Abstract
Aims: The aim of this study was to compare the outcome of patients with a post-procedural tricuspid valve gradient (TVG) of >3 mmHg vs ≤3 mmHg after transcatheter edge-to-edge tricuspid valve repair (TTVR).
Methods and results: Between March 2016 and October 2018 we treated 145 patients with severe tricuspid regurgitation (TR) with TTVR by placing 2.2±0.7 clips per patient. Device success (TR reduction ≥1° to at least moderate) was achieved in 125 patients (86.2%). TTVR resulted in an elevated TVG >3 mmHg in 25 (17.2%) patients. Device success (84% vs 86.7%, p=0.9), number of clips implanted (2.3±0.7 vs 2.2±0.7, p=0.33), clinical improvement including NYHA class (III/IV 24% vs 28%, p=0.92) and increase in six-minute walking test at one month (67 m [IQR 5-103 m] vs 56 m [IQR 8-97 m], p=0.93), mortality (HR 1.07, 95% CI: 0.43-2.65, plogrank=0.88) and the combined endpoint mortality and hospitalisation for heart failure at one year (HR 1.07, 95% CI: 0.46-2.48, plogrank=0.88) were similar between patients with a TVG >3 mmHg versus patients with a TVG ≤3 mmHg.
Conclusions: A small cohort of patients demonstrated an elevated TVG higher than 3 mmHg at discharge. This elevation had no impact on clinical improvement, mortality or hospitalisation for heart failure.
Introduction
Severe tricuspid regurgitation (TR) causes right ventricular and tricuspid valve annular dilatation leading to right heart failure and is associated with poor outcomes1. Although tricuspid valve repair or replacement is recommended by European and American guidelines2,3, many patients are considered inoperable due to high morbidity and mortality risk. Transcatheter edge-to-edge tricuspid valve repair (TTVR) is a novel treatment approach in heart failure patients with severe TR at prohibitive surgical risk4,5. Effective TR reduction and clinical improvement following TTVR with edge-to-edge devices has been demonstrated, including improvement in symptoms and in functional capacity6,7. An edge-to-edge repair technique of atrioventricular valves narrows the regurgitant orifice by approximating the leaflets and reducing the valve diameter. Both mechanisms potentially increase transvalvular inflow gradient. It has been shown in a single-centre study that patients with a post-procedural mitral valve gradient >5 mmHg after transcatheter edge-to-edge mitral valve repair have a poorer long-term outcome, including an increased all-cause mortality8. Indeed, the pressure and flow conditions of the mitral and tricuspid valve are different. The mitral valve consists of only two leaflets and is smaller9 than the tricuspid valve which physically leads to a higher inflow velocity and higher pressure gradient compared to the tricuspid valve. In contrast, the tricuspid valve (embedded within the right-sided low-pressure circulation) contains three, sometimes four, leaflets and is considerably larger10 than the mitral valve which leads to a lower inflow velocity and subsequently a lower pressure gradient compared to the mitral valve. An arbitrarily defined tricuspid valve gradient (TVG) of ≤3 mmHg has been used in TTVR procedures by us and others in the past4 due to the lack of an evidence-based interventional strategy which defines a TVG as acceptable after TTVR.
The clinical relevance of a post-procedural elevated TVG on clinical outcome is unknown. Hence, the aim of this study was to investigate TVG after TTVR over time and compare patient characteristics and outcome of patients with a TVG at discharge of >3 mmHg versus ≤3 mmHg.
Methods
STUDY POPULATION AND DESIGN
All patients who were treated in an off-label and compassionate use setting with TTVR between March 2016 and October 2018 at the University Hospital of Munich were included in this analysis. All patients were symptomatic with signs of right-sided heart failure. Patients were deemed at prohibitive surgical risk by an interdisciplinary Heart Team and provided written informed consent. The local ethics committees approved the data analysis of patients treated with TTVR.
PROCEDURE
The transcatheter edge-to-edge repair system (MitraClip®; Abbott Vascular, Santa Clara, CA, USA) was used as described previously6. Image guidance was provided by two- and three-dimensional transoesophageal and transthoracic echocardiography (TTE) with additional fluoroscopy11,12. Careful assessment of TVG was performed after every clip implantation with the aim of maintaining a TVG ≤3 mmHg4.
OUTCOMES
The primary outcome of this study was death and hospitalisation for heart failure in the follow-up period. Further information is provided in Supplementary Appendix 1.
ECHOCARDIOGRAPHY
TTE assessment of TVG was performed preprocedurally, at discharge, and after 1, 6, and 12 months. We followed current recommendations for the assessment of native valve regurgitation, chamber quantification and assessment of the right heart13,14,15,16. Evaluation of TR comprised vena contracta width (biplane), TR volume and effective regurgitant orifice area according to the proximal isovelocity surface area method. The synthesis of all parameters led to a grading of TR into four grades: mild (1+), moderate (2+), severe (3+) and massive/torrential (4+). We measured the diastolic mean TVG and the systolic right ventricular tricuspid pressure gradient (RVTG) using the simplified Bernoulli equation. Patients were advised to remain in the resting expiratory position and gradients/velocity time integral (VTI) signals were measured (in all patients) in transthoracic examinations to secure comparable conditions, usually applying the RV focused view (as recommended by guidelines on echocardiographic assessment for valvular stenosis17). The septal-lateral diameter of the TV was measured in the RV focused view.
STATISTICAL ANALYSIS
Information on statistics is provided in Supplementary Appendix 1.
Results
BASELINE CHARACTERISTICS
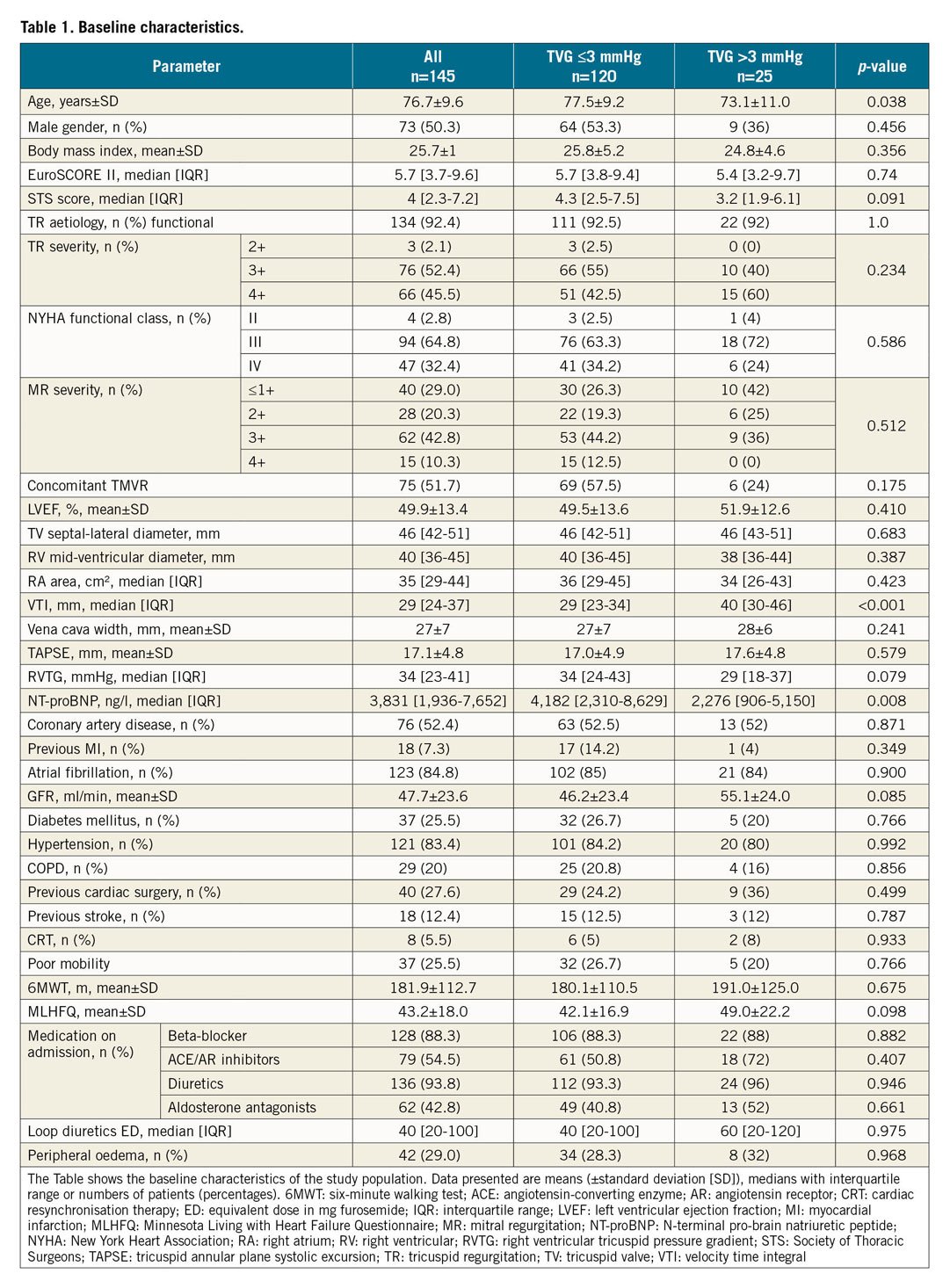
Between March 2016 and October 2018, we treated 145 consecutive patients with severe TR with TTVR. The baseline characteristics of all patients are shown in Table 1.
PROCEDURAL OUTCOME
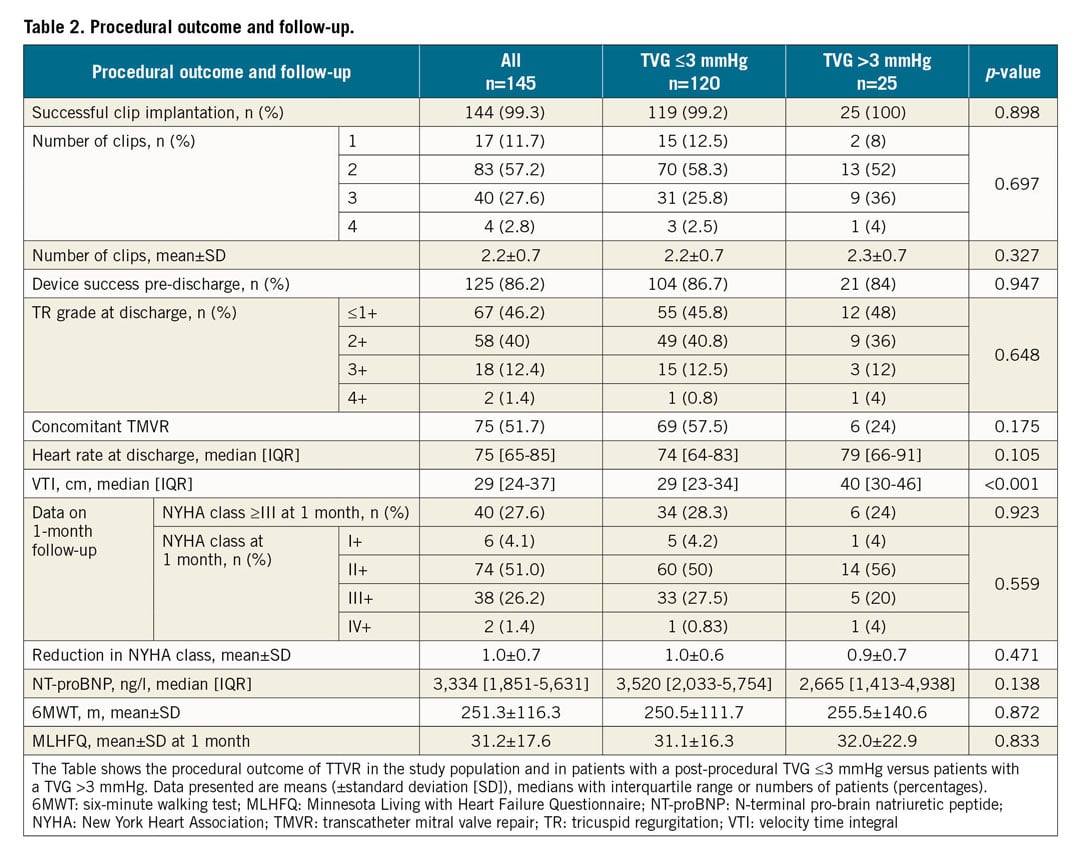
Patients were treated with TTVR for isolated severe TR (70 patients) or in combination with mitral valve repair for concomitant severe MR and TR with significant annulus dilatation (75 patients). Device success, which was defined as TR reduction ≥1° to at least moderate, was achieved in 125 patients (86.2%) (Figure 1, Supplementary Figure 1). Clip detachment occurred in four patients. Of these, one clip detachment occurred during the procedure, two detachments occurred within one day and one was noticed during echocardiographic examination at one-month follow-up. Persistent iatrogenic atrial septum defect was detected in 22 patients (29%) at follow-up examinations and the residual mitral valve inflow gradient was 3 mmHg (2-4) in patients receiving TTVR and mitral valve repair concomitantly. The procedural outcome of all patients is shown in Table 2. The median time interval from procedure to pre-discharge echo was 3 (2-5) days. The median follow-up time of patients was 6 (2-11) months.
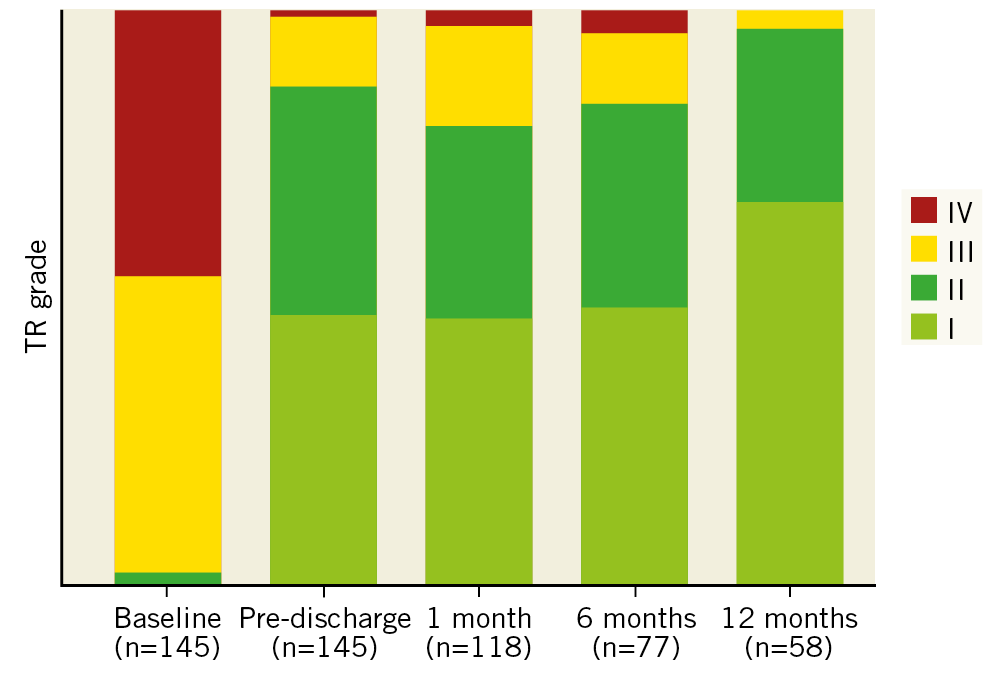
Figure 1. TR grade at baseline and follow-up echocardiographic examinations in patients after TTVR.
The median baseline TVG was 1 mmHg (1.0-1.4 mmHg). The TVG at discharge increased to 2 mmHg (1.6-3.0 mmHg), p<0.001, and remained stable at six-month (2.0 mmHg [1.0-2.5 mmHg], p=0.11) and 12-month (2 mmHg [1.0-2.0 mmHg], p=0.78) follow-up (Figure 2A, Supplementary Figure 2A). Of these, twenty-five patients showed an elevated TVG >3 mmHg at discharge. The TVG at 30 days and six months remained significantly higher in the TVG >3 mmHg group compared to the TVG ≤3 mmHg group (p=0.0035 at 30 days and p=0.018 at six months). In patients with a pre-discharge TVG >3 mmHg, at least 10 patients (45%, measured in 22 patients) presented with an elevated TVG ≥3 mmHg at 30 days, 5 patients (56%, measured in 9 patients) at six months and 2 patients (100%, measured in 2 patients) at 12 months (Figure 2B, Figure 2C, Supplementary Figure 2B, Supplementary Figure 2C).
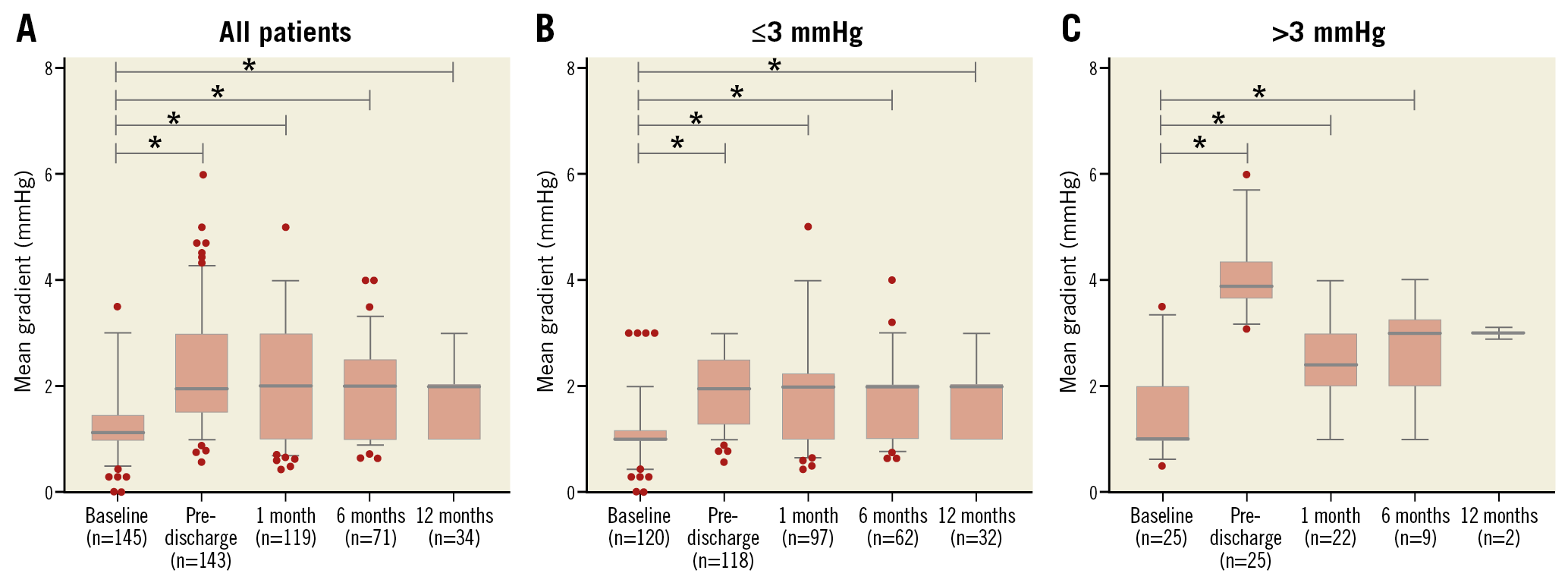
Figure 2. Changes in tricuspid valve gradient over time. Changes in all patients (A) and according to study group (B: TVG ≤3 mmHg, C: TVG >3 mmHg). Boxes represent interquartile range; whisker represents 5th and 95th percentile, bold dark line represents median. Asterisks represent significant differences with a p-value <0.05.
CHARACTERISTICS AND OUTCOME OF PATIENTS WITH A POST-PROCEDURAL TVG >3 mmHg VERSUS ≤3 mmHg
Patients with a TVG >3 mmHg were younger (73.1±11.0 vs 77.5±9.2 years, p=0.038) and presented with lower levels of NT-proBNP at baseline (2,276 ng/l [906-5,150 ng/l] vs 4,182 ng/l [2,310-8,629 ng/l], p=0.008) compared to patients with a TVG ≤3 mmHg. Patients with a TVG >3 mmHg – albeit not significant – were less frequently male (36% vs 53%), had a better glomerular filtration rate (55 ml/min vs 46 ml/min) and more often underwent cardiac surgery (36% vs 24%). All other baseline characteristics are shown in Table 1. The echocardiographic RV parameters including septal-lateral annular end-diastolic diameter (46 mm [43-51 mm] vs 46 mm [42-51 mm], p=0.683) and tricuspid annular plane systolic excursion (TAPSE) (17.6±4.8 mm vs 17.0±4.9 mm, p=0.58) did not differ between the groups, whereas RVTG (29 mmHg [18-37 mmHg] vs 34 mmHg [24-43 mmHg], p=0.08) was absolutely lower in patients with a TVG >3 mmHg.
Device success (TR reduction of ≥1 grade to at least moderate in 84% vs 86.7%, p=0.9) and number of clips implanted (2.3±0.7 vs 2.2±0.7, p=0.33) were similar between the groups. At one-month follow-up, there was no difference in NYHA class (Table 2). More information on patients undergoing concomitant TMVR is shown in Supplementary Appendix 2 and Supplementary Figure 3. Both groups showed a similar increase in 6-minute walking distance (6MWD) (67 m [5-103 m] vs 56 m [8-97 m], p=0.93). The improvement of quality of life (Minnesota Living with Heart Failure Questionnaire [MLHFQ]) was more pronounced in patients with a TVG >3 mmHg versus ≤3 mmHg (17.8±16.7 vs 9.9±17.0, p=0.08) (Figure 3). Only two patients showed a TVG in excess of 5 mmHg with a heart rate of 111/min and 83/min, respectively, at the determination of TVG. Of these, the first patient was alive nine months after the procedure and the second patient who was treated with TTVR was alive at one-month follow-up in very good physical condition. The frequency of the triple-orifice technique (versus the bicuspidalisation technique18) was significantly higher in patients with a TVG >3 mmHg (p<0.001). Moreover, the median TVG at discharge was significantly higher in patients undergoing a bicuspidalisation technique (2.0 [1.5-2.9] mmHg vs 2.0 [2.0-3.4] mmHg, p=0.04) in the whole population.
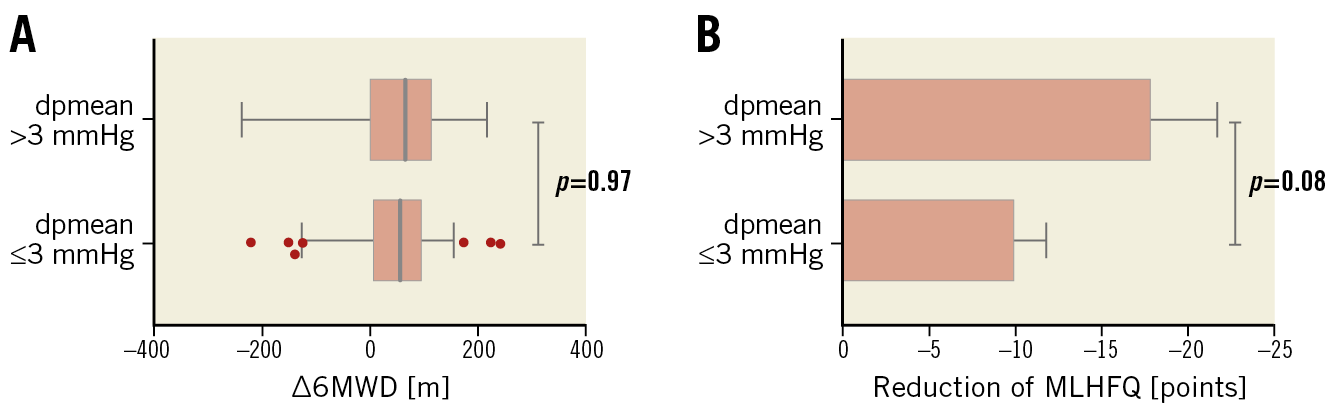
Figure 3. Improvement in 6MWD and increase in quality of life at one month after TTVR with TVG at discharge of ≤3 mmHg versus >3 mmHg. Improvement in 6MWD (A) and increase in quality of life according to the MLHFQ (B). Boxes represent interquartile range; whisker represents 5th and 95th percentile, bold dark line represents median in panel A; whisker represents standard deviation in panel B. 6MWD: six-minute walking distance; dpmean: mean pressure gradient (d: delta, ∆); MLHFQ: Minnesota Living with Heart Failure Questionnaire
The clinical endpoints one-year mortality (HR 1.07, 95% CI: 0.43-2.65; plogrank=0.88) (Figure 4) and the combined endpoint mortality and hospitalisation for heart failure at one year (HR 1.07, 95% CI: 0.46-2.48; plogrank=0.88) (Figure 5) did not differ between patients with a TVG >3 mmHg versus patients with a TVG ≤3 mmHg.
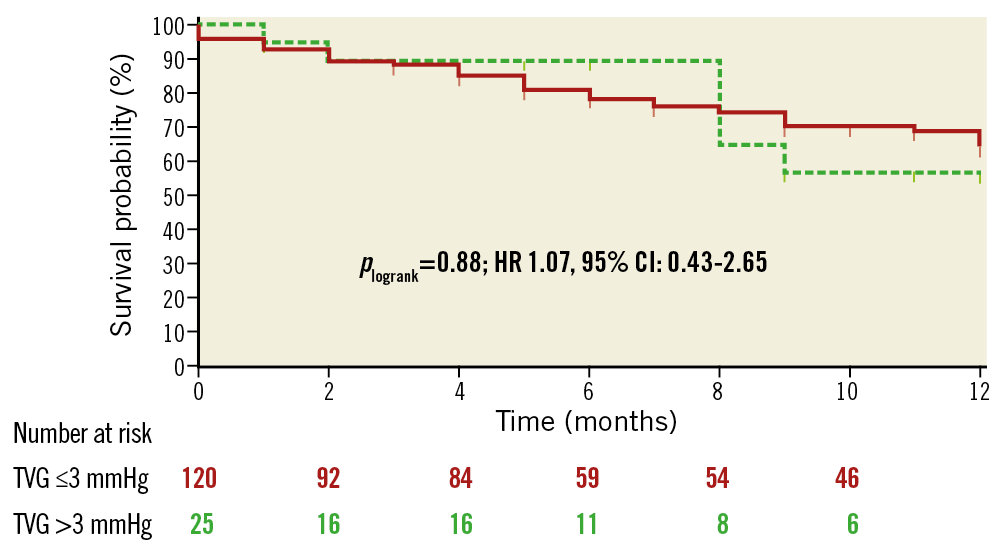
Figure 4. Kaplan-Meier one-year survival estimates of patients after TTVR with post-procedural TVG ≤3 mmHg versus >3 mmHg. Vertical markings within survival curves indicate last live contact.
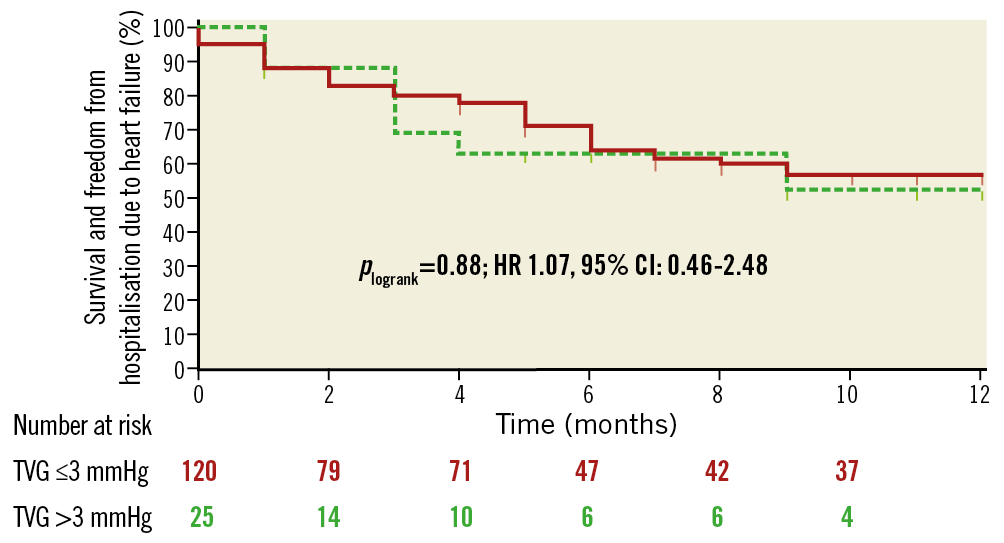
Figure 5. One-year estimates of the combined endpoint death and admission due to heart failure of patients after TTVR with post-procedural TVG ≤3 mmHg versus >3 mmHg. Vertical markings within survival curves indicate last live contact.
Discussion
This prospective observational study investigated the mean TVG after TTVR using the edge-to-edge repair technique and compared patient characteristics and outcomes of patients with a TVG at discharge of >3 mmHg versus ≤3 mmHg. The main findings at long-term follow-up are, that 1) the mean TVG increased slightly after TTVR from 1 mmHg to 2 mmHg and remained stable up to six and 12 months, 2) a small proportion of patients presented with an elevated TVG >3 mmHg, 3) improvement in NYHA class and 6MWD at one month after the procedure was similar between groups, and 4) this elevation in TVG did not result in an increase either in mortality or in the combined endpoint of mortality and hospitalisation for heart failure.
International guidelines consider mitral or tricuspid valve inflow gradients in excess of 5 mmHg as stenosis2,3. In patients undergoing transcatheter mitral valve repair, it was demonstrated that a mitral valve gradient above 5 mmHg – which was reported in up to 25% of patients – is associated with an increase in a combination of all-cause mortality, left ventricular assist device implantation, mitral valve replacement, and recurrent procedure at long-term follow-up8. There are no data in this regard concerning TTVR. Edge-to-edge valve repair increases ventricular inflow valve gradients, but data on the clinical tolerability of increased diastolic gradients in the right-sided low-pressure circulation and its impact on outcome are unknown. In this regard, our analysis on TTVR shows that a TVG in excess of 5 mmHg is extremely rare and that an elevated TVG in excess of 3 mmHg is not associated with impaired clinical improvement or prognosis. These findings might be explained by the difference in pressure and flow conditions between both atrioventricular valves. The bicuspid mitral valve – embedded within the left high-pressure system– is smaller9 than the tricuspid valve which physically leads to a higher inflow velocity, higher pressure gradient and increased susceptibility for mitral stenosis after an edge-to-edge repair. In contrast, the tricuspid valve – embedded within the right-sided low-pressure circulation – contains three, sometimes four leaflets and is larger10 than the mitral valve, which leads to a lower inflow velocity and subsequently lower pressure gradient compared to the mitral valve. Although more clips are usually needed to reduce TR (2.2±0.7 tricuspid clips per patient in our cohort vs 1.4±0.6 mitral clips per patient in the German transcatheter mitral valve interventions registry [TRAMI], n=828 patients19) due to larger valve area and the complex tricuspid anatomy, this fact did not lead to a higher inflow gradient in our analysis.
There is no evidence-based interventional strategy which defines a TVG which is acceptable after TTVR. An arbitrarily defined TVG of ≤3 mmHg has been used in TTVR procedures and studies by us and others in the past4. Here we show that an elevated TVG in excess of 3 mmHg is not associated with an increase in clinical endpoints or a deterioration of functional capacity when compared to all other patients. In the study of Neuss et al, Kaplan-Meier curves after TMVR separated from the beginning of follow-up, whereas Kaplan-Meier curves in our study after TTVR did not separate up to one year. Our strategy of carefully monitoring the TVG during TTVR resulted in a small cohort of patients with a TVG >3 mmHg, with only about 1% of treated patients with a TVG >5 mmHg. Hence, in contrast to transcatheter mitral valve repair, a clinically relevant tricuspid stenosis after TTVR did not occur.
Limitations
This was a prospective, observational analysis at a single centre investigating a rather small number of patients in both groups; however, it represents one of the largest patient cohorts undergoing TTVR. Echocardiographic parameters such as effective regurgitant orifice area and pressure half-time were not available in all patients. Hence, our study focused on the significance of an isolated Doppler parameter rather than tricuspid valve stenosis which would require the integration of these multiple echocardiographic parameters. The transvalvular gradient cut-off of 3 mmHg was arbitrarily selected but has been used in TTVR procedures by us and others in the past. This analysis is based on a limited follow-up due to the early nature of the TTVR field.
Conclusions
TTVR resulted in a small increase in the TVG, which remained stable at follow-up. A small cohort of patients showed an elevated TVG >3 mmHg after the procedure. This elevation had no impact on the clinical improvement after TTVR or on mortality and the need for hospitalisation for heart failure.
|
Impact on daily practice There is no evidence-based interventional strategy which defines a TVG which is acceptable after TTVR; instead, an arbitrarily defined TVG of ≤3 mmHg has been used in TTVR procedures by us and others in the past. Only a small cohort of patients showed an elevated TVG >3 mmHg after the procedure which did not have an impact on clinical improvement after TTVR or on mortality and the need for hospitalisation for heart failure. Thus, an elevated TVG after TTVR might be an overestimated problem in the right-sided low-pressure circulation. |
Conflict of interest statement
M. Orban has received speaker honoraria from Sedana Medical and AstraZeneca. D. Braun has received speaker honoraria from Abbott Vascular. N. Karam has received consultant fees from Abbott Vascular. M. Nabauer has received speaker honoraria from Abbott Vascular. J. Hausleiter has received speaker honoraria and research support from Abbott Vascular and Edwards Lifesciences. The other authors have no conflicts of interest to declare.