Abstract
Background: In patients with severe mitral regurgitation (MR) who are scheduled for transcatheter mitral valve repair (TMVR), risk stratification is predominantly based on surgical risk scores.
Aims: We sought to characterise and define stages of right heart remodelling in patients undergoing TMVR and evaluate the impact of this staging classification on survival.
Methods: According to echocardiographic parameters, 929 patients undergoing MitraClip treatment were classified into three stages: severe MR without right heart damage (stage 0), with moderate-to-severe tricuspid regurgitation (TR) (stage 1), with right ventricular dysfunction defined as a reduced fractional area change <35% and a tricuspid annular plane systolic excursion <17 mm, or with increased right atrial area >25 cm2 and/or indexed right ventricular volume >30 ml/m2 (stage 2). We compared clinical outcomes and performed a multivariate analysis to evaluate the predictive value of the extent of cardiac damage.
Results: Rates of one-year all-cause mortality increased with more advanced stages of right heart remodelling (stage 0: 8% vs stage 1: 9.7% vs stage 2: 18.1%; p<0.001). In the multivariate analysis, advanced cardiac damage was an independent predictor of one-year all-cause mortality (stage 2: p=0.007).
Conclusions: A simple staging classification objectively characterises the extent of right heart remodelling caused by MR and allows risk prediction in patients undergoing a MitraClip procedure.
Introduction
Heart valve diseases especially affect the elderly population and are, therefore, expected to become more prevalent in the coming decades. Apart from aortic valve stenosis, mitral valve regurgitation (MR) is the most common valvular disease12. According to the current guidelines, an assessment of MR severity is based on an integrated approach that includes qualitative, semiquantitative, and quantitative echocardiographic parameters1. Additionally, the symptomatic status as well as an assessment of the surgical risk is decisive for the treatment strategy in patients fulfilling the echocardiographic criteria1.
Transcatheter mitral valve therapies, such as edge-to-edge repair with the MitraClip™ system (Abbott Laboratories, Abbott Park, IL, USA), have emerged as a viable treatment option in elderly patients at high surgical risk, who are deemed unsuitable for heart valve surgery due to concomitant comorbidities and frailty345678. In these high-risk patients, the risk assessment is performed by an interdisciplinary Heart Team, considering commonly used risk scores such as the logistic European System for Cardiac Operative Risk Evaluation (logistic EuroSCORE)12. These risk scores include patient-related clinical factors, comorbidities, and laboratory parameters9. However, there are no recommendations or risk assessment tools that consider right heart remodelling or damage caused by severe mitral regurgitation.
In this multicentre study, we sought to characterise and classify right heart remodelling in patients with severe MR undergoing a MitraClip procedure and evaluate the impact of a newly defined staging classification on the outcome.
Methods
PATIENT POPULATION
Between September 2010 and February 2019, 1,105 consecutive patients with severe symptomatic MR underwent a MitraClip procedure at the Heart Center Bonn, Cologne, or Düsseldorf. Of these patients, we had to exclude 176 patients due to a lack of echocardiographic parameters. Finally, we included a total of 929 patients undergoing a MitraClip procedure due to severe MR in this study (Figure 1). The study was approved by the local ethics committees and all patients participated in this study after having provided written informed consent.
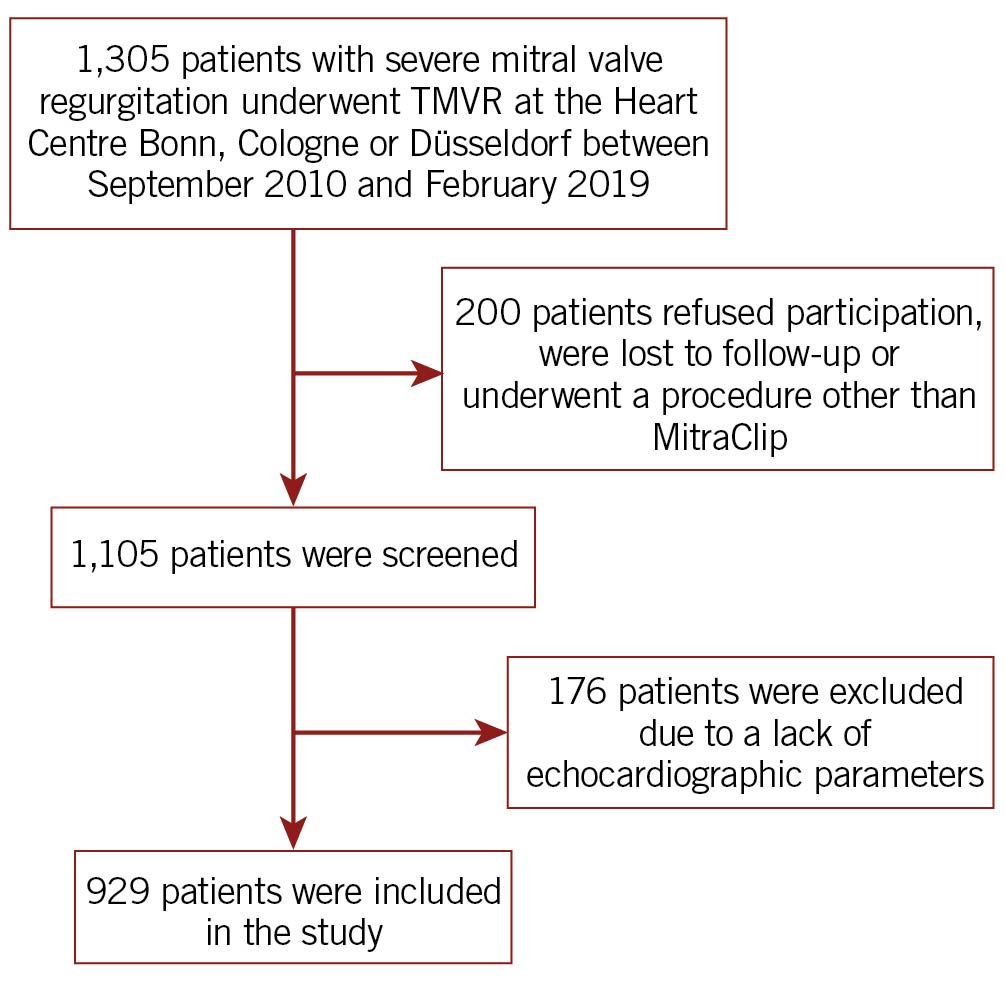
Figure 1. Study flow chart. TMVR: transcatheter mitral valve repair
Before the MitraClip procedure, all patients underwent a standardised evaluation including echocardiography, left and right heart catheterisation, pulmonary function test and an angiology examination. Details about patient screening have been described previously10. The MitraClip procedure was performed in a hybrid operating room under general anaesthesia with transoesophageal and fluoroscopic guidance, as previously described111213.
STAGING CLASSIFICATION
First of all, we identified individual transthoracic echocardiographic parameters that were associated with worse outcomes in our study cohort. In the selection of these parameters, we considered their simplicity of acquisition and abnormality of cardiac function: left-sided heart valve defects have been shown to be associated with the occurrence of tricuspid regurgitation, which negatively affects patient outcomes1415; right ventricular dysfunction is a common finding in patients with MR and has been shown to be a negative prognostic marker in this patient cohort1617; and an indirect consequence of mitral regurgitation, for example, through the presence of atrial fibrillation or tricuspid valve regurgitation, is right heart dilatation, which has been shown to be associated with worse outcomes181920.
According to the echocardiographic parameters, all patients were classified into three stages: severe MR without right heart damage (stage 0), with tricuspid valve affection with moderate-to-severe tricuspid regurgitation (TR) (stage 1), with right ventricular dysfunction that was defined as a reduced fractional area change <35% and a reduced tricuspid annular plane systolic excursion (TAPSE) <17 mm, or with right heart damage with increased right atrial area >25 cm2 and/or indexed right ventricular volume >30 ml/m2 (stage 2) (Figure 2).
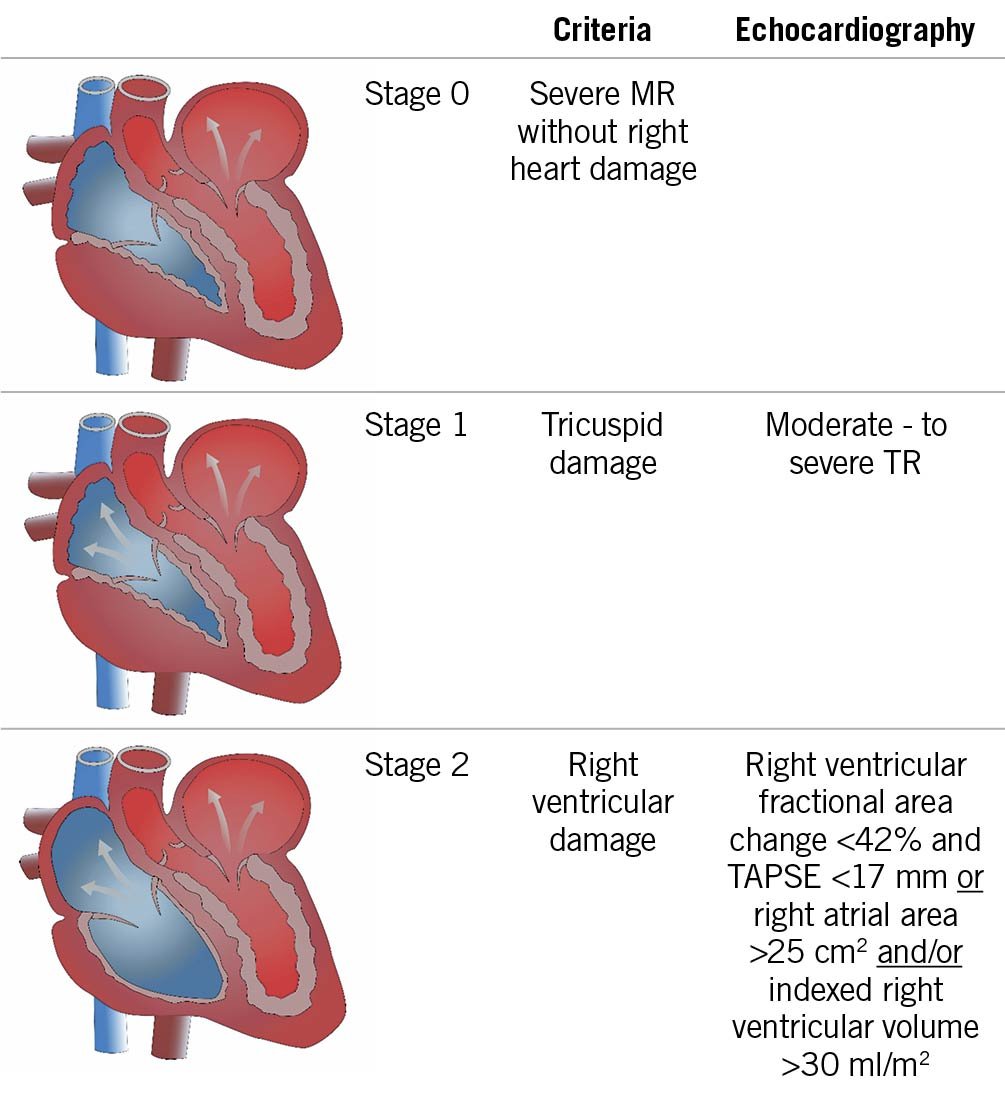
Figure 2. Staging classification according to right heart remodelling in patients undergoing a MitraClip procedure due to severe MR. MR: mitral valve regurgitation; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid valve regurgitation
In all patients, stratification into a given stage was based on preprocedural transthoracic echocardiography. Patients were classified into the most advanced stage if the echocardiographic criteria of that stage were fulfilled.
STUDY ENDPOINT, DATA COLLECTION, AND FOLLOW-UP
One-year all-cause mortality was the primary endpoint of our study. After discharge, clinical follow-up data were prospectively collected during scheduled outpatient clinic visits or direct telephone interviews with the referring cardiologists, general practitioners, and patients.
STATISTICAL ANALYSIS
Data are presented as the mean±standard deviation, if normally distributed, or as the median and interquartile range (IQR) (quartile 1/quartile 3), if not normally distributed. Continuous variables were tested for having a normal distribution with the use of the Kolmogorov-Smirnov test. Categorical variables are given as frequencies and percentages. For continuous variables, a Student’s t-test or a Mann-Whitney U test was performed, as appropriate, for a comparison between two groups. When comparing more than two groups, analysis of variance (ANOVA) or the Kruskal-Wallis test was used. Spearman’s correlation coefficients were used to establish associations. The χ2 test was used for analysis of categorical variables.
For the statistical analysis, we compared the outcomes between the four stages of cardiac remodelling and performed Kaplan-Meier survival analyses. A log-rank test was used to determine statistical differences in terms of survival. Finally, we performed a multivariate Cox proportional hazards regression analysis, which included univariate predictors with a p-value <0.1, to assess independent predictors of one-year all-cause mortality.
Statistical significance was assumed when the null hypothesis could be rejected at p<0.05. Statistical analyses were conducted with PASW Statistics, version 24.0.0.0 (IBM Corp., Armonk, NY, USA) and MedCalc, version 11.6.1.0 (MedCalc Software Ltd, Ostend, Belgium). The investigators initiated the study, had full access to the data, and wrote the manuscript. All authors vouch for the data and its analysis.
Results
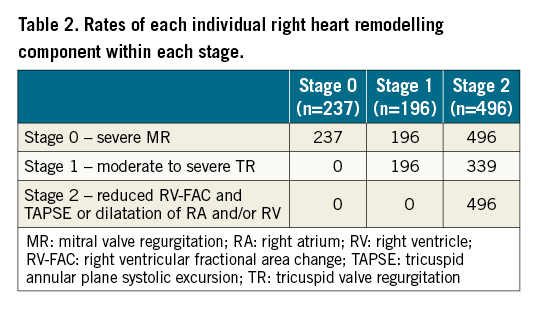
Out of 929 patients undergoing a MitraClip procedure, 50.4% were male, and the mean age of the study population was 77 years. According to preprocedural echocardiography, 237 (25.6%) patients were in stage 0 (severe MR without right heart damage), 196 (21.1%) patients were in stage 1 (moderate-to-severe tricuspid valve regurgitation), and 496 (53.3%) patients were in stage 2 (right heart remodelling/damage). The prevalence of these right heart remodelling stages is shown in Figure 3. Baseline and procedural characteristics according to the different stages are presented in Table 1. The rates of each individual cardiac damage component within each stage are presented in Table 2.
Figure 3. Prevalence of right heart remodelling stages in the patient population. According to preprocedural echocardiography, 237 (26%) patients were in stage 0, 196 (21%) patients were in stage 1, and 496 (53%) patients were in stage 2.
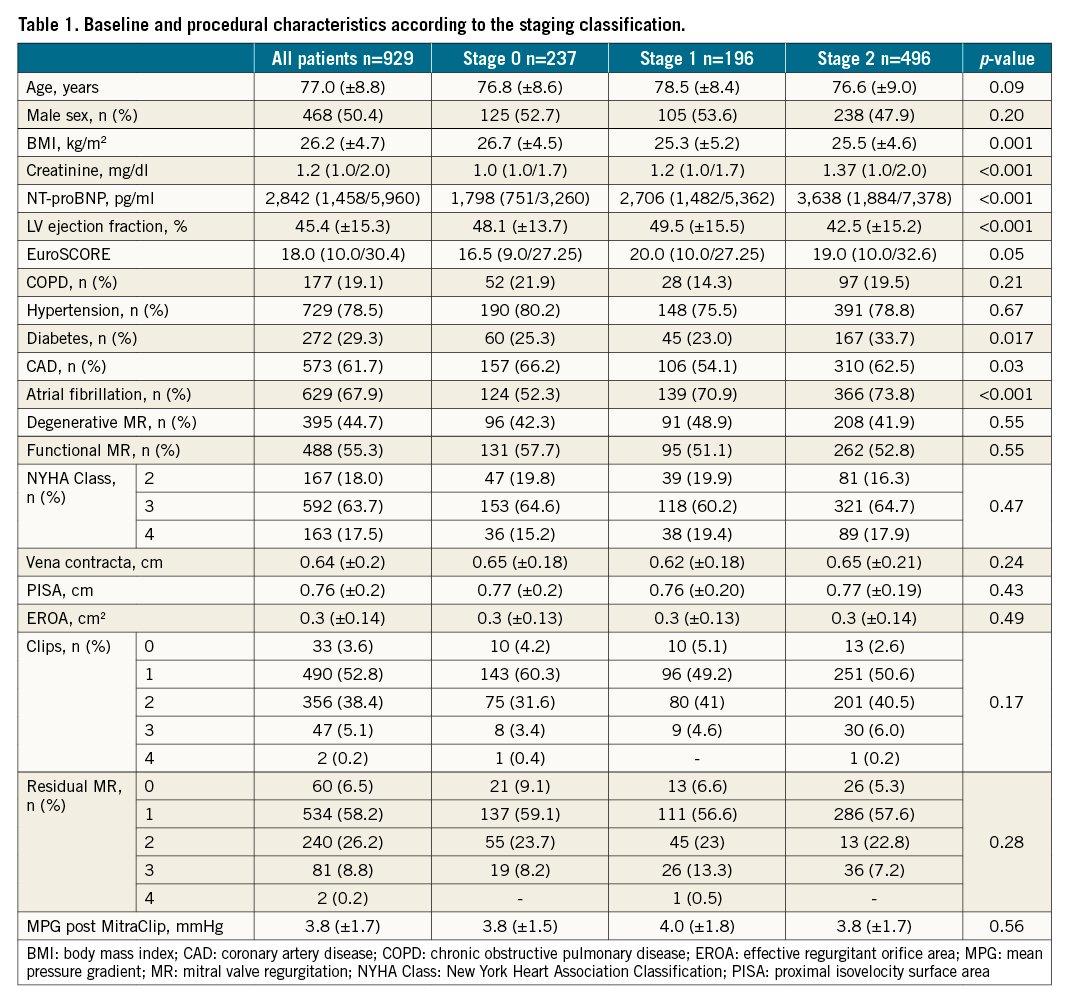
Patients in the more advanced stages suffered from higher rates of comorbidities, such as chronic renal failure, reduced ejection fraction, diabetes or atrial fibrillation. Interestingly, these results were not reflected by a higher logistic EuroSCORE. However, advanced right heart remodelling stages were associated with higher N-terminal pro-brain natriuretic peptide (NT-pro-BNP) values at baseline.
OUTCOME ACCORDING TO THE STAGING CLASSIFICATION
All-cause mortality rates within one year were associated with an advanced stage of right heart remodelling (stage 0: 8% vs stage 1: 9.7% vs stage 2: 18.1%; p<0.001), as shown in Figure 4.
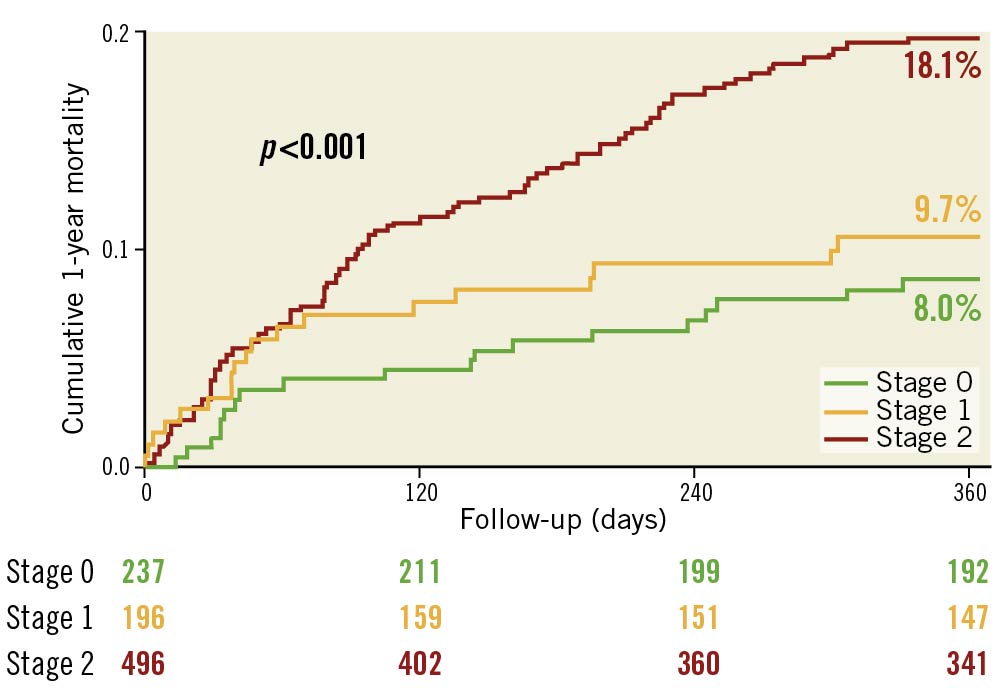
Figure 4. Kaplan-Meier survival analysis of one-year all-cause mortality in patients undergoing a MitraClip procedure according to right heart remodelling. All-cause mortality rates within one year were associated with an advanced stage of right heart remodelling (stage 0: 8% vs stage 1: 9.7% vs stage 2: 18.1%; p<0.001).
To evaluate further the impact of right heart damage on outcome according to MR aetiology, we substratified our patient cohort according to functional (FMR) and degenerative MR (DMR) and performed another survival analysis (Figure 5). In both groups, right heart damage (stage 2) was significantly associated with mortality (FMR: stage 0: 6.9% vs stage 1: 12.6% vs stage 2: 17.9%; p=0.007; DMR: stage 0: 9.4% vs stage 1: 5.5% vs stage 2: 19.2%; p=0.005).
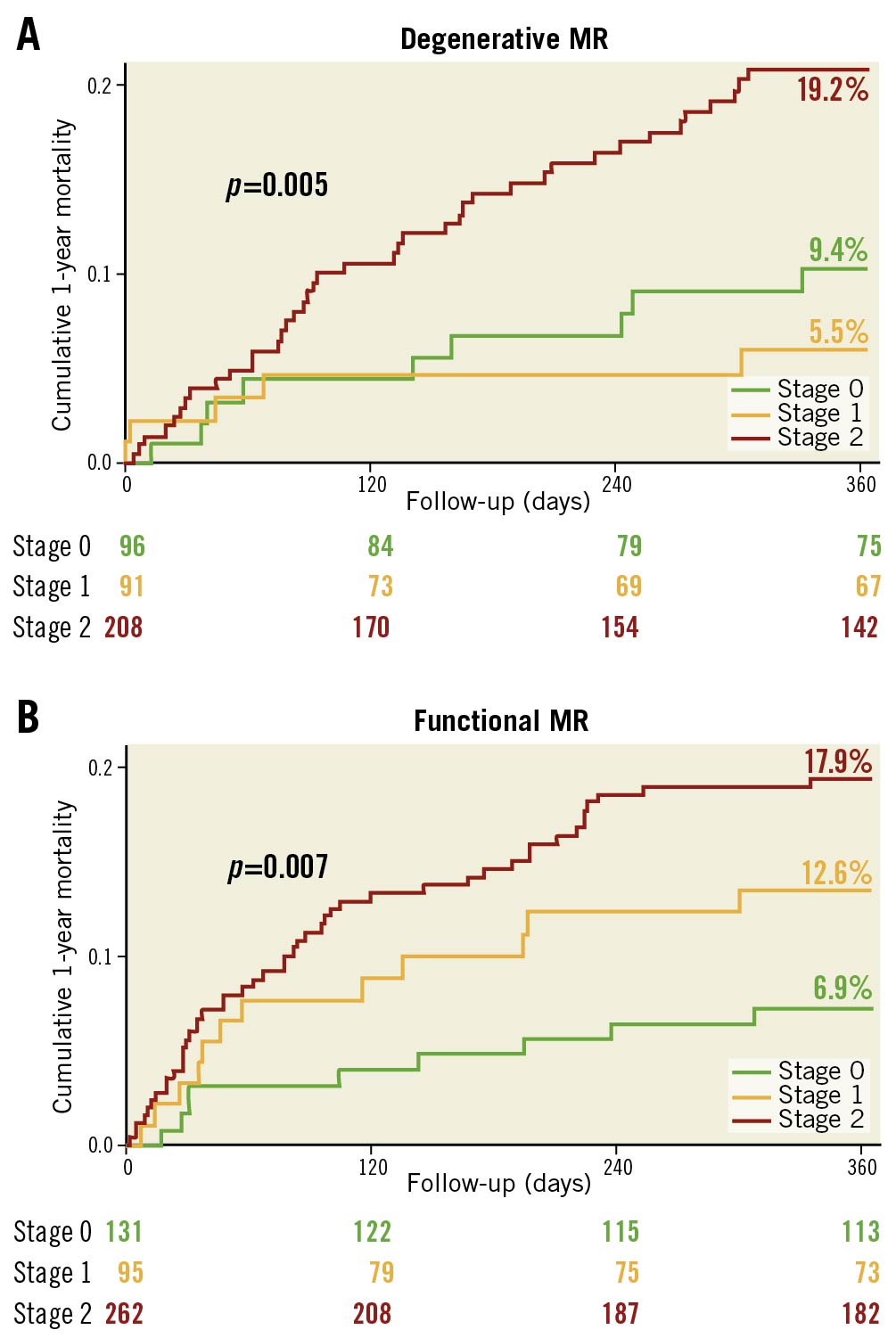
Figure 5. Kaplan-Meier survival analysis of one-year all-cause mortality in patients undergoing a MitraClip procedure according to right heart remodelling and MR aetiology. In patients with degenerative MR (A) as well as in patients with functional MR (B), right heart damage (stage 2) was significantly associated with mortality (DMR: stage 0: 9.4% vs stage 1: 5.5% vs stage 2: 19.2%; p=0.005; FMR: stage 0: 6.9% vs stage 1: 12.6% vs stage 2: 17.9%; p=0.007). MR: mitral valve regurgitation
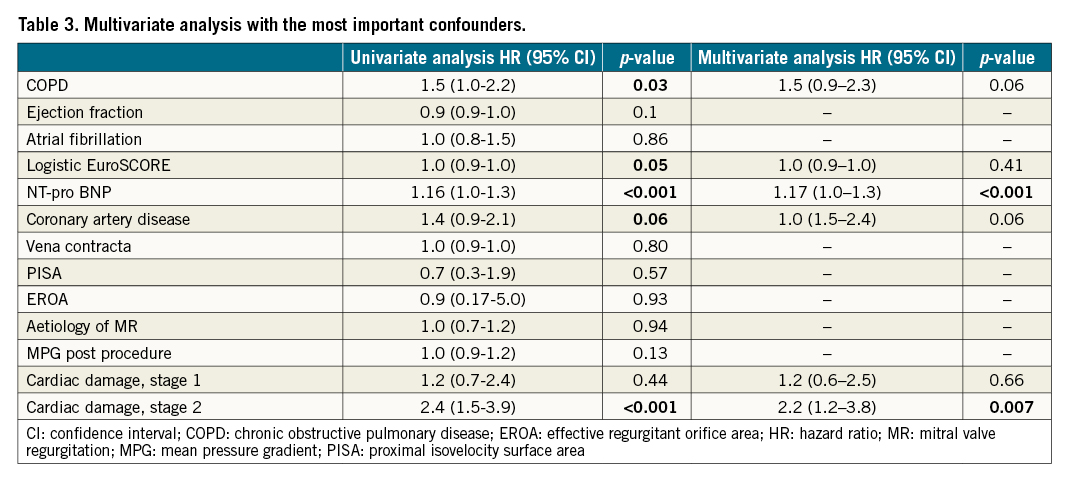
MULTIVARIATE ANALYSIS
In multivariate analyses, right heart damage, as represented by stage 2, was independently predictive of one-year all-cause mortality (stage 2: p=0.007), as shown in Table 3. Elevated NT pro-BNP values (p<0.001) were the only other independent predictor of one-year all-cause mortality following the MitraClip procedure. MR severity at baseline, represented by echocardiographic parameters such as the proximal isovelocity surface area (PISA), vena contracta and the effective regurgitant orifice area (EROA), as well as the aetiology of MR, were not associated with a worse outcome in univariate analysis. The logistic EuroSCORE was significantly associated with mortality in univariate analysis, contrary to the new staging classification; however, it was not independently predictive of one-year all-cause mortality.
Discussion
This multicentre study, including 929 patients undergoing a MitraClip procedure for the treatment of severe MR, showed a significant association between right heart remodelling due to MR at baseline and one-year all-cause mortality. Advanced right heart damage, as represented by a new staging classification, has been identified as one of the strongest predictors of an adverse outcome after transcatheter mitral valve repair with the edge-to-edge MitraClip technique.
Risk assessment remains challenging when deciding on optimum treatment strategies in elderly patients with severe MR. According to the current recommendations, risk stratification is performed by an interdisciplinary Heart Team, considering commonly used risk scores, such as the logistic EuroSCORE12. These risk scores include patient-related clinical parameters, comorbidities, and laboratory parameters9; however, they do not consider anatomical and functional cardiac remodelling and right heart damage caused by severe MR. However, taking into account the association between the extent of right heart remodelling caused by MR at baseline and mortality after the MitraClip procedure, which was demonstrated by this study, the assessment of right heart remodelling might be useful to optimise risk stratification and Heart Team decision making. Similar results have been recently published by Généreux et al21, investigating the impact of cardiac damage on outcomes in patients with severe aortic stenosis. The authors showed that advanced cardiac damage was also significantly associated with mortality in this patient cohort.
Our multivariate analysis identified the more advanced stage of right heart remodelling as an independent predictor of one-year all-cause mortality in patients with severe MR undergoing a MitraClip procedure – contrary to the logistic EuroSCORE and other comorbidities, such as coronary artery disease or chronic obstructive pulmonary disease. Our findings suggest that more emphasis should be given to the extent of right heart remodelling at baseline, as the assessment of this parameter is simple and provides additional information to improve risk stratification.
Notably, right heart remodelling was a considerably stronger predictor of adverse outcomes than echocardiographic parameters that describe MR severity at baseline such as PISA, vena contracta, regurgitation volume, and EROA, indicating that the extent of cardiac damage represents, at least partly, a persistent haemodynamic burden for patients with severe MR. This generates the hypothesis that patients with severe MR might benefit the most from early treatment, before they develop advanced right heart dysfunction or damage – even if they are still asymptomatic. Conversely, we cannot assume that patients in advanced stages of MR do not benefit from the MitraClip procedure anymore, as their outcome without therapy could be even worse.
Previous studies have already shown the negative impact of concomitant tricuspid regurgitation (TR) on outcome in patients undergoing a MitraClip procedure due to MR2223. This finding could be confirmed by our study. It is conceivable that advanced TR contributes adversely to the progression of right heart remodelling and that patients with concomitant TR will possibly profit from additional tricuspid valve repair.
MR leads to left ventricular (LV) and left atrial (LA) volume overload, resulting in LV and LA dilatation24. Rising LA pressure contributes to an increase in pulmonary artery pressure, leading to right atrial and ventricular pressure overload, inducing tricuspid regurgitation and, ultimately, right heart dysfunction and remodelling25. So far, there are few data investigating the prevalence of extravalvular cardiac damage in patients with severe MR. Similar to previous registries578, our study population represented inoperable real-world patients, with advanced age, reduced LV ejection fraction at baseline and a high median logistic EuroSCORE of 18.0. Of those, 74% of the included patients presented with extravalvular cardiac damage, resulting in most of these patients being assigned to stage 2 owing to right heart damage. However, contrary to what was suggested in the literature, patients do not seem to go systematically and consecutively through all of the stages of cardiac remodelling, as patients in the advanced stages did not always comply with the criteria of earlier stages. This result might suggest that the occurrence of right heart remodelling is, at least partly, influenced by individual and patient-related factors such as genetic predisposition, resistance, and/or resilience.
The results of this study should be considered as hypothesis-generating. Larger and prospective trials are needed to confirm our findings and to evaluate further the evolution of right heart remodelling in patients with severe MR undergoing a MitraClip procedure.
Study limitations
An important limitation of our study is the retrospective study design. In our analysis, we only included patients with severe MR undergoing the MitraClip procedure. Patients undergoing surgical valve repair or replacement as well as patients undergoing other transcatheter valve therapies were excluded from the analysis. Furthermore, we only included high-risk patients deemed unsuitable for surgery. Therefore, caution should be used in generalising the present findings. Nevertheless, our findings are hypothesis-generating and will serve as a pivotal foundation for further investigations into an optimal treatment strategy in patients suffering from MR.
Conclusions
Right heart remodelling and the extent of cardiac damage are associated with an adverse outcome in patients undergoing a MitraClip procedure to treat severe MR (Central illustration). A simple staging classification objectively characterises the extent of right heart remodelling caused by MR and allows risk prediction in these patients.
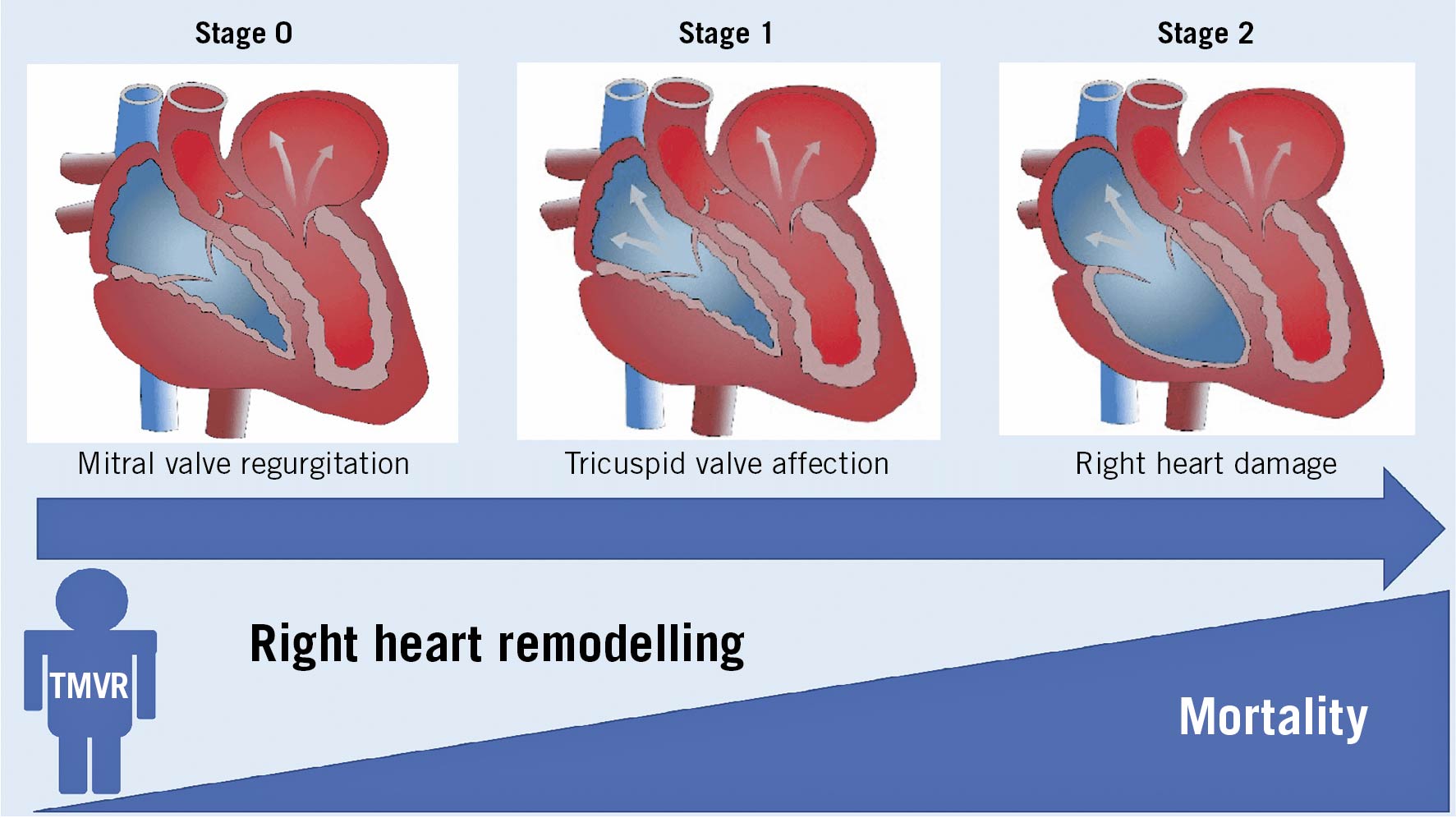
Central illustration. Right heart remodelling and the extent of cardiac damage is associated with mortality in patients undergoing a MitraClip procedure to treat severe mitral valve regurgitation. TMVR: transcatheter mitral valve repair
Impact on daily practice
This is the first study characterising stages of right heart remodelling based on echocardiographic parameters in patients with severe MR undergoing transcatheter mitral valve repair (TMVR) and evaluating the impact of this staging classification on survival. Our study results show that a simple staging classification objectively characterises the extent of right heart remodelling caused by MR and allows risk prediction in patients undergoing a MitraClip procedure. Larger prospective studies need to confirm our staging classification and its impact on outcome.
Conflict of interest statement
J.M. Sinning has received speaker honoraria and research grants from Abbott, Abiomed, Medtronic, Boston Scientific, and Edwards Lifesciences. R. Pfister has received “modest” speaker and consultant honoraria by Abbott and Edwards Lifesciences, outside the submitted work. C. Iliadis has received travel support from Abbott and speaker and consultant honoraria from Abbott and Edwards Lifesciences, outside the submitted work. M. Kelm reports receiving fees from Bunnenberg Stiftung, grants from DFG CRC 1116, during the conduct of the study, grants from Philips, Abbott, Medtronic, Boston Scientific, Mars, and Boehringer Ingelheim, personal fees from Daiichi Sanyko Deutschland GmbH and Ancora Heart, grants and personal fees from Amgen, and grants from B.Braun, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.