Abstract
Aims: To assess the 30-day clinical outcome of endovascular and surgical revascularisation procedures in patients with carotid obstructive disease (COD) and concomitant coronary artery disease (CAD).
Methods and results: Between January 2006 and December 2009, 659 patients with COD and concomitant CAD were treated. The incidence of the primary endpoint (composite of death, MI and stroke) was 4.25% (0.9%, 1.1% and 2.3%, respectively). Acute renal insufficiency occurred in 2.4% and major bleedings in 4.4% of patients. According to the treatment forms patients were divided into three groups: surgical, 185 patients (28.1%), endovascular, 378 (57.4%), and hybrid, 89 (13.5%). Seven patients (1%) were managed medically only. The primary endpoint of the study occurred in 4.8%, 2.4% and 8.6%, respectively, p=0.01. The secondary endpoint, that included the occurrence of renal or respiratory insufficiency and major bleedings occurred in 10.1%, 6.5% and 23.8%, respectively, p<0.001. At multivariate logistic regression analysis renal insufficiency (OR=2.517; 95%CI=1.077-5.883, p=0.03) and treatment group (endovascular: OR=0.369; 95%CI=0.168-0.813, p=0.01 or hybrid: OR=3.098; 95%CI=1.359-7.060, p=0.007) predicted the primary endpoint.
Conclusions: Surgical and endovascular treatments yield very good immediate results; the later being less invasive, may be particularly suited to these fragile and complex patients. Long-term follow-up is under assessment.
Introduction
The co-existence of atherosclerosis in different vascular districts is known as plurivascular disease, a pathological condition that continuous to expand in parallel with life expectancy. In fact, with ageing atherosclerotic plurivascular disease becomes a leading cause of morbidity needing hospitalisation and cure as well as a cause of mortality1,2.
Revascularisation of macro-circulatory systems affected by atherosclerotic lesions can be achieved by both surgical and endovascular means. A large body of evidence is available regarding the long-term outcome of surgical and endovascular procedures applied in patients with coronary artery disease (CAD). Less information has been obtained from patients with carotid obstructive disease (COD), and very little is known about the advantages, shortcomings, and long-term outcomes of patients having concomitant CAD and COD that may be referred to completely surgical or endovascular interventions, or managed with a combined (hybrid) approach that includes both forms of treatment3,4.
As there are no available randomised comparisons of this kind in such an important, and rapidly growing subset of patients, we initiated a systematic assessment of clinical outcomes in consecutive patients with COD and associated CAD referred for cardiovascular interventions to high volume centres dedicated to the treatment of plurivascular disease.
Thus, the aim of the present study was to analyse the 30-day clinical outcomes of a wide population of patients with concomitant CAD and COD treated according to the “best standards of care”. These patients belong to a larger database that includes patients entered with also other forms of plurivascular disease and treatment as defined by the FRIENDS (Finalised Research In ENDovascular Strategies) study group, an Italian, spontaneously generated, independent, non profit association.
Present members are part of high-volume institutions committed to cardiovascular care and work with a shared intention under a common coordination. The initial goal of the group is to assess the short, intermediate and long-term outcome of revascularisation procedures applied to patients with complex, plurivascular disease with a multi-disciplinary approach5.
Material and methods
Patient population
Patients with a concomitant COD and CAD, documented with selective angiography performed in each participating centre between January 2006 and December 2008, were extracted from the common FRIENDS database, with the intention of focusing on this issue in the previously collected individual datasets developed in each centre. Clinical follow-up was obtained prospectively by either clinical visits or telephone contact at 30 days.
All patients included in this study gave informed consent to undergo the proposed treatment and follow the pre-specified follow-up program. The ethical committees of each participating institution were informed about the aims and methods of this study.
Diagnosis of CAD and COD
CAD was diagnosed by selective angiography when a stenosis >70% was present in at least one of the major coronary branches or >50% in the left main, and was conventionally classified according to the degree of involvement of the coronary tree. According to clinical presentation, CAD was classified as stable, (including patients with silent ischaemia); or acute coronary syndromes (ACS), including patients with unstable angina (UA), non ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI).
COD was diagnosed in clinically symptomatic patients when congruent signs of cerebral ischaemia detected by imaging techniques were associated to neurological manifestations of ischaemic nature. COD was confirmed by selective angiography in almost all cases and when an endovascular treatment was considered, or by non-invasive means only in patients with a preferred indication for surgical revascularisation. COD was diagnosed when a stenosis >70% involving the internal carotid artery was identified at selective angiography or when a peak systolic velocity >130 m/sec was detected by duplex ultrasound. In neurologically asymptomatic patients, angiography was performed according to current recommendations6, mostly in those with severe CAD, with urgent need for CABG, with clear evidence of significant carotid disease as diagnosed by non-invasive means or in cases of non-diagnostic findings because of technical limitations of the non-invasive imaging.
Chronic kidney disease was diagnosed and classified according to the National Kidney Foundation criteria, based on the calculated glomerular filtration rate (GFR)7.
Interventions
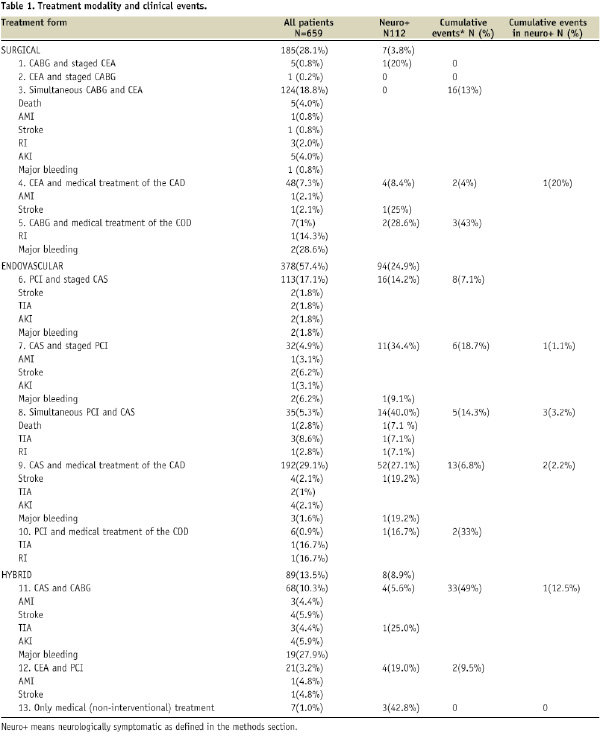
Each of the participating centres developed a local team of experts in vascular medicine to discuss the therapeutic indications in this specific patient’s setting5. The cardio-vascular team included cardiac and vascular surgeons, and clinical and interventional cardiologists, and opinions from neurologists were required as needed. Therapeutic decisions were applied individually for each patient according to best knowledge and local expertise, and are summarised in Table 1.
Coronary or carotid interventions were mandated either by symptoms as well as by the indications proposed from current guidelines6,8. Staged interventions are intended as those performed within a range of 1-45 days from the first; while simultaneous interventions are those performed during the same access to the catheterisation laboratory or within the same day.
Coronary artery by-pass grafting (CABG) was performed “off pump” in many cases. Carotid endoarterectomy (CEA) and percutaneous coronary interventions (PCI) were performed according to conventional techniques. Local anaesthesia was preferred for CEA when suitable. Stent placement was performed in nearly 100% of PCI after balloon dilatation, or vessel preparation with rotational atherectomy when needed. As to the technical aspects of carotid artery stenting (CAS), different kinds of stents and distal protection devices were used according to individual clinical and anatomical characteristics as recommended by experts9.
Data collection
Patients information was entered in a common dedicated database. Clinical events were assessed in-hospital and one month after discharge.
Endpoints
The primary endpoint of the study is the occurrence of major adverse cardiac and cerebral-vascular events (MACCE) at 30 days, including any death, myocardial infarction (MI) and any stroke.
Secondary endpoints of the study are the assessment of the in-hospital outcome comprised in the primary endpoint including also complications related to the procedures such as: transient ischaemic attacks (TIA), major bleeding, acute kidney injury (AKI) and need for dialysis after CAS or PCI. TIA, major bleeding, AKI and need for dialysis, cranial-nerve palsy, respiratory insufficiency (RI) needing mechanical ventilation, or other complications at the surgical site of the vascular access after CEA or CABG.
Study endpoint definitions
Death: all deaths will be considered irrespective of its aetiology.
Myocardial infarction (MI): is defined as either the development of pathologic Q waves lasting at least 0.4 second in at least two contiguous leads with an elevation of the CK MB fraction level or, in the absence of pathologic Q waves, an elevation in CK MB fraction levels to more than 3 or 5 times the UNL (Upper Normal Limit) for PCI and CABG respectively.
Stroke: ischaemic neurologic deficit that persisted for more than 48 hours as assessed by the neurologists, confirmed by brain imaging and quantified with the use of the National Institutes of Health Stroke Scale, the Barthel index of functional levels in activities of daily living, and the Rankin scale of functional disability as proposed by the SAPPHIRE investigators10.
Transient ischaemic attack (TIA): a brief episode of neurological dysfunction caused by a focal brain or retinal ischaemia, with clinical symptoms typically lasting less than one hour and without evidence of acute infarction11.
Acute kidney injury (AKI): intended as either a contrast-induced nephropathy (with or without the need for dialysis) and return to baseline, or with persistent lost of at least 25% of the baseline GFR12.
Bleeding: according to recent interventional trials, major bleeding was defined as the occurrence within 30 days of treatment of intracranial or intraocular bleeding, haemorrhage at the access site requiring intervention, haematoma with a diameter of at least 5 cm, a reduction in haemoglobin levels of at least 4 g per decilitre without an overt bleeding source or at least 3 g per decilitre with such a source, reoperation for bleeding, or transfusion of a blood product13.
Statistical methods
Continuous data are expressed as means and standard deviations; discrete variables are given as absolute values and percentages. The Student’s t-test or Kruskal-Wallis test were used to compare differences between continuous variables, where appropriate. The chi-square statistic with Yates’ correction, or Fisher’s exact test when appropriate, were used to test associations of categorical data. Differences between the endovascular versus either the surgical or the hybrid group were also assessed by means of multi-comparison tests (Brandt-Snedecor or ANOVA with the Bonferroni’s Method, where appropriate). Univariate analysis to test the relation between the clinical and treatment variables and the occurrence of events included in primary and secondary endpoints was performed by means of binary logistic regression, obtaining also the odds-ratio for each parameter. A multivariate logistic regression model was then created including relevant variables to identify independent predictors of outcome. All tests were two-sided. A probability value of less than or equal to 5% was considered significant. SPSS version 15 and Microsoft Excel 2003 was used for the data analysis.
Results
Between January 2006 and December 2009, 659 patients with COD and concomitant CAD were referred to our hospitals for vascular care and underwent revascularisation on at least one of the two vascular districts. Data regarding in-hospital and 30-day outcomes were obtained in all patients.
The type of treatment applied is shown in Table 1, and the baseline characteristics of all patients are reported in Table 2.
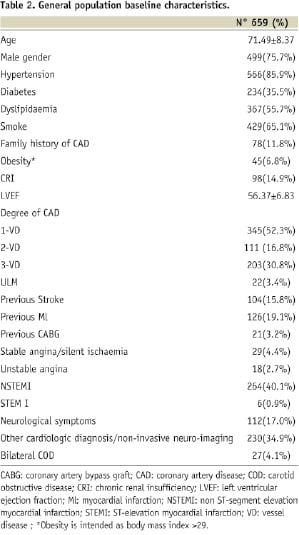
Coronary angiography was performed because of stable angina or silent ischaemia in 4.4% of patients and ACS in 44%. In the remaining cases it was performed for other reasons such as chest pain, heart failure, major ventricular arrhythmias, cardiomyopathy of recent diagnosis or as pre-surgical diagnostic screening.
Carotid angiography was performed because of history of previous stroke in 15.8%, recent neurologic symptoms in 17% of patients, because of the presence of a severe CAD in over 50% (of which 30.8% with three-vessel disease and 3.4% with critical stenosis of unprotected left main) and because of a severe carotid stenotic disease detected by non-invasive means in the remaining 17%.
Overall, 48.6% of patients received a multivessel coronary treatment (215 by CABG), and 4.1% a bilateral carotid revascularisation. CEA was performed under local anaesthesia in 20 patients (10%) and 30.2% of CABG patients (n=65), had off-pump cardiac surgery.
Regarding CAS, a distal protection device was used in 419 patients; 355 in the endovascular group (94%) and 64 (72%) in the hybrid group. A carotid stent was successfully implanted in all patients in the endovascular and hybrid groups.
The occurrence of clinical events comprised in the primary and the secondary endpoints in each treatment group is detailed in Table 1. Overall, the incidence of death, MI and stroke was 0.9%, 1.1% and 2.3%, respectively. Acute kidney injury occurred in 2.4% and major bleedings in 4.4% of patients.
For the purpose of this first analysis of the FRIENDS database, patients were divided into three groups: Surgical, that includes 185 patients (28.3%) from groups 1 to 5 of Table 1, endovascular, 378 patients (57.4%) from groups 6 to 10 of Table 1 and Hybrid, 89 patients (13.5%) form groups 11 and 12 of Table 1. Seven patients (1.0%) were managed medically only and are not described in the statistical analysis.
The comparison of the baseline characteristics of the three groups, clinical outcome, primary and secondary endpoints are shown in Table 3.
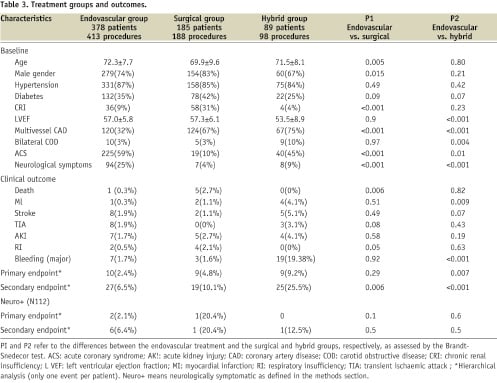
The primary endpoint of the study occurred in 4.8%, 2.4% and 9.2% respectively, p=0.01. The secondary endpoint, that included also the occurrence of renal or respiratory insufficiency and major bleedings occurred in 10.1%, 6.5% and 25.5% respectively, p<0.001.
Although all the three groups presented important high-risk characteristics, these were sensibly different as expected from the different type and timing of treatment applied.
The surgical group had younger patients, more frequently males, diabetics, with CRI and multivessel CAD. They had a higher mortality (2.7%) and more respiratory complications (2.1%) related to CABG, but despite the high-risk baseline, the incidence of MI, stroke and bleeding was very low. The endovascular group was older, and counted significantly more symptomatic patients on both, the cardiac and the neurologic district. Despite the older age and clinical instability, the incidence of death, MI and stroke was also very low. The hybrid group included more females, and was characterised by a high incidence of multivessel CAD presenting with ACS, and bilateral COD. These patients had more MACCE and in particular a high incidence of major bleeding complications.
Simultaneous versus staged procedures
The comparison of the primary endpoint between 159 patients undergoing a simultaneous revascularisation of the COD and the CAD, versus a staged revascularisation strategy performed in 240 patients yielded no significant difference (logistic regression: OR=1.496; 95%CI=0.680-3.290, p=0.32); while there was a significantly higher incidence of the secondary endpoint for the simultaneous treatment largely driven by bleeding complications and AKI: (logistic regression: OR=1.835; 95%CI= 1.108-3.040, p=0.02).
Single versus double district procedures
The comparison of the primary endpoint between 399 patients (61.2%) undergoing a double district revascularisation versus a single-district revascularisation (253 patients treated because of the CAD or the COD only and the other district managed medically) yielded a non-significant trend towards a higher incidence of MACCE in the double district group (logistic regression: OR=2.172; 95%CI=0.860-5.486, p=0.1). Such difference was instead highly significant for the secondary endpoint (logistic regression: OR=2.220; 95%CI=1.238-3.981, p=0.007).
Univariate analysis
Univariate analysis was performed by means of binary logistic regression to test the relation between the clinical and treatment variables and the occurrence of events included in primary and secondary end-points. Results, including also the odds-ratio for each parameter, are shown in Table 4.
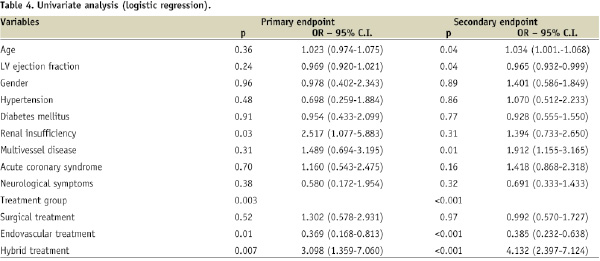
At multivariate logistic regression, a previous renal insufficiency (OR=2.517; 95%CI=1.077-5.883, p=0.03) and the treatment group were the only two independent variables associated to the primary endpoint, with an OR=0.369; 95%CI= 0.168-0.813, p=0.01 for the endovascular treatment, and OR=3.098; 95%CI=1.359-7.060, p=0.007 for the hybrid treatment. As to the occurrence of the composite secondary endpoint, age (p=0.04) and treatment group (p=0.001) were the two independent predictors of outcome. When the form of treatment (staged or simultaneous and single or double district) were included in the multivariate model, only the treatment group emerged as an independent predictor of the primary endpoint (p=0.003), with a borderline significance for age (p=0.056).
Discussion
The dissemination of atherosclerosis in multiple vascular districts denotes an aggressive manifestation of the disease that strongly determines survival. This form of presentation continues to expand in parallel with life expectancy of human beings. In fact, with ageing, atherosclerotic plurivascular disease becomes a leading cause of morbidity needing hospitalisation and care as well as a cause of mortality. Treatment of this disease modality is not standardised and depends largely on local standards and habits. Due to the lack of specific randomised controlled studies, practices in this field are often driven by reports from experts working in centres of excellence, but their results may not easily apply at large14.
The FRIENDS collaboration represents one of the largest experiences regarding this matter and as such, it permits to explore the results of different treatment strategies applied to these patients. Bearing in mind the limitations of a non randomised experience, our short-term results suggest the following interpretations. Despite the high risk of a population with plurivascular atherosclerosis, revascularisation techniques applied after a cautious selection of the most suitable strategy, in centres dedicated to vascular care, yield excellent immediate results. The very low incidence of events in our experience is similar to that recently reported from the large carotid revascularisation endarterectomy versus stenting trial (CREST)15
It is worth noting that endovascular procedures appear to be particularly appropriate to these complex patients due to their less invasive nature. Indeed, the primary endpoint rate (a composite of death, stroke, or MI within 30 days) was 50% and 70% lower among patients undergoing endovascular procedures than among those undergoing surgical or hybrid procedures, respectively. Surgery is burdened by the complications related to major cardiac operations such as AKI and RI leading to a higher mortality. However, the global outcome of surgery in our experience is excellent, likely due, at least in part, to the use of off-pump techniques by dedicated surgeons in our centres. Indeed, off-pump CABG is known to be associated with a lower incidence of stroke in patients with COD16 and periprocedural MI in this setting correlates with outcome only if CK rise is >20 times the UNL17.
Simultaneous revascularisation procedures, both surgical and endovascular appear to be acceptably safe. Most of the cases in our experience belong to the surgical group in neurologically asymptomatic patients, and results compare favourably with other series18. Simultaneous CAD and COD revascularisation by endovascular means has also been reported19 but experience is limited. However, simultaneous endovascular procedures are burdened by a higher incidence of bleeding and AKI, complications that may influence long-term survival; therefore, whenever possible, staged procedures should be preferred depending on the clinical context, limiting the simultaneous treatment to infrequent cases of unstable clinical presentation in the two territories being refractory to medical therapy. In our experience, most neurologically symptomatic patients were treated with endovascular procedures, often with a simultaneous approach (Table 1).
The co-existence of severe atherosclerotic lesions in the carotid and coronary districts is a common combination of advanced atherosclerosis, and the frequency and severity of vessel involvement revealed in our series is similar to other historical controls20. CAD is a major determinant of survival in patients with revascularised COD and therefore myocardial revascularisation in these patients may offer relevant clinical benefits21. The treatment of the two vascular districts was safe in terms of MACCE in the short term in our series by either technique, but at the price of a higher incidence of AKI and bleeding. The long-term clinical assessment of these groups is warranted.
Hybrid revascularisation strategies probably permit treatment of difficult and critically ill patients and may represent a reasonable alternative for selected cases if performed by expert teams22. However, the hybrid approach is limited, in our experience, by a higher incidence of MACCE and bleeding complications that derive from the acute or unstable clinical presentation on one or both vascular territories, on the one hand, and on the other hand, as a consequence of performing surgery immediately after an endovascular procedure under intensive anticoagulant and anti-platelet regimens. A recent report on 101 patients treated with CAS and immediate CABG compared favourably to our results with a slightly lower incidence of stroke and less bleeding, underscoring the importance of optimising the management of anticoagulation and anti-platelet therapy22.
In summary, this first analysis of the FRIENDS collaboration put in evidence the feasibility and short-term safety of a multidisciplinary diagnostic and therapeutic model for the management of patients with complex vascular disease involving simultaneously the carotid and coronary circulation as applied in specialised centres dedicated to vascular care. Endovascular alternatives appear particularly suited in this context largely represented by fragile and critical patients that seem to benefit from the less invasive approach delivered by well indicated and cautiously performed transcatheter procedures. Also, surgical results are excellent.
Patients with multivascular atherosclerotic disease are often treated by different specialists, and due to the lack of clear evidence-based indications, they are frequently advised contradictory alternatives depending on the specialist which leads to different therapeutic decisions in each indivdual case. Cardiologists find themselves at the crossroad of this complex process, not only because of their attitude towards clinical medicine and their knowledge of circulatory physiopathology, but also because of their situation of working in a clinical division with a ward. In this situation they can confront the individual patients and their referring physicians who can then be appropriately informed about therapeutic options. This same situation occurs as well in intensive care units where complex patients can be treated in a comprehensive manner with the assistance of other specialists as needed. Nonetheless, their skills in vascular interventions add further capacity to their interaction with other interventional colleagues, with as a result much better coordination of diagnostic, preventive, and therapeutic strategies. This integrated approach should aim at providing the highest standards of care to these patients by offering them the best exercise of a global vascular approach and when needed, appropriate local vascular interventions.
The assessment of the long-term results of these patients is essential, and our group is committed in obtaining such information for future presentation.

