Abstract
Background: In terms of pathophysiology, tricuspid regurgitation (TR) and right ventricular (RV) function are linked to each other.
Aims: This study sought to evaluate RV-pulmonary artery (PA) coupling and its impact on clinical outcomes of TR in patients undergoing mitral transcatheter edge-to-edge repair (TEER).
Methods: We calculated RV-PA coupling ratios in patients undergoing mitral TEER from August 2010 to March 2019 by dividing the tricuspid annular plane systolic excursion (TAPSE) by the echocardiographic estimated PA systolic pressure (PASP). TR was graded as none/trace, mild, moderate, or severe. The primary outcome was all-cause mortality or rehospitalisation within 12 months.
Results: Among 744 patients analysed, severe TR was documented in 22.3% of patients and the mean TAPSE/PASP was 0.43±0.25. Technical success of TEER was achieved in 97.2% of participants. Severe TR vs TR ≤moderate (adjusted HR 1.92, 95% CI: 1.39-2.66) and TAPSE/PASP (adjusted HR 0.45, 95% CI: 0.22-0.93) were associated with the outcome. Patients were divided according to the TAPSE/PASP tertile. Compared to patients with TR ≤moderate, patients with severe TR had a higher event rate (TAPSE/PASP <0.30: 32.9% vs 45.1%; 0.30≤ TAPSE/PASP <0.44: 27.8% vs 41.8%; TAPSE/PASP ≥0.44: 16.0% vs 40.4%), whereas the prognostic significance of TR was attenuated in patients with reduced TAPSE/PASP (i.e., RV-PA uncoupling; interaction term p=0.03). The trends were consistent in the multivariable regression models, spline curves, and sensitivity analysis using post-interventional parameters.
Conclusions: RV-PA coupling affects the outcome correlation of TR in patients undergoing mitral TEER. The prognostic impact of TR is attenuated in patients with RV-PA uncoupling.
Introduction
Tricuspid regurgitation (TR) is a highly prevalent disease in ageing societies1. TR commonly accompanies mitral regurgitation (MR), and functional TR is caused by pulmonary hypertension, right ventricular (RV) remodelling, and tricuspid annular dilatation1. Despite the development of therapeutic options for MR, previous studies collectively have shown that TR has a substantial impact on prognosis following transcatheter edge-to-edge repair (TEER) for MR23. In terms of pathophysiology, TR and RV function are tightly linked to each other. RV longitudinal elongation and spherical deformation lead to subsequent tricuspid leaflet tethering and the development of TR4. However, it remains uncertain whether TR contributes alone to the dismal outcome of TEER for MR or acts in conjunction with RV function. More specifically, RV function may interact with the prognostic impact of TR.
RV function can non-invasively be assessed by 2D Doppler echocardiography. Moreover, RV to pulmonary artery (RV-PA) coupling refers to the relationship between RV systolic function and RV afterload. Studies evaluating the RV-PA coupling in patients undergoing TEER for MR have shown that a lower tricuspid annular plane systolic excursion / pulmonary arterial systolic pressure (TAPSE/PASP), which reflects RV-PA uncoupling, was associated with adverse outcomes567. Despite the fact that TR and impaired RV systolic function often coexist5, no published studies have examined the hypothesis that the clinical relevance of TR changes according to RV function, which would be fundamental in providing optimal therapeutic strategies for each individual. In the present study, we tested the hypothesis that the prognostic impact of TR may change according to RV-PA coupling.
Methods
Study setting and design
The present analysis is based on data from the Rhineland registry, which is a prospective, multicentre, consecutive collection of patient information from three centres in Germany (Bonn, Cologne, Düsseldorf). We reviewed patients who underwent TEER with the MitraClip system (Abbott) to treat MR from August 2010 to March 2019. All patients suffered from symptomatic MR and were deemed either as ineligible or high risk for conventional surgery. For the purpose of the present analysis, patients were excluded if they had an absence of echocardiographic data within a time window of three months prior to TEER or if the baseline echocardiography was not adequate for the assessment of right ventricular function and tricuspid regurgitation. The study protocol was approved by the ethics committee of each centre. All patients provided written informed consent.
Assessment of tricuspid regurgitation
All study participants underwent transthoracic echocardiography. The acquired images were evaluated by board-certified cardiologists at each centre’s echo laboratory. In the case of atrial fibrillation, three consecutive heartbeats were averaged to give an accurate measurement of the echocardiographic parameters. The assessment and grading of TR severity were based on both qualitative and quantitative parameters, as recommended in the guidelines89. The degree of TR was graded as follows: none/trace, mild, moderate, and severe. The vena contracta, effective regurgitant orifice area and regurgitant volume were also measured by proximal isovelocity surface area methods at baseline.
Assessment of right ventricular function
We assessed RV-PA coupling by calculating the TAPSE/PASP ratio10. Both parameters were routinely recorded in the echocardiography studies at each centre. TAPSE was measured by using M-mode echocardiography with the cursor aligned on the tricuspid lateral annulus in the apical four-chamber view. TR pressure gradient was estimated from the peak velocity of the TR jet by utilising the simplified Bernoulli equation. The PASP was then calculated by adding the estimated right-atrial pressure according to the dimension of the inferior vena cava and its respiratory change. Additionally, RV fractional area change (RVFAC) <35% was calculated as [RV end-diastolic area – RV end-systolic area] / RV end-diastolic area ×1008.
Clinical outcomes
The primary endpoint was a composite of mortality and heart failure rehospitalisation within 12 months after TEER. We also assessed each outcome separately. Clinical follow-up data were obtained through standardised interviews at scheduled hospital visits, telephone interviews with the patient’s family, or documentation from the referring general practitioners. Acute technical success of TEER was defined according to the Mitral Valve Academic Research Consortium guidelines11.
Statistical analysis
Continuous variables are reported as the mean±standard deviation (SD) or as medians and interquartile ranges (IQR), while categorical variables are reported as the number (percentage). The study population was divided into three groups according to tertiles of TAPSE/PASP. Continuous variables were compared using the one-way analysis of variance or Kruskal-Wallis tests. The chi-square test was applied to compare categorical variables. The Tukey’s honestly significant difference test was used to adjust for multiple testing between the groups. We also created receiver operating characteristic curves of TAPSE and TAPSE/PASP for predicting the primary endpoint.
To examine the study inference, we performed the following analyses. First, we fitted a Cox proportional hazard model to test the clinical significance of severe TR for the outcomes. The models were adjusted for age, sex, atrial fibrillation, coronary artery disease, estimated glomerular filtration rate, logistic EuroSCORE, New York Heart Association Functional Class, left ventricular (LV) ejection fraction, severity of MR, and TAPSE/PASP51012. Hazard ratios (HR) and 95% confidence intervals (95% CI) were determined. Second, we depicted spline curves for the outcome correlation of TR across TAPSE/PASP. Third, an interaction term analysis was performed. Additionally, we conducted a mediation analysis using severe TR as an exposure and TAPSE/PASP as a mediator, which could elucidate the direct and indirect effects of TR.
To examine the robustness of our inference, we conducted several sensitivity analyses. We repeated these analyses for the post-procedural TR. Covariables for the adjustment were the aforementioned parameters measured after the procedure. Also, we applied RVFAC/PASP as RV function and depicted spline curves for the outcome correlation of TR across RVFAC/PASP.
Two-tailed p values <0.05 were considered statistically significant. All statistical analyses were performed using R version 3.5.2 (R Foundation for Statistical Computing) and Stata 15.1 (StataCorp).
Results
Population
A total of 744 patients were included in the analysis (Table 1). The mean age was 77±9 years, and 414 (55.7%) were female. The participants exhibited a high logistic EuroSCORE (18.1% [IQR 10.1-31.1%]) and reduced LV ejection fraction (44.5±15.3%). Severe TR was documented in 166 (22.3%) patients. The mean TAPSE was 17.9±5.1 mm, PASP was 48.3±16.8 mmHg, and the TAPSE/PASP ratio was 0.43±0.25 (Supplementary Figure 1). The median time from baseline echocardiography to TEER was 24 days (IQR 5-46 days) in the present analysis. Acute technical success was achieved in 97.2% of study participants.
Table 1. Baseline characteristics according to TAPSE/PASP.
|
All n=744 |
TAPSE/PASP |
||||
|---|---|---|---|---|---|
|
Tertile 1 n=233 |
Tertile 2 n=244 |
Tertile 3 n=267 |
p-value |
||
|
Demographic parameters |
|||||
|
Age, years |
77±9 |
77±9 |
77±9 |
78±8 |
0.31 |
|
Sex female, n (%) |
414 (55.7) |
141 (60.5) |
137 (55.9) |
136 (50.9) |
0.10 |
|
Body surface area, m2 |
1.87±0.22 |
1.84±0.24 |
1.88±0.22 |
1.86±0.29 |
0.30 |
|
Hypertension, n (%) |
581 (78.1) |
179 (76.8) |
203 (83.2) |
199 (74.5) |
0.049 |
|
Diabetes mellitus, n (%) |
222 (29.8) |
77 (33.0) |
80 (32.8) |
65 (24.3) |
0.048 |
|
Coronary artery disease, n (%) |
61.4 (457) |
158 (67.8) |
153 (62.7) |
146 (54.7) |
0.009 |
|
Atrial fibrillation, n (%) |
505 (67.9) |
154 (66.4) |
171 (70.1) |
181 (67.8) |
0.68 |
|
Prior pacemaker/ICD/CRT, n (%) |
288 (38.7) |
98 (42.1) |
100 (41.0) |
90 (33.7) |
0.11 |
|
Prior cardiac surgery, n (%) |
206 (27.7) |
90 (38.6) |
72 (29.5) |
44 (16.5) |
<0.001 |
|
NT-pro-BNP, pg/ml |
2971 [1525, 6345] |
4295* [2225, 8958] |
2932 [1773, 6115] |
1972 [949, 4517] |
<0.001 |
|
Estimated GFR, ml/min/1.73m2 |
47.5±20.6 |
46.3±21.3 |
48.5±19.8 |
47.6±20.8 |
0.48 |
|
Logistic EuroSCORE, % |
22.1 [10.1, 31.1] |
22.1* [13.3, 39.4] |
17.4* [10.6, 28.7] |
13.2* [8.1, 24.9] |
<0.001 |
|
NYHA III/IV, n (%) |
604 (81.2) |
193 (83.2) |
200 (82.0) |
211 (79.0) |
0.47 |
|
Echocardiographic parameters |
|||||
|
LV ejection fraction, % |
44.5±15.3 |
40.1±15.2* |
44.7±15.3* |
48.2±14.4* |
<0.001 |
|
LV end-diastolic volume, ml |
143.8±69.3 |
150.7±66.4 |
141.0±60.0 |
142.7±76.5 |
0.26 |
|
LV end-systolic volume, ml |
86.0±57.5 |
95.4±57.7$ |
84.2±52.1 |
79.4±61.4 |
0.007 |
|
LA volume, ml |
107.8±61.3 |
118.1±75.6$ |
108.1±55.2 |
98.7±51.3 |
0.004 |
|
Functional MR, n (%) |
430 (57.8) |
151 (64.8) |
144 (59.0) |
135 (50.6) |
0.005 |
|
MR moderate-to-severe/severe, n (%) |
634 (85.2) |
192 (84.6) |
205 (84.7) |
237 (88.8) |
0.29 |
|
TAPSE/PASP |
0.43±0.25 |
0.23±0.05* |
0.36±0.04* |
0.67±0.28* |
<0.001 |
|
PASP, mmHg |
48.3±16.8 |
63.3±15.3* |
48.6±10.6* |
34.8±10.3* |
<0.001 |
|
TAPSE, mm |
17.9±5.1 |
14.2±3.6* |
17.6±4.0* |
21.3±4.9* |
<0.001 |
|
RV fractional area change, % |
38.2±11.9 |
33.5±11.5* |
37.8±11.1* |
42.6±11.4* |
<0.001 |
|
RV end-diastolic area, mm2 |
21.3±7.6 |
22.8±7.4$ |
21.5±7.2 |
20.0±7.8 |
<0.001 |
|
Procedural parameters |
|||||
|
Number of clips implanted |
1.5±0.6 |
1.5±0.6 |
1.4±0.6 |
1.5±0.7 |
0.15 |
|
Post-procedural MR ≤moderate |
684 (91.9) |
215 (92.3) |
222 (91.0) |
247 (92.5) |
0.80 |
|
Post-procedural transmitral pressure gradient, mmHg |
3.9±1.8 |
3.7±1.8 |
4.0±1.8 |
3.9±1.7 |
0.12 |
|
*p<0.05 vs All by Tukey’s test. $p<0.05 vs Tertile 3 by Tukey’s test. CI: confidence interval; CRT: cardiac resynchronisation therapy; GFR: glomerular filtration ratio; HR: hazard ratio; ICD: intracardiac defibrillator; LA: left atrial; LV: left ventricular; MR: mitral regurgitation; NYHA: New York Heart Association; PASP: pulmonary artery systolic pressure; RV: right ventricular; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid regurgitation |
|||||
Clinical outcomes
During a median follow-up of 18 months (IQR 8-30 months), 100 patients died and 121 patients were hospitalised due to heart failure, and the primary outcome occurred in 196 patients within 12 months. In the univariable Cox proportional hazard model, severe TR in comparison to TR ≤moderate was associated with an increased risk of the primary outcome (unadjusted HR 1.91, 95% CI: 1.41-2.59; p<0.001) (Table 2). The association remained significant (adjusted HR 1.92, 95% CI: 1.39-2.66; p<0.001) after adjusting for the predefined covariates. As for the primary endpoint, severe TR was associated with the increased risk of mortality (adjusted HR 2.15, 95% CI: 1.37-3.38; p<0.001) and rehospitalisation due to heart failure (adjusted HR 1.66, 95% CI: 1.08-2.54; p=0.02) (Table 2). Additionally, in the multivariable Cox proportional hazard model, the TAPSE/PASP ratio was independently associated with the primary endpoint (adjusted HR 0.45, 95% CI: 0.22-0.93; p=0.031) (Figure 1, Supplementary Table 1). The receiver operating characteristics curve analyses of TAPSE and TAPSE/PASP for predicting outcomes are depicted in Supplementary Figure 2.
Table 2. Association of severe TR with clinical outcomes after mitral TEER.
|
Severe TR vs moderate or less TR |
Multivariable adjusted HR (95% CI) |
|||
|---|---|---|---|---|
|
All cohort |
Tertile 1 |
Tertile 2 |
Tertile 3 |
|
|
Primary endpoint |
1.92 (1.39-2.66) |
1.58 (0.92-2.70) |
1.88 (1.05-3.36) |
3.39 (1.79-6.43) |
|
All-cause mortality |
2.15 (1.37-3.38) |
1.79 (0.76-4.18) |
2.69 (1.30-5.56) |
2.80 (1.18-6.64) |
|
Rehospitalisation due to heart failure |
1.65 (1.08-2.54) |
1.49 (0.79-2.81) |
0.95 (0.36-2.48) |
3.82 (1.61-9.08) |
|
The models were adjusted for age, sex, atrial fibrillation, coronary artery disease, estimated glomerular filtration rate, logistic EuroSCORE, New York Heart Association Functional Class, LV ejection fraction, MR, and TAPSE/PASP. CI: confidence interval; HR: hazard ratio; LV: left ventricular; TEER: mitral transcatheter edge-to-edge repair; TR: tricuspid regurgitation |
||||
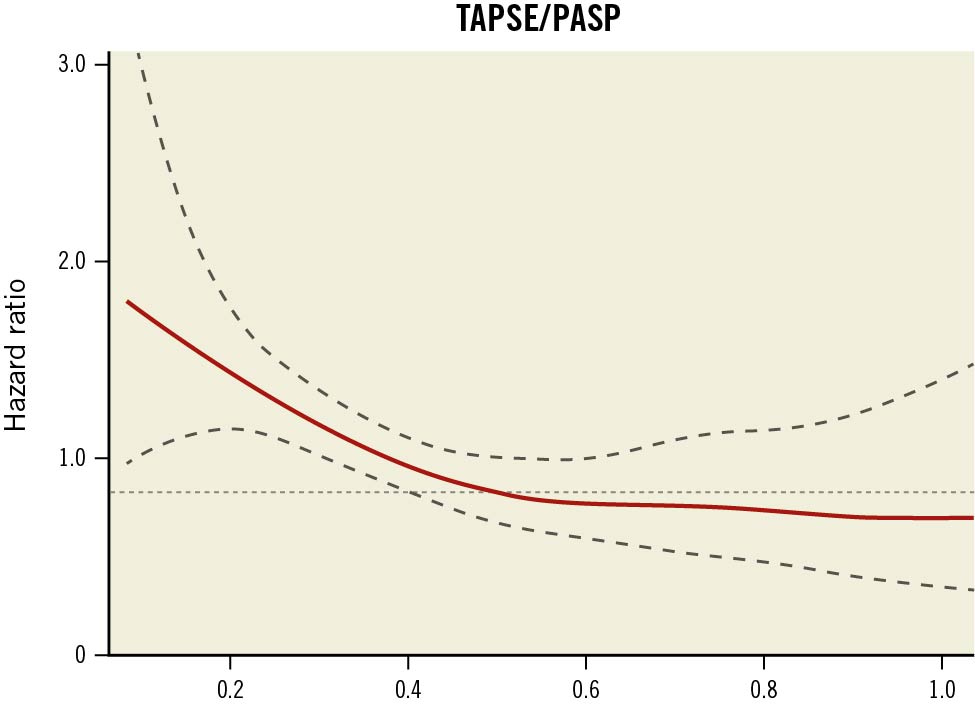
Figure 1. Spline curve for the hazard ratio of TAPSE/PASP. A spline curve for the relationship between TAPSE/PASP and its hazard risk is shown. A linear association was observed: a reduced TAPSE/PASP (i.e., RV-PA uncoupling) was associated with an increased hazard for mortality or heart failure hospitalisation. The association was static if TAPSE/PASP was larger than approximately 0.5. PASP: pulmonary artery systolic pressure; RV-PA: right ventricular-pulmonary artery; TAPSE: tricuspid annular plane systolic excursion
Baseline characteristics according to TAPSE/PASP tertile
Patients were divided according to TAPSE/PASP (Table 1): tertile 1, TAPSE/PASP <0.30 (n=233); tertile 2, 0.30 ≤TAPSE/PASP <0.44 (n=244); tertile 3, TAPSE/PASP ≥0.44 (n=267). Patients in the first tertile were more likely to exhibit comorbidities (coronary artery disease, history of cardiac surgery, and higher NT-pro-BNP and logistic EuroSCORE values) compared with patients in the second or third tertile. Moreover, patients in the first tertile had a significantly reduced LV ejection fraction. The severity of TR differed significantly across the groups (Supplementary Figure 3).
New section
Clinical impact of tricuspid regurgitation in relation to RV function
Kaplan-Meier curves of each tertile are depicted in Figure 2. Compared to patients with TR ≤moderate, patients with severe TR showed a significantly higher outcome incidence in the second tertile (27.8% vs. 41.8%, p=0.03) and in the third tertile (16.0% vs. 40.4%, p<0.001), whereas the difference did not reach statistical significance in the first tertile (32.9% vs. 45.1%, p=0.11). Table 2 lists the multivariable-adjusted HRs of severe TR in each tertile. The association of TR with the primary outcome was pronounced in the second tertile (adjusted HR 1.88, 95% CI: 1.05-3.36; p=0.033) and third tertile (adjusted HR 3.39, 95% CI: 1.79-6.43; p<0.001), while the association was attenuated in the first tertile (adjusted HR 1.58, 95% CI: 0.92-2.70; p=0.10; interaction term p=0.03). The trend was also observed in the fitting spline curves (Figure 3). The prognostic impact of TR was attenuated in patients with reduced TAPSE/PASP, which was consistently observed regardless of the TR grade (i.e., moderate, severe). With a limited sample size, the trend was consistent for mortality and rehospitalisation due to heart failure (Table 2). Furthermore, Supplementary Figure 4 depicts the spline curve showing the outcome correlation of TR across RVFAC/PASP. Similar to the main analysis, the association of TR with outcome was attenuated with lower RVFAC/PASP.
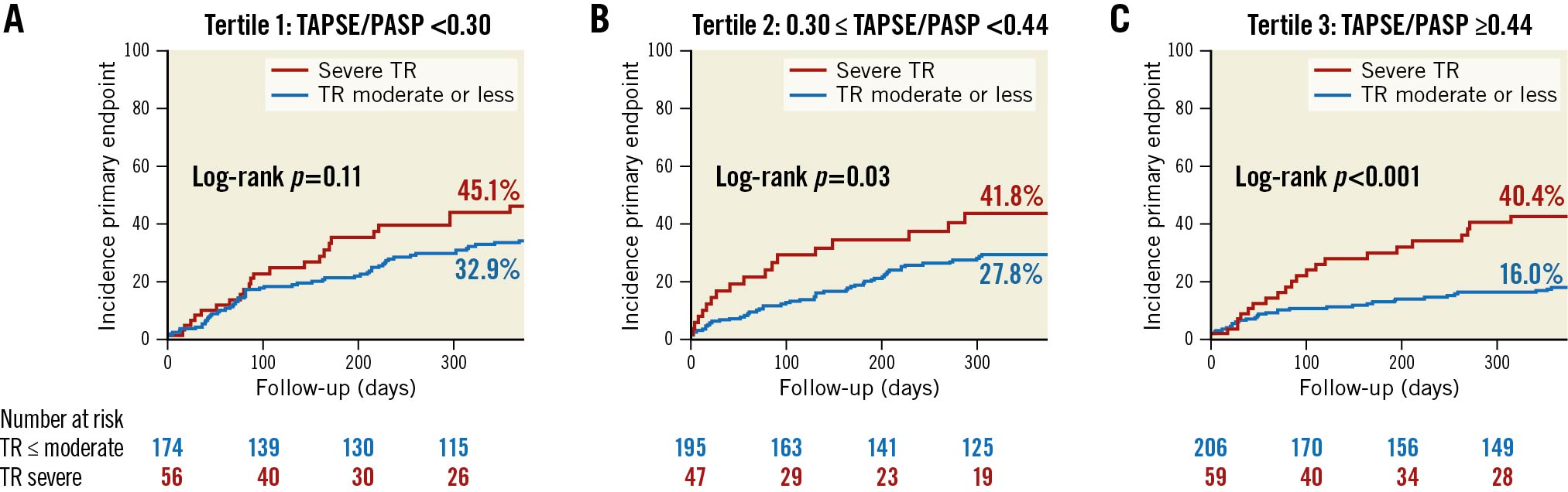
Figure 2. Cumulative incidence of composite outcome between patients with severe TR and TR moderate or less. In the second and third tertile, patients with severe TR had a higher incidence of the primary endpoint than patients with TR moderate or less. Although the association was also observed in the first tertile, the difference did not reach statistical significance. PASP: pulmonary artery systolic pressure; RV-PA: right ventricular-pulmonary artery; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid regurgitation
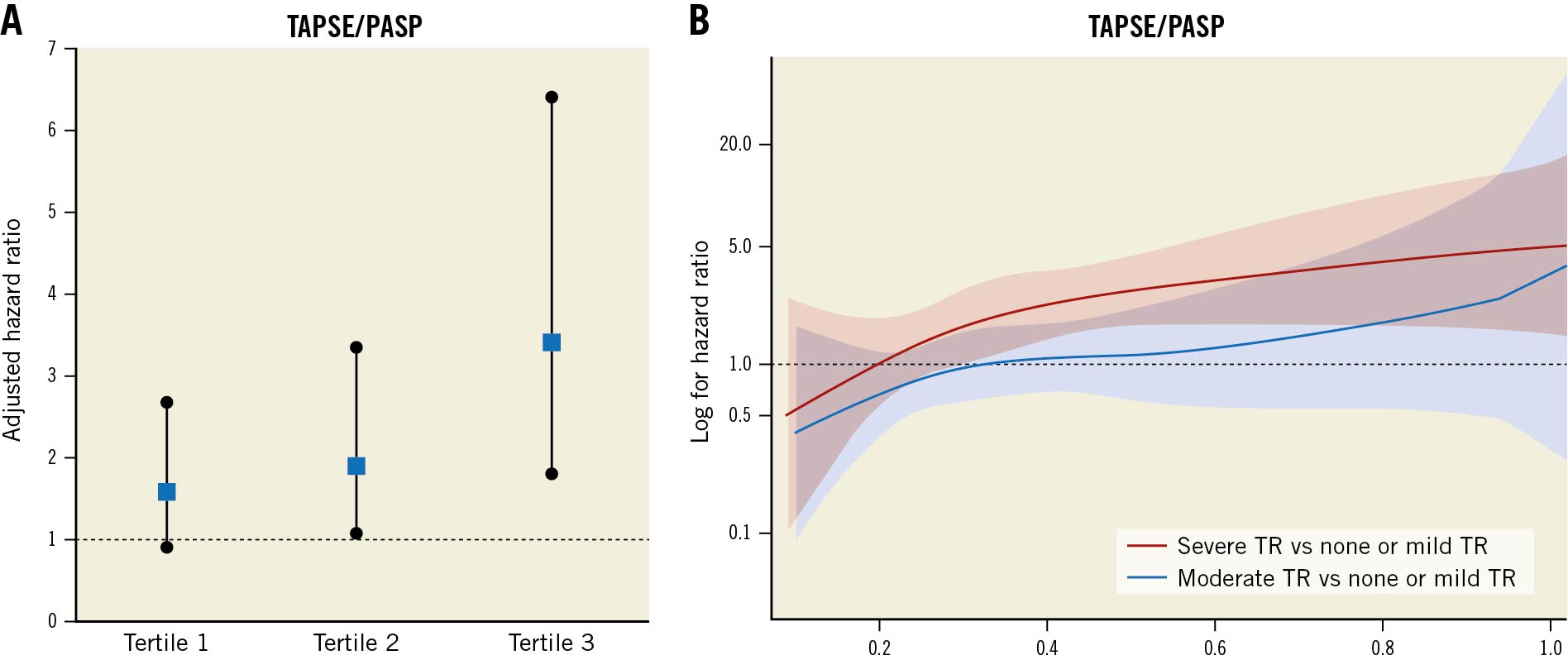
Figure 3. Prognostic impact of TR according to TAPSE/PASP. Forest plot of adjusted HR for TR against the outcome in multivariable regression (A) revealed that the association of TR with outcomes was pronounced in the third tertile (i.e., patients with increased TAPSE/PASP) but attenuated in the first tertile (i.e., patients with decreased TAPSE/PASP). The interaction was also observed in the spline curves depicting the hazard risk of TR according to TAPSE/PASP (B). In addition, the HR of severe TR (red line) was greater than that of moderate TR (blue line), implying that the risk is higher with a higher grade of TR. HR: hazard ratio; PASP: pulmonary artery systolic pressure; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid regurgitation
Additionally, a summary of the mediation analysis is presented in Supplementary Table 2. There was a significant direct effect of TR on the outcome, whereas the indirect effect of TR mediated by TAPSE/PASP was not significant.
Correlation of outcome to tricuspid regurgitation after TEER
After the procedure, data from 637 patients (85.6%) were available to reassess TAPSE/PASP values. Mean TAPSE/PASP was 0.55±0.37, with a significant increase from baseline (p<0.001). Of these, 149 (23.4%) patients had post-procedural severe TR. MR reduction to moderate or less was achieved in 91.9% of patients, with 66.3% of patients having mild or less MR at discharge. In the multivariable model, after adjusting for the predefined baseline and post-procedural covariates (Supplementary Table 3), post-procedural severe TR was associated with an increased risk of the primary endpoint (adjusted HR 1.86, 95% CI 1.25-2.77; p=0.002), which was mainly driven by all-cause mortality (adjusted HR 2.35, 95% CI: 1.38-3.99; p=0.002) (Table 3). With a limited sample size, a similar association was observed for rehospitalisation due to heart failure (adjusted HR 1.56, 95% CI: 0.91-2.70; p=0.11). The association was also examined according to tertile of post-procedural TAPSE/PASP: tertile 1, TAPSE/PASP <0.37 (n=206); tertile 2, 0.37≤ TAPSE/PASP <0.56 (n=217); tertile 3, TAPSE/PASP ≥0.56 (n=214). Similar to the main analysis, the prognostic impact of TR was pronounced in patients with increased TAPSE/PASP but attenuated in those with decreased TAPSE/PASP (interaction term p=0.03) (Table 3, Figure 4).
Table 3. Association of post-procedural severe TR with clinical outcomes after the procedure.
|
Postprocedural severe TR vs moderate or less TR |
Multivariable adjusted HR (95% CI) |
|||
|---|---|---|---|---|
|
All cohort |
Tertile 1 |
Tertile 2 |
Tertile 3 |
|
|
Primary endpoint |
1.86 (1.25-2.77) |
1.47 (0.82-2.62) |
2.04 (0.83-4.99) |
2.68 (1.26-5.69) |
|
All-cause mortality |
2.35 (1.38-3.99) |
1.89 (0.88-4.08) |
1.98 (0.59-6.64) |
3.58 (1.27-10.1) |
|
Rehospitalisation due to heart failure |
1.56 (0.91-2.70) |
0.96 (0.42-2.22) |
1.82 (0.47-7.03) |
2.94 (1.19-7.29) |
|
The models were adjusted for age, sex, atrial fibrillation, coronary artery disease, estimated glomerular filtration rate, logistic EuroSCORE, New York Heart Association Functional Class, post-procedural LV ejection fraction, post-procedural MR, and post-procedural TAPSE/PASP. CI: confidence interval; HR: hazard ratio; TR: tricuspid regurgitation |
||||
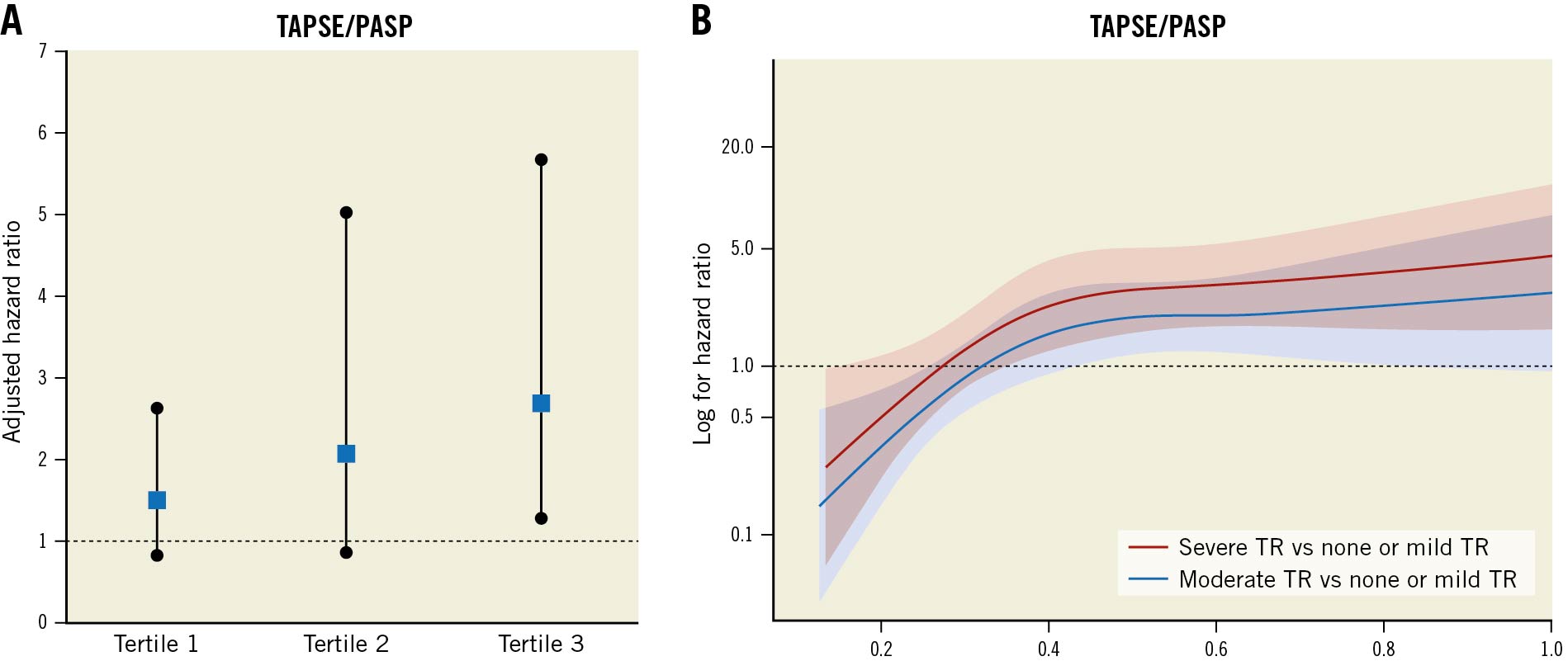
Figure 4. Impact of post-procedural TR on outcomes according to TAPSE/PASP. Similar to the main analysis, there was a significant interaction between outcome of TR and TAPSE/PASP (A). The prognostic impact of TR was attenuated as TAPSE/PASP decreased. The trend was seen in the spline curve analysis, depicting the HR of severe TR (red line) and that of moderate TR (blue line) (B). HR: hazard ratio; PASP: pulmonary artery systolic pressure; TAPSE: tricuspid annular plane systolic excursion; TR: tricuspid regurgitation
Discussion
The present study investigated the prognostic impact of TR according to RV-PA coupling in patients undergoing mitral TEER. The main findings can be summarised as follows:
- Severe TR was associated with mortality and rehospitalisation due to heart failure within 12 months after TEER for MR.
- The prognostic impact of TR varied according to TAPSE/PASP: the association was pronounced in patients with a high TAPSE/PASP ratio but attenuated in patients with a low TAPSE/PASP (i.e., RV-PA uncoupling).
- These findings were consistent across different statistic assumptions, including the analysis using the measurements after TEER.
TR is a common valvular heart disease, with 0.55% of the general population having moderate or severe TR1. In terms of pathophysiology, TR, RV dysfunction, and pulmonary hypertension are linked to each other. In patients with MR, longstanding elevated pulmonary arterial pressure may result in RV longitudinal elongation and spherical deformation, which lead to subsequent tricuspid leaflet tethering and the development of TR4. Also, TR leads to a persistent volume overload for the RV and advances the impairment of RV function. However, it remains uncertain whether TR contributes alone to the dismal outcome or acts in conjunction with RV function.
Our study cohort consisted of patients undergoing TEER for MR, wherein 22.3% of the participants showed severe TR before the intervention. The prevalence of TR was comparable to earlier results (14.0% to 21.8%)1314. Furthermore, a reduction in MR to moderate or less was achieved in 91.9% of patients, with 66.3% of patients having mild or less MR at discharge. This rate was comparable to earlier studies but slightly lower than what was reported in most recent investigations of the latest iteration of TEER devices151617. Since the severity of MR may affect the study inference, a sensitivity analysis was conducted using the post-procedural covariables.
For the assessment of RV function, we used the concept of RV-PA coupling assessed by TAPSE/PASP. The concept has been initially valid for patients with pulmonary hypertension18 but has also recently been applied to various patient cohorts719202122. The coupling of this measurement indicates that RV systolic function can compensate for an increased afterload (i.e., pulmonary artery pressure). In contrast, a decreased TAPSE/PASP, namely RV-PA uncoupling, suggests that RV systolic function cannot compensate for the afterload. More recently, Brener et al and Karam et al have collectively reported that RV-PA coupling was a strong predictor of outcomes in patients with heart failure and MR57. However, little is known about the interaction of the clinical impact of RV-PA coupling and TR, despite their pathophysiological interaction.
In the present study, TR was associated with the risk of mortality or hospitalisation due to heart failure, but the outcome correlation of TR changed according to RV-PA coupling assessed by TAPSE/PASP. The prognostic impact of TR was more pronounced in patients with increased TAPSE/PASP (i.e., RV-PA coupling) but attenuated in patients with reduced TAPSE/PASP (i.e., RV-PA uncoupling). The finding was consistent both at baseline and after the procedure. Also, a spline curve shows the interaction between the prognostic impact of TR and TAPSE/PASP. One of the contributing factors to the interaction between TR and TAPSE/PASP could be that a severely impaired RV function can worsen clinical prognosis5. Lurz et al reported that decreased TAPSE/PASP remained to be an independent factor associated with outcomes after a transcatheter treatment for TR10, implying that severely impaired RV function might be a predominant prognostic factor in those populations. Another possible explanation for the interaction might be a mediation effect by RV function. Concomitant impaired RV function may mediate the prognostic impact of TR. However, our mediation analysis did not find a significant mediation effect of TR, through RV function, that was linked to the outcomes. Also, concomitant cardiac comorbidities (e.g., impaired LV systolic function or the presence of coronary artery disease) may play an essential role as risk indicators of the outcome23, which might lower the clinical significance of TR.
Our findings do not entirely align with previous knowledge. A cohort study investigating patients with reduced LV ejection fraction reported that the outcome correlation with TR remained significant even after adjusting for RV dysfunction as a categorical variable12. Their study was conducted in the early 2000s, implying that the guideline-directed medical therapies differed from the current cohort. A large observational study reported that the prognostic impact of severe TR in patients with degenerative MR was irrespective of the presence of RV dysfunction ≥moderate24. We delved into the interaction by applying an afterload-corrected RV function (i.e., TAPSE/PASP) as a categorical and as a continuous variable, which could account for the differing results.
In clinical decision-making for TR, the principal issue is to determine if the TR should be treated to curb a dismal clinical prognosis. Identifying the subjects who would benefit from a tricuspid intervention is essential to obtain the optimal therapeutic strategy in each individual. We found that the clinical impact of TR changed according to RV-PA coupling. Notably, the spline curve of the severe TR was found to be left-upwards compared to moderate TR, implying that the risk is higher with a higher grade of TR. Thus, a novel conceptual framework could be suggested. The prognostic impact of TR is determined by two critical factors (i.e., the severity of TR and RV-PA coupling) (Central illustration), as the severity of MR and LV function are on the mitral side. The impact of transcatheter TR treatment on outcomes might vary according to the severity of TR and RV function (e.g., RV-PA coupling). A multicentre cohort study reported that there was no outcome benefit of transcatheter tricuspid therapy over medical therapy alone in patients with TR and severely impaired RV function25. In contrast, patients with preserved RV function assessed by RV-PA coupling may be more likely to benefit from transcatheter tricuspid treatment19.
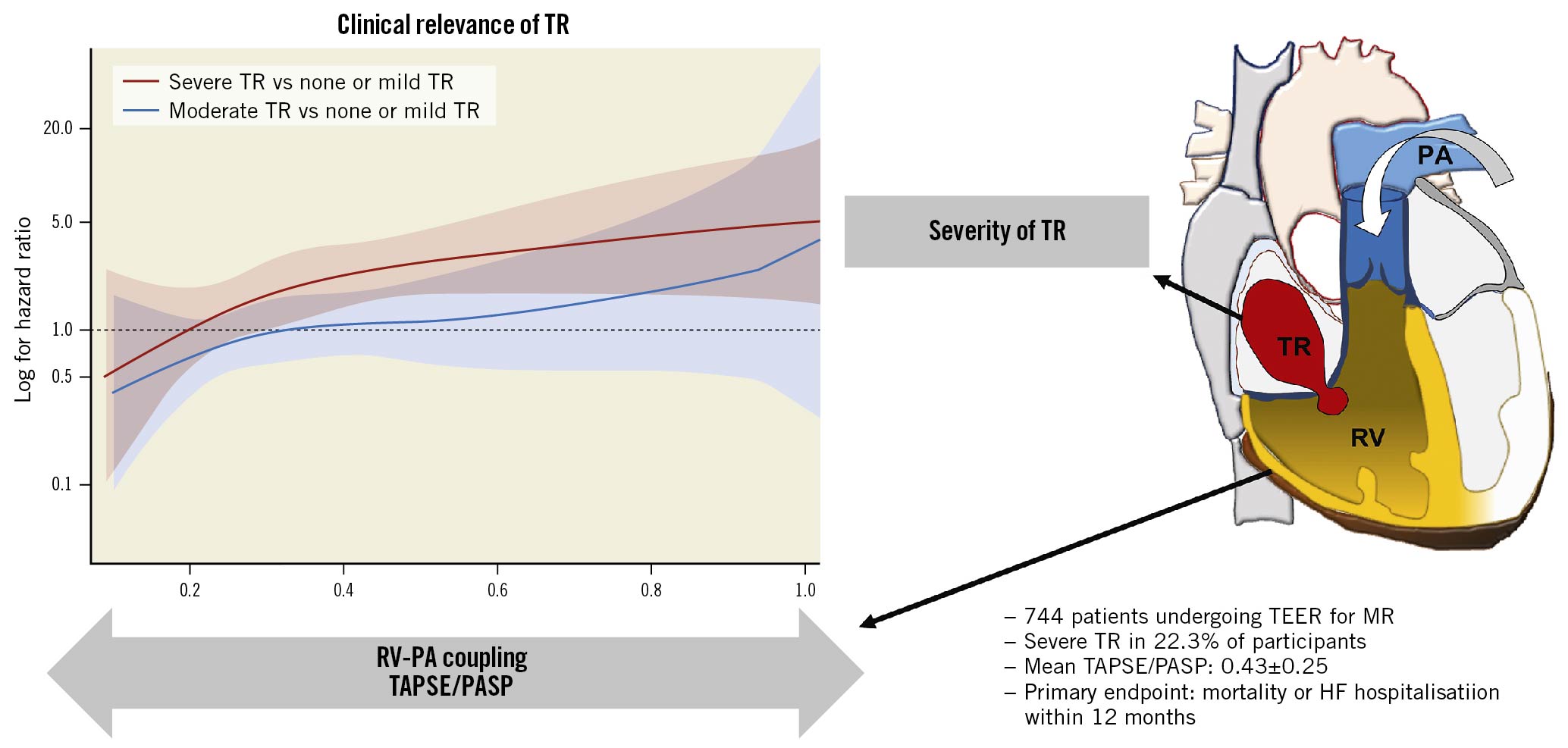
Central Illustration. Impact of right ventricular-pulmonary arterial coupling on outcomes of TR. TR is a strong predictor of all-cause mortality and rehospitalisation due to heart failure in patients undergoing mitral TEER. The risk is higher with a higher grade of TR. Besides, RV-PA coupling is also associated with the outcome. Moreover, RV-PA coupling affects the outcome correlation of TR. The prognostic impact of TR is pronounced in patients with a high TAPSE/PASP ratio but attenuated in patients with a low TAPSE/PASP (i.e., RV-PA uncoupling). HF: heart failure; HR: hazard risk; MR: mitral regurgitation; PASP: pulmonary artery systolic pressure; RV-PA: right ventricular pulmonary artery; TAPSE: tricuspid annular plane systolic excursion; TEER: mitral transcatheter edge-to-edge repair; TR: tricuspid regurgitation
Limitations
Several limitations should be acknowledged. First, core lab adjudicated echocardiographic assessments are lacking. The assessment and grading of the TR severity are challenging in clinical practice. Although both qualitative and quantitative parameters were used to assess TR severity, as recommended in the guidelines89, further investigations with a core lab analysis are needed to validate our preliminary findings. Second, TR and RV function might have changed in the interval between echocardiography and TEER. Nevertheless, the primary findings of the current study were consistent in the sensitivity analyses using post-procedural parameters, which would validate the study inference. Third, there was no haemodynamic data obtained by the right heart catheter. PASP might be underestimated in some patients due to a large coaptation gap and severe TR. Nonetheless, 2D echocardiography is the most widely used imaging technique to measure these parameters in clinical practice. Still, our preliminary findings need to be validated in large-scale studies with invasively measured PASP. Finally, we did not assess additional interventions to treat TR during the follow-up period. Our findings could serve as a basis in further investigations to look at the prognostic impact of treating TR with regard to the two parameters (i.e., the severity of TR, RV-PA coupling).
Conclusions
TR is a strong predictor of all-cause mortality and rehospitalisation due to heart failure in patients undergoing mitral TEER. The risk is higher with a higher grade of TR. Besides, RV-PA coupling is also associated with the outcome. Moreover, RV-PA coupling affects the outcome correlation of TR. The prognostic impact of TR is pronounced in patients with a high TAPSE/PASP ratio but attenuated in patients with a low TAPSE/PASP (i.e., RV-PA uncoupling). Our findings propose a novel conceptual framework: the clinical relevance of TR will be determined according to its severity and concomitant RV-PA coupling ratio. Further investigations are needed to investigate the prognostic impact of transcatheter TR treatment with regard to these two parameters.
Impact on daily practice
TR is a strong predictor of all-cause mortality and rehospitalisation due to heart failure in patients undergoing mitral TEER. Besides, RV-PA coupling is also associated with the outcome. Moreover, RV-PA coupling affects the outcome correlation of TR. The prognostic impact of TR is pronounced in patients with a high TAPSE/PASP ratio but attenuated in patients with a low TAPSE/PASP (i.e., RV-PA uncoupling). Our findings propose a novel conceptual framework: the clinical relevance of TR will be determined according to its severity and concomitant RV-PA coupling ratio.
Acknowledgements
We thank Dr. Meghan Lucas (scientific coordinator for the Heart Center Bonn, Bonn, Germany) for proofreading the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
G. Nickenig and S. Baldus have received research grants and speaker honoraria from Abbott, outside the submitted work. R. Pfister and C. Iliadis have received travel support by Abbott, outside the submitted work. All other authors have no conflicts of interests to declare with regard to this paper.
Supplementary data
To read the full content of this article, please download the PDF.