Abstract
Aims: Percutaneous coronary intervention (PCI) is increasingly being used for unprotected left main (ULM) disease. Limited data are available on sex-related differences in this setting. We investigated gender-associated differences in patients undergoing stent-based PCI for ULM.
Methods and results: We analysed baseline, procedural and long-term data of patients with ULM undergoing stent-based PCI at participating centres. The primary end-point was the long-term rate of major cardiovascular events rate (MACE, i.e., the composite of death, myocardial infarction, or target lesion revascularisation). The study population included 1,452 cases, with 27.8% females and 72.2% males. Women were older, more frequently diabetic, hypertensive or presenting with an acute coronary syndrome, and thus with a higher EuroSCORE, but were less commonly treated with drug-eluting stents (DES), in comparison to men (all p<0.01). After a median follow-up of 18 months, women showed an unadjusted higher risk of death (p=0.040), cardiac death (p=0.033), and the death/myocardial infarction (p=0.012). However, after multivariable adjustment, gender was no longer an independent predictor of death (hazard ratio=1.119 [0.804-1.558]), cardiac death (hazard ratio=1.045 [0.697-1.567]), or death/myocardial infarction (hazard ratio=0.531 [0.192-1.465]), given the predominant role of age, diabetes and EuroSCORE as independent predictors and confounders of the gender-based comparison.
Conclusions: Women undergoing PCI for ULM present more often with an acute coronary syndrome, are treated less frequently with DES, and have more adverse events, but these gender biases are not confirmed after adjusting for confounders. Thus, stent-based PCI for ULM offers similarly favourable clinical results in women as well as in men.
Introduction
A significant lesion of the unprotected left main (ULM) is identified in as much as 5-10% of coronary angiographies.1 Even though coronary artery bypass grafting (CABG) has been considered the “gold standard” treatment for these patients since the late ‘70s,2,3 percutaneous coronary intervention (PCI) is becoming a rather popular procedure in many catheter laboratories all over the world. This is mainly due to the introduction of drug eluting stents (DES), which reduce restenosis and target lesion revascularisation (TLR) rate in comparison to balloon-only PCI or bare metal stents (BMS).4
Several studies have already reported on stent-based PCI for ULM disease in the DES era,4,5 but the populations of these studies, mainly registry-based, encompassed a majority of males, partially reflecting the epidemiology of coronary disease. Important gender-related disparities have already been reported in the diagnosis, prognosis and treatment in cardiovascular disease in general,6 and in coronary artery disease in particular.7,8 In addition, gender may affect coronary anatomy, with females displaying shorter and smaller size vessels, including the ULM.9 It is conceivable that gender may have an important role also in the prognosis and treatment of patients undergoing stent-based PCI for ULM disease. Yet, there are no data so far focusing on this important topic.
We thus aimed to investigate gender-related disparities among subjects enrolled in a multicentre Italian registry focusing on stent-based PCI for ULM disease.
Methods
Study design, patient population and study procedures
Our work is based on a multicentre retrospective observational study realised with the participation of all high-volume Italian interventional cardiology centres performing > 800 PCI per year and affiliated with Italian Society of Invasive Cardiology.10 Briefly, between January 2002 and December 2006, 1,452 consecutive patients with ULM stenosis treated by means of PCI were enrolled. Eligible subjects were those with clinically symptomatic ULM disease with angiographic evidence of > 50% diameter stenosis eligible for stent implantation. Age and comorbidities were not exclusion criteria, but patients with ST-segment elevation myocardial infarction (MI) necessitating primary PCI or patients with cardiogenic shock at admission were not included in the registry given their peculiars characteristics and adverse clinical features. Informed written consent was obtained for all patients, and the study was in agreement with the local ethics committees.
In particular, patients were offered percutaneous revascularisation or cardiothoracic surgery according to the standard of care of each centre. Coronary angioplasty and stent implantation reflected current practice and guidelines, with the choice of device, stenting strategy and use of glycoprotein IIb/IIIa inhibitors at the operator’s discretion. After the procedure, all patients were prescribed lifelong aspirin and either 250 mg ticlopidine twice daily or 75 mg clopidogrel for six to 12 months.
Main outcome measures
As primary endpoint, we assessed the incidence of major adverse cardiac events (MACE), i.e., the composite of death, MI, or TLR. Deaths were classified as either cardiac and non-cardiac, with all deaths considered cardiac unless an unequivocal non-cardiac cause could be established. The diagnosis of MI was validated using a combination of symptoms, ECG findings and serum biomarkers. Periprocedural MI was defined as an increase in creatine phosphokinase levels > 3 times the upper reference limit in the first 48 hours after PCI. Repeat TLR included repeated percutaneous or surgical intervention in the previously treated segment involving the implanted stent and the 5-mm distal and proximal edges. Secondary outcomes measures were the single components of MACE, cardiac death and a composite of death and MI.
Follow-up and data collection
Data collection from institutional databases was comprehensive of baseline clinical characteristics, procedural and follow-up information, and all these variables were aggregated in a dedicated central database. Clinical follow-up was performed during direct patients visits, by telephone interviews or by consulting civil registries of mortality when patients could not be contacted either way. Although strategies concerning follow-up angiography varied among centres, most patients underwent at least one angiographic follow-up.
Statistical analysis
The goal of our analysis was to explore gender-related differences in patient presentation, treatment and outcomes in patients with ULM disease managed with PCI. We reported means and standard deviations for continuous variables, differences among groups were tested by unpaired Gossett t test. Categorical variables were expressed as counts and percentages and were compared by χ2 or Fisher exact test. Multivariable binary logistic and Cox proportional hazard analyses was performed to appraise the gender-related differences simultaneously adjusting for all variables with significant (p < 0.05) or borderline significant (p ≤ 0.10) association with gender at univariate analysis, as well as including by default diabetic status, EuroSCORE, and disease location in the ULM. Results of these analyses are reported as odds ratios (OR) or hazard ratios (HR) with 95% confidence intervals. All computation were performed with SPSS 11.0 (SPSS, Chicago, IL, USA).
Results
Baseline and procedural characteristics
A total of 1,452 patients were included in our study, with 404 females (27.8%). Analysis of baseline features showed that women were significantly older (p<0.001), had more commonly hypertension (p=0.011), diabetes mellitus (p<0.001), and a higher EuroSCORE (p<0.001), but were less commonly smokers (p<0.001) (Table 1). Notably, women were much more likely to be admitted with a diagnosis of acute coronary syndrome (269 [67%] vs. 580 [55%] in men, p<0.001), a difference which proved significant even after extensive multivariable adjustment (p=0.014).
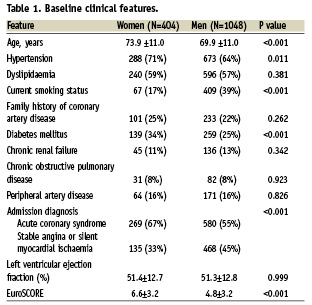
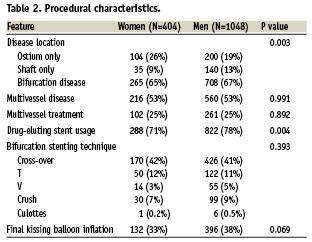
Comparison of procedural features showed that women had higher prevalence of ostium ULM disease (p=0.003), and were less likely to be treated with DES (p=0.004) in comparison to men. Other angiographic and technical data were between genders, including extent of multivessel disease, rate of multivessel PCI, and choice of bifurcational stenting technique (all p>0.05). Notably, the apparent bias against DES usage in women disappeared after extensive multivariable adjustment (p=0.491), thus suggesting that device choice did not depend on gender but rather on patient presenting features and thrombotic/bleeding risk.
Clinical outcomes at univariate and multivariable analyses
Early (30-day) outcomes proved different between genders, with a significantly higher risk of death (p=0.001) and MACE (p=0.002) in females (Table 3), whereas long-term follow-up after a median follow-up of 18 months (with 12 [0.8%] losses to follow-up), showed significantly higher rates of death (p=0.040), cardiac death (p=0.033), and death/MI (p=0.012) in women, despite similar rates of TLR (p=0.620) and MACE (p=0.553).
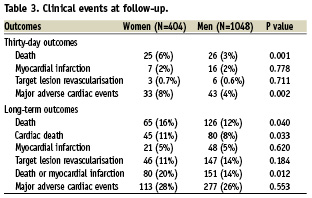
After multivariate adjustment, gender was no longer an independent predictor of any early or long-term adverse events, including 30-day MACE, 30-day and long-term death, long-term cardiac death, and long-term death/MI (all p>0.05), given the predominant role of age, diabetes and EuroSCORE as independent predictors and confounders of the gender-based comparison (Table 4 and Figure 1). Specifically, diabetes mellitus and EuroSCORE independently predicted 30-day all cause death (respectively OR=1.449 [1.008-2.082], p=0.045, and OR=1.506 [1.379-1.645], p<0.001), long-term all cause death (HR=1.436 [1.053-1.958], p=0.022, and HR=1.309 [1.238-1.383], p<0.001), long-term cardiac death (HR=1.534 [1.051-2.238], p=0.027, and HR=1.317 [1.231-1.408], p<0.001), and the composite of long-term death or MI (HR=1.359 [1.019-1.812], p=0.037, and HR=1.287 [1.189-1.324], p<0.001). Thirty-day MACE were also predicted by diabetes mellitus, with the additional independent prognostic role of age (OR=0.980 [0.962-0.998], p=0.028) and distal ULM involvement (OR=1.372 [1.047-1.796], p=0.022). Finally, we found no significant interaction between age and gender (all p>0.05), or between DES usage and gender on the risk of adverse events (all p>0.05).

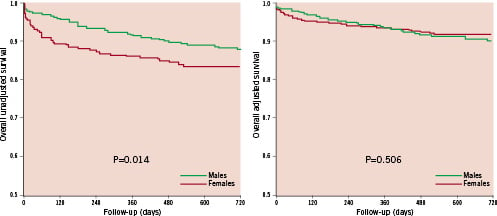
Figure 1. Overall survival according to gender at unadjusted (left panel) and multivariable adjusted (right panel) Cox proportional hazard analysis.
Discussion
The major findings of this study evaluating gender-related differences in patients undergoing PCI for ULM disease are four-fold: (1) women that elected to undergo ULM stenting more commonly presented with an acute coronary syndrome, possibly because of a higher diagnostic threshold for ischaemia; (2) another significant gender difference was in disease location, as women had more frequent ostial ULM disease than men; (3) women are also treated more rarely with DES, but this largely depends on their higher procedural and thrombotic/bleeding risk; (4) adverse events are apparently more frequent in women, but these gender biases are not confirmed after adjusting for confounders; (5) thus, stent-based PCI for ULM may offer similarly favourable clinical results in women as well as in men.
The recognition of sex disparities in the epidemiology, diagnosis and treatment of cardiovascular disease are well-established.11 However, a huge knowledge deficit still persists about the influence of gender on treatment patterns and outcomes of coronary revascularisation. In the severe subset of ULM disease, even if a recent prospective multicentre randomised study confirmed CABG to be the standard of care, no analyses were ever conduced focusing on gender.5
Actually, women are usually older and have more comorbidities when they present with coronary artery disease. Moreover, they usually experience a delay in the clinical diagnosis, which may easily translate into increased procedural morbidity and mortality even after coronary revascularisation is eventually performed.12
Surgical coronary revascularisation in women faces an increased technical difficulty due to smaller reference vessel diameters than in men.13 This has been elegantly demonstrated in an intravascular ultrasound study appraising coronary size after cardiac transplant.9 Specifically, Herity and colleagues have shown in such an instance that in hearts harvested from female donors and transplanted to male recipients, there was a unique and significant increase in left anterior descending vessel area two years after transplantation. Given the more prevalent occurrence of diffuse and small vessel disease in women, the percutaneous approach to ULM treatment could be of peculiar usefulness for female patients, and the present study supports its role suggesting that a gender bias does not exist when underlying confounding factors are considered (i.e., differences in baseline and procedural risk factors).
In line with older studies and registries,8,14 our short-term results revealed worse early outcomes in women. Specifically, we found differences in rates of 30-day MACE and long-term death/MI, both largely driven by differences in mortality. These data may be partly explained by the burden of comorbidities and unfavourable coronary anatomic features. Particularly, they may be the effect of the higher procedural risk typical of women. In addition, it can be hypothesised that more men presenting worse clinical features (e.g., higher EuroSCORE) were treated preferentially with CABG. Despite this, no substantial difference in mid-term outcomes emerged among genders after multivariable adjustment, whereas age and diabetes turned out to be the predominant independent predictors of death and confounders of the gender based comparison.14
The present multicentre study reflects current Italian practice in the percutaneous management of ULM, since all high-volume Italian interventional cardiology centres participated in data collection. Retrospective observational analyses were conducted on a large sample size, and, though many similar registries have been published to date5,16-18 to the best of our knowledge this study is the first to report on sex-related outcomes after PCI for ULM disease.
Study limitations
This work has all the drawbacks inherent to a retrospective observational study. In addition, data on cardiac medication prescribed after the study procedure could not be retrieved. It was not possible to obtain data on patients treated with CABG instead of PCI or on those undergoing CABG because of failed PCI, as our study population encompasses only those cases actually undergoing PCI. Similarly, precise risk estimates of stent thrombosis were not available.
Losses to follow-up were low, 12 (0.8%), but it has to be underlined that some patients were followed-up only by telephone interview. Thus all cases have been included in the main analysis. Median follow-up lasted on average 18 months. Probably this period may not be sufficient to reflect the true long-term effect of stent-based PCI on hard clinical endpoints and comparing females vs. males. Longer-term follow-up with respect to outcomes would provide additional evidence on the potential presence gender-related bias in this setting. Nonetheless, it is unlikely that much longer follow-up can disclose clinically meaningful differences in the risk of MACE or other adverse events in men vs. women.
Conclusions
In conclusion, whereas this study suggests an apparent mortality excess among women undergoing PCI for ULM in the current era, this gender bias is not confirmed after adjusting for other important prognostic factors, demonstrating that females face a similar outlook in comparison to males even if they have worse clinical features (higher age, EuroSCORE and prevalence of acute coronary syndrome as admission diagnosis and diabetes mellitus). Thus, notwithstanding the important prognostic role of different baseline risk profile among genders, PCI for ULM offers favourable mid-term clinical results in women as well as in men.
Appendix
This registry has been possible through the contribution of the following colleagues: L. Bolognese (Dipartimento Cardiovascolare, Ospedale S. Donato, Arezzo); G. Lauria (Istituto Cardiologia, Policlinico S. Orsola, Università di Bologna); M. Di Salvo (Dipartimento di Cardiologia, Ospedale Ferrarotto, Università di Catania); S. Vecchio (Dipartimento Cardiovascolare, Ospedale Careggi, Università di Firenze); P. Buja, G. Grassi, and P. Millosevich (Ospedale Civile, Mestre); P. Ravagnani, D. Trabattoni, F. Fabbiocchi, P. Montorsi, A. Lualdi, and S. Galli (Centro Cardiologico Monzino, Dipartimento di Scienze Cardiovascolari, Università di Milano); M. Ferraro (Centro Emocolumbus, Milano); G. D’Annibale (Dipartimento di Cardiologia, Hesperia Hospital, Modena); D. Tavano (Dipartimento di Cardiologia, Clinica Mediterranea, Napoli); M. Pepe (Dipartimento di Scienze Cardiovascolari, Università di Padova); A. Patti (Dipartimento Cardiovascolare, Ospedale Cervello, Palermo); D. Ardissimo (Unità Operativa di Cardiologia, Azienda Ospedaliero-Universitaria, Parma), S. Petronio (Dipartimento Cardio-Toracico, Ospedale Cisanello, Università di Pisa); A. Maresta (Dipartimento di Cardiologia, Ospedale S. Maria delle Croci, Ravenna); G. Piovaccari (Dipartimento di Cardiologia, Ospedale degli Infermi, Rimini); M. Medda and L. Inglese (Cardiovascular Interventional Radiology Department, IRCCS Policlinico S. Donato, S. Donato Milanese).

