Abstract
Aims: Unprotected left main (ULM) coronary artery disease is encountered in 3%-10% of coronary angiograms and is associated with high mortality. The survival of patients with ULM disease presenting with acute coronary syndromes (ACS) depends on different variables and is lowest in those with cardiogenic shock (CS). The aim of the present study was to estimate the impact of baseline characteristics on the subsequent clinical outcome in patients treated by percutaneous coronary intervention (PCI) of ULM for ACS.
Methods and results: One hundred and thirty-four patients were retrieved from our database and followed by phone or physician visit. Patients were classified into two groups according to their presentation (CS/STEMI group: patients presenting with CS or ST-elevation myocardial infarction; NSTEMI/UA group: patients with non-STEMI or unstable angina). Data collected were baseline characteristics, procedural information, and clinical outcome. The primary endpoint was all-cause mortality at 6-month follow-up. The secondary end point was a composite of cardiac death, myocardial infarction, and any repeat revascularisation, i.e., major adverse cardiac events (MACE). Kaplan-Meier curves were computed for survival. Logistic regression determined that hypercholesterolaemia (OR 6.22, p=0.03), high pre-procedural TIMI score (OR 3.89, p=0.01), preserved left ventricular ejection fraction (OR 1.07, p=0.01) and LM as culprit lesion (OR 8.57, p=0.01) protected against development of CS. Primary outcome occurred in 44% of patients in the CS/STEMI group compared to 6% in the NSTEMI/UA group (p<0.001). MACE were observed in 30 patients (48%) of the CS/STEMI group and in 12 patients (19%) of the NSTEMI/UA group (p=0.001).
Conclusions: Acute coronary syndrome due to critical ULM stenosis is associated with high mortality even after successful PCI. Patients presenting with CS or STEMI are at particular risk.
Abbreviations
CABG coronary artery bypass grafting
MACE major adverse cardiac events
MI myocardial infarction
PCI percutaneous coronary intervention
TVR target vessel revascularisation
ULM unprotected left main coronary artery
URL upper reference limit
Introduction
Critical unprotected left main (ULM) coronary artery disease is a dreaded condition as it puts nearly the entire myocardium at risk, and is associated with high morbidity and mortality1. Significant ULM disease is encountered in 3%-10% of patients undergoing coronary angiography2-4. Although percutaneous coronary intervention (PCI) has long surpassed coronary artery bypass grafting (CABG) as the most common revascularisation strategy in patients with coronary artery disease, ULM is still considered as a relative contra-indication to PCI and CABG remains the single class I recommendation by official European and American guidelines5-7. Major advances have been made in PCI in the past decade, including the nearly systematic use of drug-eluting coronary stents (DES) and the development of more effective antithrombotic regimens, stimulating a renewed interest in PCI of ULM. Consistently, new evidence demonstrated no excess of mortality or risk of major adverse cardiac events (MACE) for PCI of the ULM when compared with CABG8-14. As a result PCI is considered as an alternative therapy to CABG by the European Society of Cardiology depending on individual risk stratification15.
Acute coronary syndrome (ACS) related to ULM disease is particularly challenging and represents a distinctive subset. In this setting, PCI might be the only therapeutic alternative, particularly in presence of haemodynamic instability, such as cardiac arrest or cardiogenic shock (CS). This study examined the outcomes of PCI of ULM for de novo lesions in patients presenting with ACS in two Swiss medical centres with a focus on the impact of clinical variables at the time of diagnosis.
Methods
Patient population
Between June 1995 and March 2007, a total of 28,798 patients underwent PCI at our institutions. We retrieved all patients with ULM-PCI suffering from acute coronary syndrome due to de novo stenosis from our database and identified 134 consecutive patients representing the current study population. Medical records including pre-hospitalisation medical history, physical examination, laboratory tests, coronary angiography and ventriculography, 12-lead ECG, PCI reports, as well as post-procedural echocardiography were reviewed. The revascularisation risk was estimated using the surgical logistic EuroSCORE (European system for cardiac operative risk evaluation)16.
Patients were classified into two groups according to their initial presentation: CS/STEMI group, for patients presenting with CS or ST-elevation myocardial infarction; NSTEMI/UA group, for patients with non-STEMI or unstable angina.
The study complied with the Declaration of Helsinki regarding investigations in humans and was approved by the institutional ethics committee at the Bern University Hospital, Switzerland. No extramural funding was used to support this work. All authors have read and approved to the manuscript as written, and are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper, and its final contents.
Quantitative coronary angiographic analysis
Coronary angiograms were recorded at baseline and immediately after the intervention. Digital angiograms were analysed at the angiographic core laboratory at the Bern University Hospital, Switzerland, with the use of an automated edge-detection system using the CMS-GFT algorithm (MEDIS, Leiden, The Netherlands). TIMI flow and Syntax scores were computed post hoc. Quantitative measurements included the diameter of the reference vessel, minimal luminal diameter, and percent diameter of stenosis (defined as the diameter of the reference vessel minus the minimal luminal diameter, divided by the reference diameter and multiplied by 100).
Follow-up
Patients were clinically followed for six months. Information regarding clinical status was collected at clinic visits or by telephone interview. When the patient was not accessible, data were retrieved from the referring physician or hospital electronic database. Routine follow-up angiography was advised as part of the routine follow-up.
Definitions
ULM was considered by angiographically documented stenosis >50% located in the left main coronary artery with no patent graft to the left anterior descending or circumflex coronary artery. ACS was defined according to the consensus paper from the ESC–ACC–AHA–WHF Joint Force17. Cardiogenic shock was defined as sustained hypotension (systolic blood pressure (BP) <90 mmHg lasting >30 minutes) accompanied by signs of tissue hypoperfusion in the setting of clinically adequate or elevated left ventricular filling pressures18. Hypercholesterolaemia was defined according to the reports of the National Cholesterol Education Programme: from 1995 till 2002 according to the Adult Treatment Panel II and from 2002 onwards according to the Adult Treatment Panel III19,20. Technical success was defined as successful deployment of a stent in the target lesion. Procedural success was defined as ULM revascularisation with ≤ 30% residual diameter stenosis by quantitative coronary angiography, without major procedural or post-procedural adverse events (death, myocardial infarction, emergency target vessel revascularisation or acute stent thrombosis).
Death was classified as either cardiac or non-cardiac, according to the Academic Research Consortium (ARC) definition. Deaths that could not be classified were considered cardiac. Target lesion revascularisation (TLR) was defined as any repeat percutaneous intervention of the target lesion. The target lesion was defined as the treated segment from 5 mm proximal to the stent to 5 mm distal to the stent. Target vessel revascularisation (TVR) was defined as any repeat PCI of any segment of the target vessel, defined as the entire major coronary vessel proximal and distal to the target lesion, including upstream and downstream branches and the target lesion itself. Major adverse cardiac event (MACE) was defined as the occurrence of cardiac death (CD), non-fatal myocardial infarction (MI), or TVR during the follow-up period. Definite, probable and possible stent thromboses were determined according to the ARC definitions. Stent thrombosis was defined as early, late, and very late if the event occurred within 30 days, <1 year, or >1 year, respectively, after the procedure.
Statistical analysis
For continuous variables QQ plots were computed to check for a normal distribution. Normally distributed variables were analysed using parametric tests and non-normally distributed data using non-parametric tests. Continuous variables are expressed as mean±standard deviation or median with interquartile range. Differences were compared using Student’s-t test or Mann Whitney U test. Categorical variables are expressed as counts and percentages. MACE were reported hierarchically. We established contingency tables for categorical variables and used the chi-square and the Fisher’s exact test to account for differences between the two groups. A binary logistic regression model was computed using a forward-stepwise selection. We included all pre-procedural variables that had a significance level of <0.25 in the univariate analysis to show which variables are independently associated with the affiliation to either group 1 or group 2. Cumulative incidence of endpoints was estimated by the Kaplan Meier method and differences were assessed with the log-rank test. P-values are two-sided with a significance level of 0.05. Analyses were performed using SPSS software 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
ULM-PCI in the acute setting represented 0.5% of PCI performed between March 1995 and June 2007 at our institutions. From 134 patients included in the study, three patients were excluded from the analysis due to missing medical records. From the remaining patients, 65 presented with CS or STEMI and 66 with NSTEMI or UA.
Baseline clinical characteristics
The baseline patient characteristics are summarised in Table 1. No significant differences were found between both groups except that dyslipidaemia and previous revascularisations were less frequent in the CS/STEMI group than in the NSTEMI/UA group.
Key clinical and angiographical variables at time of diagnosis are depicted in Tables 1 and 2. Patient’s morbidity and lesion complexity were higher in the CS/STEMI group than in the NSTEMI/UA group: higher EuroSCORE (11±4 vs. 9±4, p=0.003), lower LVEF (34±14% vs. 49±18%, p<0.001), higher SYNTAX score (24±10 vs. 17±11, p<0.001), higher stenosis grade (78±19% vs. 67±19%, p=0.001), smaller minimum lumen diameter (0.77±0.73 mm vs.1.17±0.75 mm, p=0.003) and slower TIMI flow (1.7±1.3 vs. 2.9±0.5, p<0.001). Interestingly, 15 patients in the CS/STEMI group but only one in the NSTEMI/UA group presented with complete thrombotic occlusion of ULM (p=<0.001).
Using a logistic regression model the presence of dyslipidaemia (OR 6.22; 95% CI 1.2-32.3, p=0.03), a high pre-procedural TIMI score (OR 3.89; 95% CI 1.4-10.82, p=0.01), as well as a preserved left ventricular ejection fraction (OR 1.07; 95% CI 1.02-1.12, p=0.01), and the left main as culprit lesion (OR 8.57; 95% CI 1.61-45.57, p=0.01) were independently associated with the development of NSTEMI or unstable angina. In turn, patients that did not present the aforementioned features were more likely to present with CS or STEMI.
Procedural characteristics
Mechanical circulatory assistance was more frequently used in the CS/STEMI group than in the NSTEMI/UA group: intra-aortic balloon pump (38% vs. 8%, p<0.001), percutaneous ventricular assist devices (pVAD) such as TandemHeart (Cardiac Assist, Inc., Pittsburgh, PA, USA) or Impella (Abiomed Inc., Danvers, MA, USA)(pVAD, 11% vs. 8%, p=0.51), other extracorporeal bypass pump (1.6% vs. 0%, p=0.49).
More lesions were treated in the CS/STEMI group (1.8±1.0 vs.1.5±0.8, p=0.04) - leading to a higher percent of patients treated concomitantly in the left anterior descending coronary artery (p=0.04) - than in the NSTEMI/UA group. In both groups, 64% of all ULM lesions were distal and 25% of these were treated with a double stent approach. The favoured stenting technique was (provisional) T-stenting. Differences depending on stenting techniques were tested and were not significant. Furthermore, bare metal (vs. drug-eluting) stents were more often used in the CS/STEMI group than in the NSTEMI/UA group (42 vs. 26%, p=0.04). Use of post-dilatation, the size of the biggest balloon (p=0.20) and the maximum pressure employed (p=0.08) did not significantly differ between the groups. Technical success (98% vs. 96%, p=0.32) and post-procedural angiographic characteristics were similar (Table 2). Of note, no more difference was found in coronary blood flow (mean post-procedural TIMI flow 3.0±0.2 in both groups) at the end of PCI.
Clinical outcome
During hospitalisation, the MACE rate was higher in the CS/STEMI group (33%) than in the NSTEMI/UA group (11%, p<0.001). This was mainly due to an increased mortality in this group (all-cause mortality: 33% vs. 5%, p<0.001; cardiac mortality: 26% vs. 3%, p<0.001). Five deaths (4%) were non-cardiac. From these, three (3%) were attributable to major bleeding. Median survival time from definite diagnosis to in-hospital death was five days (IQR 1-8 days).
Follow-up at 6 months was available in 125 patients (95%) and is summarised in Table 3a. Angiographic follow-up was performed in 34 patients (26%). Survival and survival free of MACE are depicted in Figure 1. Survival was influenced by the ACS type (p<0.001) and the initial coronary TIMI flow (Figure 2, p=0.027). As depicted in Table 3a and b, CS was associated with the poorer outcome. Survival free of MACE was independent from lesion location (p=0.39), stenting approach (p=0.41), and type of stent used (BMS vs. DES, p=0.15).
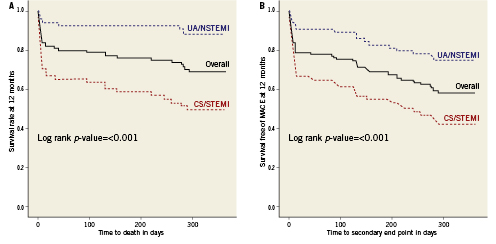
Figure 1. Kaplan-Meier curves for survival (A) and survival free of MACE (B) according to ACS type. ACS: acute coronary syndrome; CS: cardiogenic shock; NSTEMI: non-ST elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; UA: unstable angina
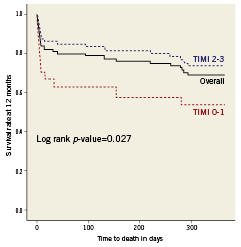
Figure 2. Kaplan-Meier curves for survival according to initial coronary TIMI flow. TIMI: Thrombolysis In Myocardial Infarction flow grad
Using a regression model, we explored the association between initial clinical variables and mortality at 6 months. SYNTAX score (OR 1.08; 95% CI 1.0-1.2, p=0.04), left ventricular ejection fraction (OR 0.91; 95% CI 0.84-0.99, p=0.02), and stenosis >50% in vessels other than ULM (OR 10.7; 95% CI 1.0-109.7, p=0.05) were independent predictors of mortality.
Discussion
The principal limitations of ULM-PCI consist of (1) a large area at risk, (2) bi/trifurcation disease, and (3) a higher risk of stent thrombosis and restenosis. In practice, the limitations are cumulative and put to an extreme in patients suffering from acute coronary syndrome due to ULM disease. In the patients reported, ULM-PCI was considered as the only valuable therapeutic option. This is particularly well illustrated by the 16 patients suffering from complete ULM occlusion.
The main findings of the present study are: 1) Survival-free from death and myocardial infarction six months after ULM-PCI is poor in patients suffering from ACS; 2) From these, the severity of ULM stenosis, presence of concomitant CAD in another coronary segment, LV dysfunction, and circumstance of presentation were associated with even poorer outcome; 3) Accordingly, patients presenting with cardiogenic shock and STEMI had a gloomy prognosis leading to death in half of cases at six months.
These findings are interesting since only little evidence is currently available on this particular subject21. Palmerini and colleagues recently published the clinical outcome of patients treated by ULM-PCI for acute coronary syndrome (n=611) in comparison to stable angina (n=490). They found that ACS was associated with a 2- to 3-time increased risk of cardiac mortality and myocardial infarction during a 2-year follow-up. They excluded patients with STEMI and those in cardiogenic shock22. In these patients, however, it seems comprehensible that EuroSCORE, SYNTAX score, pre-procedural TIMI flow, impairment of LVEF and degree of ULM stenosis further impact clinical outcome23,24. Consistently, patients suffering from STEMI or cardiogenic shock due to ULM disease have a dismal outcome as illustrated in Table 4.
The increased risk of cardiac mortality in patients with cardiogenic shock and STEMI was proportional to a higher global clinical risk profile. This was particularly germane to the subgroup of 16 patients presenting with ULM obstruction. In this particular group, 6-month mortality was 42% despite the use of an aggressive therapeutic armamentarium as glycoprotein IIb/IIIa inhibitors in 71% and left ventricular assist devices in 67%. A more liberal utilisation of ventricular support in conjunction to IABP should be considered to improve the prognosis of patients presenting with CS.
Finally, we found that hypercholesterolaemia was negatively associated with cardiogenic shock in this specific population. This was unexpected and might be a consequence of play of chance, or be due to selection bias as patients with CS/STEMI are less likely to be questioned about their history than more stable patients. Taking out the 13 patients intubated or in cardiac arrest did however not change this fact (p=0.007). Consistently and similarly, Vauthey and colleagues found out that hypercholesterolaemia at presentation for stroke was associated with better clinical outcome25. In line with this hypothesis, statin treatment among patients undergoing emergency PCI for STEMI and cardiogenic shock has been associated with a significant mortality advantage at early follow-up25. One can speculate that treatment of dyslipidaemia will lessen the risk of plaque rupture and the development of cardiogenic shock. This is the case in our population.
Limitations
The present study was a retrospective multicentre registry and therefore lacks randomisation and intention-to-treat data. Since no sample size calculations were performed, we acknowledge that our results may be affected by a type II error. Secondly, heterogeneity is found regarding technology (DES, pVAD) and pharmacotherapy due to the long inclusion period and the constant improvements in interventional cardiology during this period.
Conclusion
Acute coronary syndrome due to critical ULM stenosis is associated with high mortality even after successful PCI. Patients presenting with CS or STEMI are at particular risk.
Conflict of interest statement
The authors have no conflicts of interest to declare.