Abstract
Background: Mitral valve repair may lead to alterations of tricuspid regurgitation (TR).
Aims: We aimed to investigate alterations, predictors and prognostic relevance of TR evolution in a large-scale multicentre population of patients undergoing transcatheter mitral valve repair (TMVR) via the MitraClip.
Methods: In total, we included 531 TMVR patients with at least one available follow-up echocardiography. TR improvement was defined as a TR ≥II at baseline, which showed a decline of at least one TR categorisation.
Results: Distribution of preprocedural TR severity was TR 0/I 41% (220/531), TR II 39% (209/531) and TR ≥III 19% (102/531), respectively. Follow-up echocardiography was at 308±187 days. TR severity improved to TR 0/I 49% (259/531), TR II 35% (183/531) and TR III 17% (89/531), p=0.003. Out of 311 patients with TR ≥II at baseline, 41% (127/311) showed TR improvement. Atrial fibrillation (AF), residual mitral regurgitation ≥II (rMR) and tricuspid annular diameter (TAD) remained variables which prevented TR improvement (odds ratio 0.49 [0.29-0.84], 0.47 [0.27-0.81] and 0.97 [0.93-0.997], respectively). TR improvement was associated with better event-free survival regarding post-procedural heart failure hospitalisation (HHF) (hazard ratio 0.6 [0.38-0.94]). The main changes of TR severity occurred within 3 months post TMVR (p=0.006), while there were only minor TR changes between 3 and 12 months of follow-up (p=0.813).
Conclusions: TR improvement was frequent after TMVR. Predictors preventing TR improvement were AF, post-procedural rMR, and TAD. Furthermore, TR improvement was an early phenomenon occurring primarily within the first three months post TMVR and served as a suitable marker of reduced HHF.
Introduction
Transcatheter mitral valve repair (TMVR) represents a minimally invasive therapeutic option in selected patients with clinically relevant mitral regurgitation (MR) and increased surgical risk1,2. Among different TMVR techniques and devices, the edge-to-edge repair via MitraClip® (Abbott Vascular, Santa Clara, CA, USA) implantation is of particular interest, representing a safe procedure with a high technical success rate3.
Tricuspid regurgitation (TR) is frequently caused by left-sided heart disease4. MR can lead to pulmonary hypertension and right ventricular afterload which then results in leaflet malcoaptation and TR5. Hence, TR is a frequent comorbidity in patients with MR6. Consecutively, MR reduction via TMVR might lead to an improvement of concomitant TR; however, there is a lack of large-scale data regarding this issue7,8,9,10 which is of special interest against the background of emerging transcatheter tricuspid valve repair (TTVR) procedures11,12. Predictors of TR improvement could help in the decision making concerning concurrent transcatheter mitral and tricuspid repair.
In the present large-scale multicentre study, we investigated time-dependent alterations of TR in patients after TMVR, and assessed predictors preventing TR improvement. Moreover, we aimed to calculate the cut-off value of tricuspid annular diameter (TAD) associated with low TR improvement post TMVR. Lastly, we analysed whether TR improvement and tricuspid annular dilatation correlates with rates of post-procedural heart failure hospitalisation (HHF).
Methods
STUDY COHORT
In total, we included data of 531 patients with available baseline and follow-up echocardiography who underwent TMVR in the Heart Failure Network Rhineland (University Hospitals Bonn, Cologne, Düsseldorf) from August 2010 to September 2018, and received at least one MitraClip. All procedures were performed with the MitraClip system. Patients agreed to participate in our registry which was approved by the ethics committee of each individual centre in accordance with the Declaration of Helsinki. Echocardiographic data were evaluated according to the institutional practice of the treatment centre. MR severity was categorised into three grades as I (mild), II (moderate), and III (severe) according to current guidelines13. Assessment of TR severity was conducted as recommended by current guidelines14, and TR severity was categorised as none/mild (0/I) versus moderate (II) versus severe (≥III) TR.
FOLLOW-UP DATA
After the MitraClip procedure, follow-up was monitored at regular clinic visits, and by telephone calls to the referring cardiologist, the general practitioner or the patients themselves. As clinical outcome parameter we determined the first readmission for heart failure within two-year follow-up after TMVR (mean available follow-up was 766±562 days). For the assessment of TR evolution after MitraClip implantation in the mitral valve, 485 echocardiographic controls were investigated at 3-month follow-up and 392 echocardiographic controls were evaluated at 12-month follow-up. Follow-up echocardiography was defined as the 12-month echocardiography and supplanted by the 3-month in patients with missing 12-month control. TR improvement was defined as a TR ≥II at baseline, which showed a decline of TR categorisation (e.g., moderate TR to none/mild TR).
STATISTICAL ANALYSIS
Normal distribution of variables was tested with the use of the Kolmogorov-Smirnov test. For comparison of two groups and continuous variables, the Student’s t-test, Mann-Whitney U test, and Wilcoxon test were used. When assessing more than two groups, ANOVA or the Kruskal-Wallis test was performed for continuous variables. For categorical variables, the chi-square test was performed. The McNemar test was used for paired variables. Event-free survival rates and statistical differences were obtained by the Kaplan-Meier method and the log-rank test. Cox regression analysis was used to assess the association between parameters and event-free survival. Logistic regression analysis was performed to identify variables which were associated with TR improvement. For the multivariable analysis, we included parameters which showed a difference with p<0.100 in the baseline characteristics and had a significant predictive value in the univariable test. Best cut-off value was calculated via the receiver operating characteristic with the highest area under the curve. A p-value of <0.05 was considered to be statistically significant. Statistical analysis was performed with SPSS software, Version 24.0.0.0 (IBM Corp., Armonk, NY, USA).
Results
STUDY POPULATION
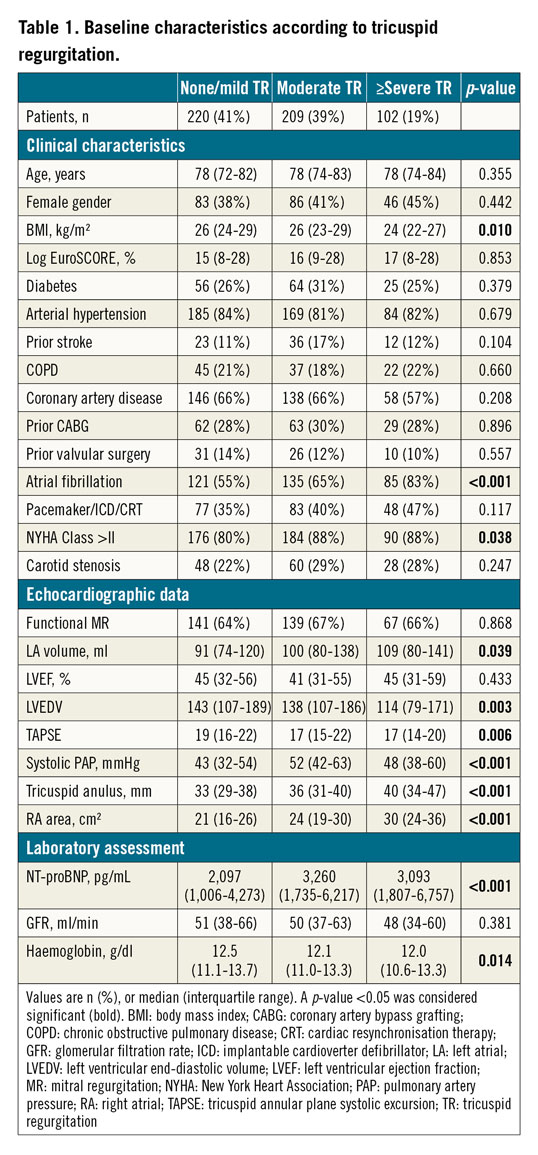
A total of 531 patients who underwent TMVR with available follow-up echocardiography were included in the final analysis. Mean time of the follow-up echocardiography was 308±187 days. Mean age of the patient cohort was 76.7±9.0 years; 215 (41%) were female. The patient cohort had high surgical risk with an increased median logistic EuroSCORE of 16% (9-29%). Aetiology of MR was primary in 184 (35%) patients and secondary in 347 (65%) patients. Post-procedural residual MR (rMR) ≥II was prevalent in 32% (171/525) of patients, while post-procedural MR >II was present in 6% (32/525) of patients. Mean number of implanted clips was 1.47±0.6.
TRICUSPID REGURGITATION DYNAMICS AFTER TMVR
At baseline, 41% (220/531) of patients had TR 0/I, while 39% (209/531) of patients had TR II, and 19% (102/531) of patients had TR ≥III (Figure 1A). Baseline patient characteristics according to TR severity are summarised in Table 1. Assessment of follow-up echocardiography revealed a significant change in TR distribution after TMVR – 49% (259/531), 35% (183/531) and 17% (89/531) of patients with TR 0/I, II and ≥III, respectively (p=0.003) (Figure 1A). In patients with TR 0/I at baseline, 24% (53/220) and 4% (9/220) of patients showed a TR worsening to TR II and TR ≥III, respectively (Figure 1B). In patients with TR II at baseline, 42% (88/209) of patients had a TR improvement to TR 0/I, while in 14% (30/209) of cases TR deteriorated to TR ≥III (Figure 1C). Patients with TR ≥III at baseline had a TR improvement to TR 0/I and TR II in 38% (39/102) and 13% (13/102) of cases, respectively (Figure 1D).
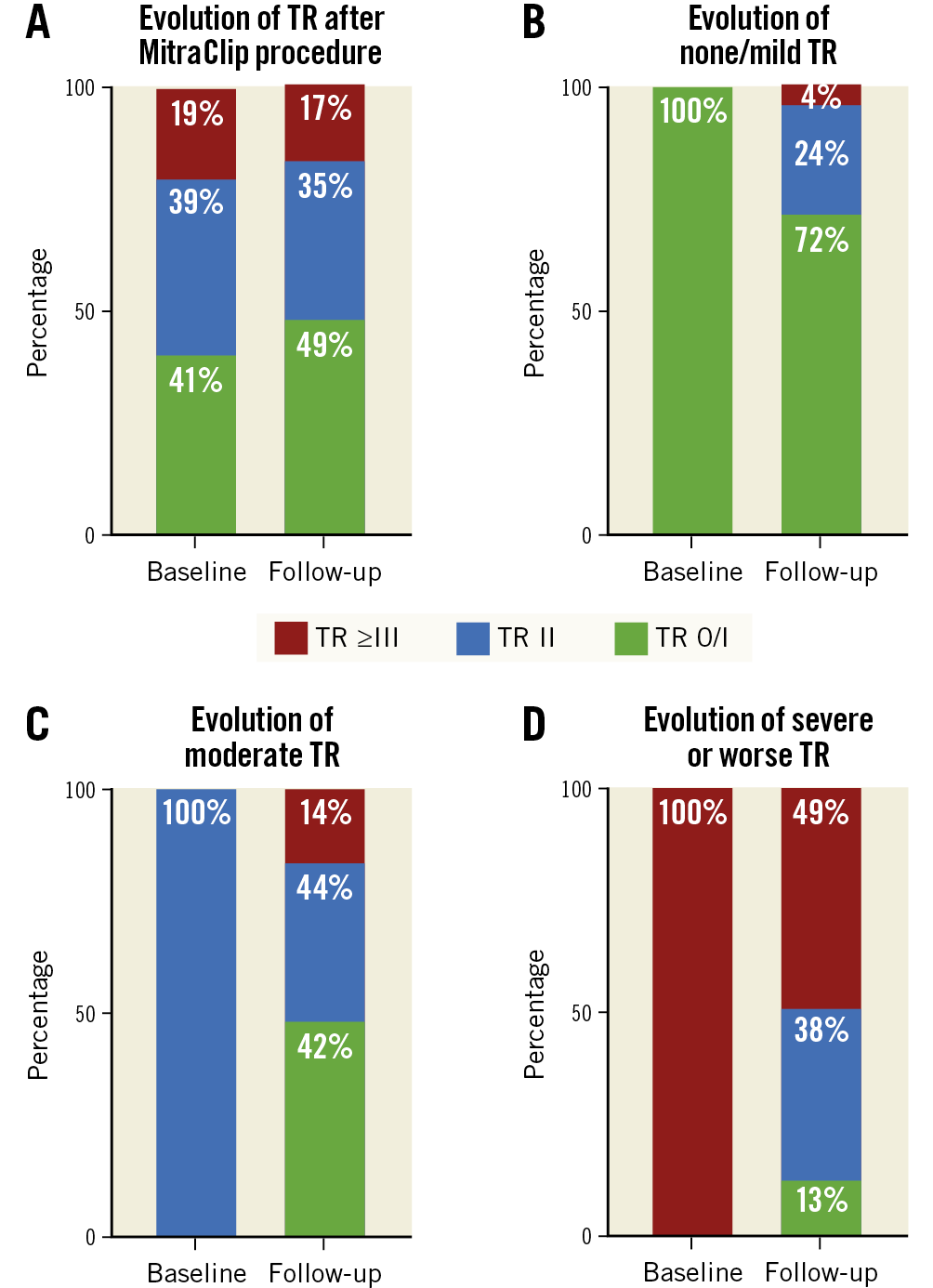
Figure 1. Evolution of tricuspid regurgitation after MitraClip procedure. A) The percentage of tricuspid regurgitation (TR) severity changed significantly after transcatheter mitral valve repair (TMVR) (p=0.003). B) - D) Changes of TR after TMVR are shown for each of the TR groups separately.
TR ALTERATION IS AN EARLY PHENOMENON
Next, we focused on the timing of temporal TR changes post TMVR procedure. For this analysis we included only patients with available 3-month and 12-month echocardiography (n=346), hence 165 patients with one missing follow-up echocardiography were excluded. Comparing preprocedural and 3-month data, proportions of TR 0/I, II, and ≥III varied significantly (41% [143/346] vs 41% [141/346] vs 18% [62/346], and 49% [171/346] vs 35% [122/346] vs 15% [53/346], respectively; p=0.006), while the TR distributions did not change comparing 3-month and 12-month data (49% [171/346] vs 35% [122/346] vs 15% [53/346], and 51% [176/346] vs 33% [115/346] vs 16% [55/346], respectively; p=0.813) (Supplementary Figure 1). Overall, 91% (485/531) of patients had a 3-month and 74% (392/531) of patients had a 12-month available echocardiography. The evolution of TR in different subgroups according to available echocardiography is summarised in Supplementary Table 1.
TRICUSPID ANNULUS DIAMETER (TAD) AFTER TMVR
Follow-up TAD was available in 441 of 531 patients. In total, there was no significant change in median TAD comparing baseline and follow-up (35.9±7.5 vs 35.9±7.5 mm; p=0.949). Moreover, the median difference in tricuspid diameter at baseline and follow-up was 0 mm (-3.5 mm to 4 mm). However, in 49% (218/441) of cases TAD declined after TMVR. TR improvement tended to be more frequent in patients with a decline in TAD (58% vs 42%, p=0.052).
ATRIAL FIBRILLATION (AF), RESIDUAL MR (rMR) AND TAD PREVENT TR IMPROVEMENT
Out of 311 patients with moderate or worse TR, 41% (127/311) revealed a TR improvement at follow-up. Baseline characteristics according to TR improvement are shown in Supplementary Table 2. Patients with TR improvement had a lower median TAD (35 mm [31-40 mm] vs 37 mm [33-43 mm]; p=0.013), lower median NT-proBNP (2,991 pg/mL [1,868-6,385 pg/mL] vs 3,302 pg/mL [1,776-6,461 pg/mL]; p<0.001), and a lower prevalence of AF (60% vs 78%; p<0.001). Moreover, rMR ≥II at discharge was more frequent in patients without TR improvement (39% vs 24%; p=0.005). Parameters which showed a difference with a p-value <0.100 were tested for their predictive ability regarding TR improvement by logistic regression analysis (Table 2). In the multivariable analysis, AF (odds ratio [OR] 0.49, 95% confidence interval [CI]: 0.29-0.84; p=0.009), rMR ≥II at discharge (OR 0.47, 95% CI: 0.27-0.81; p=0.007) and TAD (OR 0.97, 95% CI: 0.93-0.997, per 1 mm increase; p=0.032) remained predictive parameters associated with a reduced probability of TR improvement. Missing values were excluded from the multivariable analysis, which led to the inclusion of 289/311 (93%) patients. The best predictive TAD cut-off value was for a diameter ≥34 mm. Using tricuspid annular dilatation (TAD ≥34 mm) instead of TAD, univariable regression revealed an OR of 0.40 (95% CI: 0.24-0.68; p=0.001) regarding TR improvement. Repeating multivariable analysis with tricuspid annular dilatation instead of TAD showed an OR of 0.44 (95% CI: 0.25-0.76; p=0.003) (Table 2). Results for the other parameters were similar to the first multivariable model. At baseline, the subgroup of TR ≥II and a TAD ≥34 mm included 189 patients. Of these, 35% (66/189) of patients showed TR improvement of at least one grade during follow-up. However, the majority of 75% (141/189) of patients still had a TR ≥II (84 patients with TR II, 57 patients with TR III), retaining a possible TR treatment indication. In contrast, the subgroup of TR ≥II with a TAD <34 mm included 101 patients. Here, more than half (exactly 54% [54/101] of patients) had a TR improvement at follow-up, with 51/101 (50%) still having a TR ≥II at follow-up (36/101 patients with TR II, 15 patients with TR III) (Figure 2).
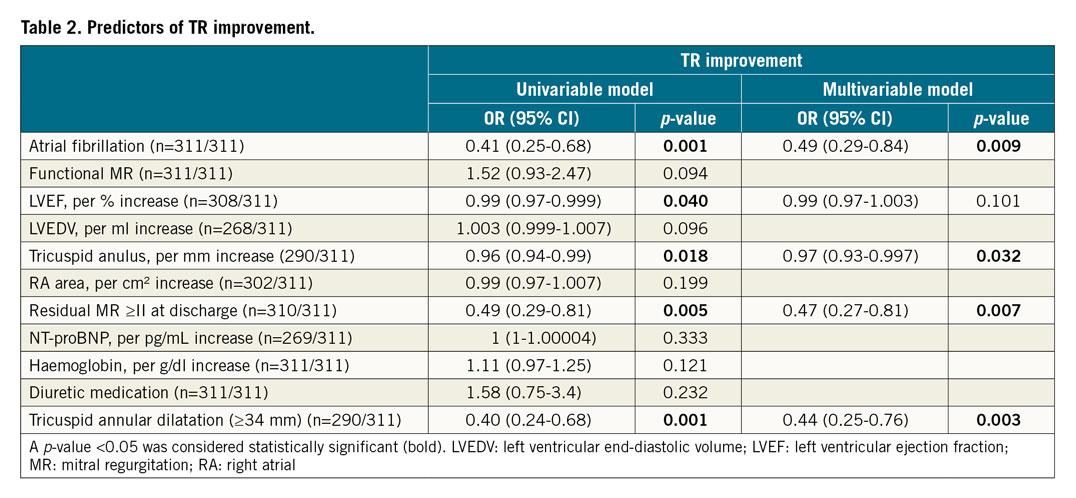
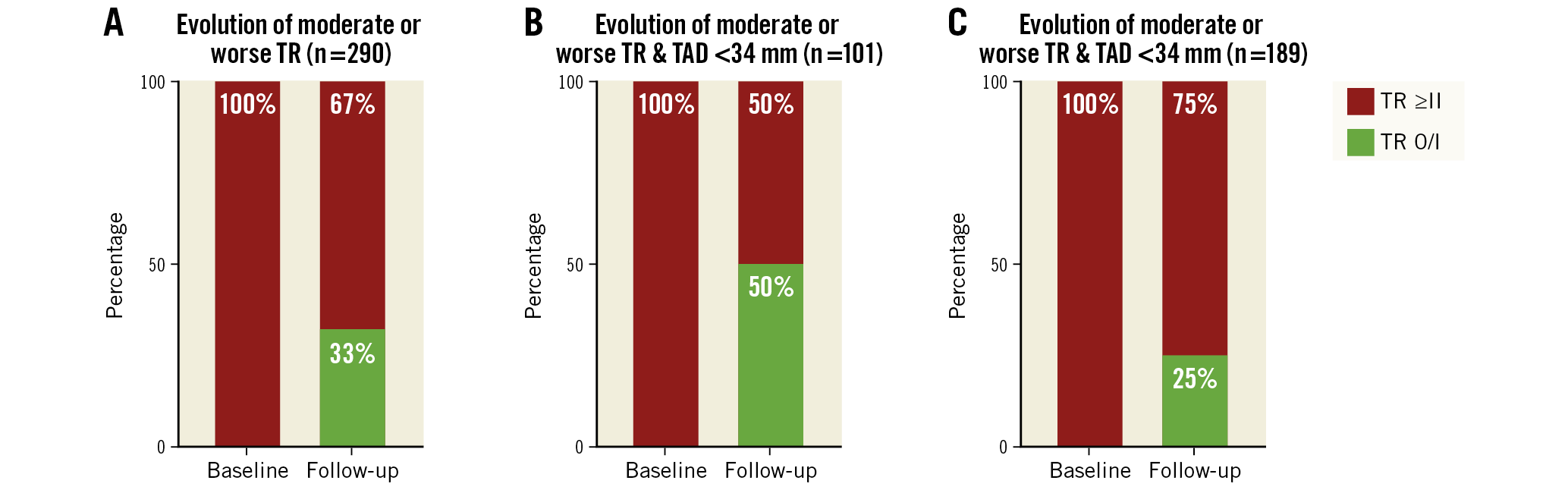
Figure 2. Evolution of moderate or worse tricuspid regurgitation (TR) characterised by differences in tricuspid annular diameter (TAD). In the subgroup analysis of patients with TR ≥II, persistent TR ≥II remained in 67% of patients (A) after TMVR. Characterised by preprocedural TAD <34 mm (B) versus ≥34 mm (C), persistent TR ≥II distribution was 25% versus 50%, respectively.
Analysis of heart failure medication for patients with available 3-month data (n=441) showed that, comparing baseline and 3-month data, medication with a beta-blocker (88% vs 91%; p=0.044) and diuretics (88% vs 93%; p=0.003) increased. Comparing the frequencies of these medications at 3 and 12 months did not show significant changes (n=328). Sub-analyses of changes in medication and daily doses are summarised in Supplementary Table 3.
HHF AFTER TMVR
Including patients with TR ≥II at baseline, Kaplan-Meier curve analysis and the log-rank test showed that TR improvement was associated with a lower rate of HHF (27% [33/124] vs 37% [68/183], log-rank test p=0.042) (Figure 3A). Multivariable Cox regression analysis revealed that TR improvement had a hazard ratio (HR) of 0.6 (95% CI: 0.38-0.94; p=0.025) regarding readmission for heart failure after TMVR (Supplementary Table 4). Moreover, patients with a tricuspid annular dilatation (defined as a tricuspid diameter ≥34 mm) at follow-up had a significantly higher rate of HHF (37% [100/270] vs 23% [41/177]; log-rank test p=0.001) (Figure 3B). Supplementary Table 5 summarises the baseline characteristics according to the presence of tricuspid annular dilatation at follow-up. Accordingly, parameters were tested in the univariable and multivariable Cox regression analysis (Supplementary Table 6), which revealed that a tricuspid annular dilatation at follow-up was associated with a 56% increased hazard (95% CI: 6-229%; p=0.023) for an HHF after TMVR.
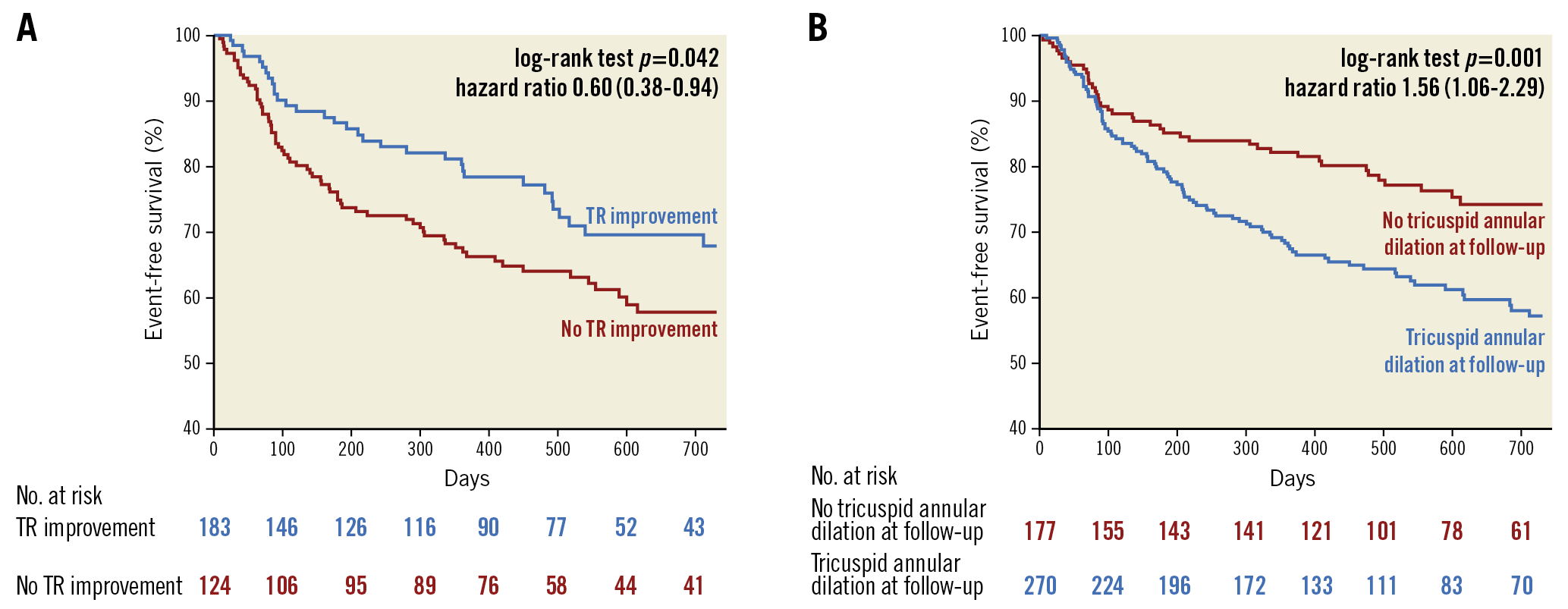
Figure 3. Association of TR improvement and tricuspid annular dilatation with cardiac hospitalisation. A) Patients without tricuspid regurgitation (TR) improvement had lower rates of event-free survival in terms of hospitalisation for heart failure. B) Tricuspid annular dilatation at follow-up was also associated with heart failure hospitalisation.
Discussion
In the present study, we investigated the post-procedural alterations of TR as well as predictors preventing TR improvement in patients undergoing TMVR with the MitraClip system. In this large-scale multicentre cohort, TR distribution changed significantly in patients after TMVR (p=0.003). Moreover, our results indicate that TR alterations post TMVR are an early phenomenon within the first 3 months, while there were no significant TR alterations between 3 and 12 months. Improvement of TR was observed in approximately half of the patients with moderate or worse TR at baseline. Moreover, rates of post-procedural HHF were lower in patients who showed TR improvement post TMVR. Of note, TAD served as one of three sensitive markers associated with reduced incidence of TR improvement in univariable and multivariable analysis. Therefore, TAD at baseline might be a crucial new marker helpful in terms of simultaneous transcatheter mitral and tricuspid valve repair versus TMVR-first and re-evaluate TR during follow-up. A 1 mm increase in TAD was associated with a 3% reduced probability of TR improvement. Moreover, tricuspid annular dilatation (≥34 mm) had a 0.44-fold (95% CI: 0.25-0.76) chance of TR improvement. Overall, the median TAD did not change during follow-up. Lastly, TR improvement and TAD (particularly <34 mm) at follow-up were markers associated with lower rates of post-procedural HHF.
TRICUSPID REGURGITATION ALTERATIONS AFTER TMVR
Prior studies regarding this topic showed that TR has a predictive value regarding survival rates after TMVR7,10,15,16, countering the idea of TR being a silent bystander. Ultimately, improvement of TR in this patient cohort represents a goal worth aiming for. Changes of TR grade were quite frequent. The proportion of none/mild TR increased, while the proportion of moderate or worse TR decreased, indicating an overall beneficial impact of TMVR on TR evolution. Medical treatment of TR involves diuretics which decrease volume overload. In our extensive analysis of heart failure medication, there was a clinically mild but statistically significant increase in diuretics with 91% to 96% or 88% to 95% at baseline and three months of follow-up within the group of TR II or no TR improvement, respectively. Therefore, this sub-analysis indicates that the changes in medication were from the clinical perspective mild and did not explain the TR improvement we observed. Focusing on the temporal changes of TR alterations, relevant changes occurred within the first 3 months post TMVR, while there were no significant differences comparing 3-month and 12-month TR. This supports the idea that the majority of TR improvement occurs during the first 3 months, and not thereafter. However, this has to be proven in a prospective randomised clinical trial with an appropriate sample size.
TR IMPROVEMENT DUE TO TMVR AND THE ROLE OF TAD
For decades the idea has persisted that tricuspid pathology is spontaneously regressive once left-sided heart lesions have been successfully treated. Today, recommendations favour concurrent tricuspid valve surgery at the time of left-sided valve repair2. However, modern percutaneous approaches are considered to be safe even in reinterventions due to their minimally invasive character. Moreover, transcatheter approaches for isolated severe MR, TR or simultaneous repair of severe MR and TR represent novel and innovative treatment options in our patients11,12,17. Conclusively, in contrast to surgical repair for transcatheter therapy, a wait-and-see approach may be feasible regarding TR patients undergoing mitral valve repair. Optimally, if there is an improvement of TR post TMVR, the additional risks and costs of TR repair might be avoided. The present study indicates that TMVR may lead to an improvement of TR. Here, 41% of patients with moderate or worse TR showed a marked TR reduction during follow-up. However, for the total cohort, a proportion of patients with severe or worse TR experienced only a minor decline from 19% to 17%. Especially in patients with a TAD ≥34 mm, TR improvement was less frequent compared to in patients with a TAD <34 mm (35% vs 54%, respectively). Moreover, persistent TR ≥II was more frequent in patients with a TAD ≥34 mm than in patients with a TAD <34 mm (75% vs 50%, respectively) (Figure 2B, Figure 2C). Thus, TAD ≥34 mm might represent a relevant criterion to argue for immediate treatment of concomitant tricuspid valve disease. In surgical treatment of TR, TAD already has a significant role within the current guidelines, where TR surgery should be considered in patients with mild to moderate TR undergoing left-sided valve surgery with a TAD of ≥40 mm1. This concept could be of value in interventional TR treatment. Heart failure patients with relevant tricuspid annular dilatation undergoing TMVR for functional MR could therefore profit from a simultaneous tricuspid repair, even when TR has not yet reached advanced severity. Overall, there is an increasing amount of evidence supporting a more progressive treatment approach for secondary TR in which interventional TR treatment may represent a very promising complement in this area.
Patients with post-procedural TR improvement or TAD <34 mm revealed lower rates of post-procedural HHF with an association in the multivariable Cox regression analysis (TR improvement HR 0.6 [0.38-0.94] and TAD ≥34 mm HR 1.56 [1.06-2.29]). Although this might indicate a relevant role of TR improvement in clinical prognosis after TMVR, these findings must be interpreted with caution. Future studies are desirable to investigate whether TR development itself has an impact on prognosis, or if progressive functional TR is more an epiphenomenon of underlying heart failure deterioration leading to progressive TR. Nonetheless, our data indicate that TR development and heart failure are correlated, and that TR improvement and TAD decline can be considered as an additional marker of successful TMVR.
For surgical tricuspid therapy, tricuspid annulus, pulmonary hypertension, right ventricular dilation, and right ventricular dysfunction are parameters which have an influence on the decision making1,18. However, we did not find an association of echocardiographically estimated systolic pulmonary artery pressure with TR improvement, which is in contrast to prior studies8,9. Assessment of pulmonary artery pressure by echocardiography may have caused equalisation of right atrial and ventricular pressures in TR, and thus led to an underestimation19. Unfortunately, right heart catheterisation for higher accuracy of pulmonary pressure assessment was not performed routinely in the present study cohort. Here, patients with TR improvement had a smaller TAD, lower prevalence of AF and less residual MR at discharge. These parameters appeared very useful markers of TR reversibility after TMVR. Since less successful TMVR with post-procedural residual MR seems to be associated with worse outcome regarding TR development, surgical double valve treatment may be reconsidered, and may be a viable option in surgical candidates. Tricuspid annular dilatation is known to be associated with TR and poor prognosis20. In the present study, the best cut-off value was a TAD of ≥34 mm, and a decline of TAD indicated TR improvement. Moreover, patients with a remaining tricuspid annular dilatation at follow-up had a lower post-procedural event-free survival from HHF. Ultimately, TAD might serve as a sensitive marker for monitoring and decision making concerning concurrent mitral and tricuspid valve repair or TMVR-first followed by TTVR-second or no TTVR.
Study limitations
To the best of our knowledge, the present multicentre study included the largest patient cohort assessing this topic; however, several limitations must be acknowledged. First, the study`s observational character warrants cautious interpretation and confirmation by controlled prospective studies. Second, there was no central echocardiography core laboratory and event adjudication. Furthermore, the number of follow-up echocardiographic assessments was limited. Analysis of post-procedural HHF must be interpreted with caution. The analysis of HHF rates and TR improvement/tricuspid annular dilatation showed a strong correlation; however, conclusions regarding pathophysiological causalities cannot be made. Finally, analysis of multiple variables is prone to confounders and the absence of statistical significance may be due to the sample size.
Conclusions
In patients undergoing TMVR, improvement of relevant TR (TR ≥II) is a frequent phenomenon within the first three months post TMVR. AF, rMR ≥II at discharge and TAD at baseline were independent and significant predictors preventing TR improvement and may help to define whether concomitant tricuspid valve disease should be treated immediately, second after a post-TMVR observational period, or not at all. Lastly, TR improvement and TAD <34 mm at follow-up were markers associated with lower rates of post-procedural heart failure hospitalisation.
|
Impact on daily practice A MitraClip procedure for mitral regurgitation may lead to an improvement of relevant concomitant tricuspid regurgitation. Parameters which prevent this improvement are (1) atrial fibrillation, (2) post-procedural residual mitral regurgitation ≥II, and (3) tricuspid annular diameter (especially a tricuspid annular diameter of ≥34 mm). TAD represents a significant predictor which may be helpful in deciding between simultaneous mitral and tricuspid valve repair, or TMVR and re-evaluation of TR. The optimal timing of TR re-evaluation seemed to be at three months after a MitraClip procedure as improvement of TR was more likely to happen early after TMVR. |
Conflict of interest statement
G. Nickenig has received speaker honoraria and research grants from Abbott, Abiomed, Medtronic, Boston Scientific, and Edwards Lifesciences, outside the submitted work. S. Baldus has received lecture honoraria from Edwards Lifesciences, Bayer Vital, CVRx, MSD Sharp & Dohme GmbH, JenaValve Technology, and Abbott, and research grants from Vifor Pharma, Symetis SA, Pfizer, JenaValve Technology, Valtech, OptumInsight, Biotronik and Abbott, outside the submitted work. R. Pfister has received speaker and consultant honoraria from Abbott and Edwards Lifesciences, outside the submitted work. C. Iliadis has received travel support from Abbott and speaker and consultant honoraria by Abbott and Edwards Lifesciences, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.