a fair comparison, because these patient cohorts differ from each other. Patients who need RA for CTO are older, have more calcified and longer lesions and more comorbidities3.
To the best of our knowledge, the present study is the first to compare the success and complication rates of RA in CTO lesions to RA in non-CTO lesions and comprises the highest number of patients who underwent RA in CTO procedures so far.
Patient demographics in the two groups were comparable. In our patient cohorts the technical and procedural success was between 95% and 97%. Despite a longer stented segment and a smaller burr size in RA CTO, we would like to emphasise that there was no difference in the success rate in RA CTO vs. RA non-CTO. The high success rate in our study may be explained by our strategy of using RA as a first-line approach after balloon failure instead of making prior attempts with other devices such as a cutting balloon or Tornus, as preferred by other operators3,12. Only this standardisation of protocol allows a valid comparison of the success and complication rates of both groups.
There are comprehensible concerns about using RA in a CTO setting, as the complication rate is expected to be high in the presence of ostensible contraindications or potential risk factors - dissections (balloon- or wire-induced), risk of extraluminal wire position, small distal vessels, invisible side branches or risk of burr entrapment due to long and heavily calcified lesions.
Despite these unfavourable factors in CTO PCI, we did not find a difference in procedure-related complications (RA non-CTO 2.5% vs. RA CTO 4.0%, p=0.447) in our study.
In our cohort, three out of 75 RA CTO patients had complications. One patient showed burr entrapment in a tortuous, heavily calcified circumflex lesion. This complication is rare but known15 and eventually might be observed more frequently in CTOs due to their complex pathology. Another patient suffered from cardiac decompensation during RA in the presence of impaired LV function. The third patient had a balloon-induced vessel perforation, which could be sealed by prolonged balloon inflation. The other eight complications, including three deaths, occurred in the non-CTO group.
In other studies, dissections after RA were seen in up to 29% of patients12 and perforations in up to 13%3. These differences from our results may be a consequence of the mentioned strategy to use the Rotablator as a first-line device. However, in our opinion the more urgent question is whether the existence of dissection planes prior to RA increases the risk of the procedure.
Dissections owing to guidewire advancement are common in CTO PCI and their occurrence is even more frequent than in non-CTO PCI16. Moreover, they are an accepted or even deliberately produced component of several recanalisation techniques that have improved the success rate, such as the parallel wire technique, see-saw technique or subintimal wire tracking17.
Discouragingly, the European expert consensus on RA advises against performing RA in such situations because of the increased risk of perforation or fear of extending the dissection further distally5.
In order to investigate whether the presence of dissection translates to a worse outcome in RA, in the present study an analysis of all angiograms was performed by two investigators to identify and classify vessel dissections prior to RA. Dissections were significantly more often found in CTO lesions compared to non-CTO lesions before RA was performed (20% vs. 8%, p=0.002). All RA CTO procedures were successful without adverse events. In RA non-CTO, only one patient had a vessel perforation which was sealed after prolonged balloon inflation (patient no. 5 in the footnotes of Table 3). All other complications occurred in procedures with non-dissected vessels, so this gives a strong hint that RA in dissection planes is not necessarily riskier than in non-dissections. Concordant results were found in a multicentre registry from Azzalini et al12, where RA was performed safely in seven patients with dissected vessels. We consider these congruent observations to be of special relevance regarding the circumstance in which dissections are a fact to be dealt with, especially in CTO PCI, and that the positive results of RA in dissection planes without adverse events contradict the recommendation of the European expert consensus5. Despite the fact that RA procedures were performed successfully in challenging cases with wire position in the subintimal space14, we would strongly recommend rotablation in the presence of dissections only when the RA wire position is confirmed in the distal vessel lumen.
Limitations
This was a single-centre, retrospective study registry with its inherit limitations, with no core lab evaluation. Lesion calcification was assessed only angiographically (without intravascular imaging). However, the indication for RA was not based on the degree of calcification but on the uncrossability or undilatability of a lesion. In addition, no long-term data are presented, which could provide information on the outcome of patients with versus those without dissections in CTO and non-CTO RA.
Conclusions
RA in CTO is as safe and as effective as in non-occluded vessels, despite longer and more complex lesions. The presence of dissections prior to RA in CTO lesions as well as in non-CTO lesions does not seem to have a negative impact on outcome.
| Impact on daily practice Our results may encourage operators to include RA more frequently in their approach to CTO PCI. |
Acknowledgements
The authors gratefully acknowledge Robert Scharp and Laura Schröder for their assistance in data collection.
Conflict of interest statement
The authors have no conflicts of interest to declare.