Abstract
Background: Tricuspid regurgitation (TR) has a poor prognosis and limited treatment options and is frequently accompanied by right ventricular (RV) dysfunction. Transcatheter tricuspid valve interventions (TTVI) to reduce TR have been shown to be safe and feasible with encouraging early results. Patient selection for TTVI remains challenging, with the role of right ventricular (RV) function being unknown.
Aims: The aims of this study were 1) to investigate survival in a TTVI-treated patient population and a conservatively treated TR population, and 2) to evaluate the outcome of TTVI as compared to conservative treatment stratified according to the degree of RV function.
Methods: We studied 684 patients from the multicentre TriValve cohort (TTVI cohort) and compared them to 914 conservatively treated patients from two tertiary care centres. Propensity matching identified 213 pairs of patients with severe TR. As we observed a non-linear relationship of RV function and TTVI outcome, we stratified patients according to tricuspid annular plane systolic excursion (TAPSE) to preserved (TAPSE >17 mm), mid-range (TAPSE 13-17 mm) and reduced (TAPSE <13 mm) RV function. The primary outcome was one-year all-cause mortality.
Results: TTVI was associated with a survival benefit in patients with severe TR when compared to matched controls (one-year mortality rate: 13.1% vs 25.8%; p=0.031). Of the three RV subgroups, only in patients with mid-range RV function was TTVI associated with an improved survival (p log-rank 0.004). In these patients, procedural success was associated with a reduced hazard ratio for all-cause mortality (HR 0.22; 95% CI: 0.09, 0.57).
Conclusions: TTVI is associated with reduced mortality compared to conservative therapy and might exert its highest treatment effect in patients with mid-range reduced RV function.
Introduction
Tricuspid regurgitation (TR) is experiencing growing recognition as a public health concern with major effects on morbidity and mortality owing to its propagation of right heart failure (HF)1,2. Mortality for isolated tricuspid valve surgery remains higher than for any other single heart valve surgery, ranging between 8 and 10% in contemporary cohorts3,4,5. Transcatheter tricuspid valve intervention (TTVI) is a rapidly evolving treatment option for severe TR, currently under clinical investigation. TTVI has been performed on a compassionate use basis, in patients at high or prohibitive surgical risk, with a range of systems6,7,8,9,10,11,12,13. However, TTVI is still developing, and the role of the procedure and appropriate patient selection remains inconclusively defined.
Prior evidence revealed an association of TTVI with improved survival in patients with symptomatic severe TR in comparison with conservatively managed patients14,15. As TTVI is lacking randomised controlled trial data, these large registries are integral to our understanding of the factors contributing to procedural risk and post-procedural adverse events as well as the identification of subgroups within the TR population where TTVI may be beneficial or futile.
The presence of right ventricular dysfunction (RVD) is a recognised risk factor associated with adverse outcome in the general population16, in patients with TR17 and in tricuspid valve surgery18. However, the clinical impact of RVD in patients undergoing TTVI has not been comprehensively evaluated.
The aims of this study were:
– To investigate survival in a TTVI-treated patient population from the prospective multicentre TriValve registry and a conservatively treated TR population from two tertiary care centres.
– To evaluate the outcome of TTVI as compared to conservative treatment stratified according to the degree of RV function.
Methods
STUDY POPULATION – TTVI COHORT
The patient population consisted of 684 consecutive patients with symptomatic significant TR undergoing TTVI from September 2014 to January 2020, after enrolment into the International Multisite Transcatheter Tricuspid Valve Therapies Registry (TriValve registry; NCT03416166). This multicentre registry includes 21 heart centres across Europe and North America. A comprehensive description of the TriValve registry has been reported previously19. All patients were symptomatic with signs of heart failure. The majority of patients were in New York Heart Association (NYHA) functional classes III or IV. TR therapy was indicated in accordance with international guidelines20,21. Heart Team consensus rendered all patients at high or prohibitive surgical risk. TTVI was conducted on an off-label or compassionate use basis. Caval valve implantations (CAVI) were excluded from this study.
STUDY POPULATION - CONSERVATIVELY TREATED TR COHORT
Consecutive patients with severe TR were evaluated at the Charité Medical University, Campus Charité Mitte and Benjamin Franklin, Berlin, Germany, between 2010 and 2017. Patients with ≥severe TR (on a four-grade scale as described before22) and with a functional TR aetiology were retrospectively identified. The collection of retrospective data and the inclusion of patients in this study were approved by the local institutional review board. All patients received guideline-directed medical therapy. Follow-up was obtained by contacting the local registration offices. The primary outcome was all-cause mortality. Both study cohorts and the investigation conform with the principles outlined in the Declaration of Helsinki.
DEVICE AND PROCEDURE
The TTVI procedures were performed using the MitraClip® (Abbott Vascular, Santa Clara, CA, USA), Trialign™ (Mitralign Inc., Tewksbury, MA, USA), Cardioband™, FORMA, PASCAL (Edwards Lifesciences, Irvine, CA, USA), TriCinch System™ (4Tech, Galway, Ireland), and GATE™ (NaviGate Cardiac Structures, Lake Forest, CA, USA) device. Technical aspects of each devices have already been reported in detail6,7,8,9,10,11,12,13.
PATIENT DATA
In the TriValve registry, clinical and echocardiographic baseline and follow-up data were prospectively collected. Clinical follow-up was carried out by clinical visits and/or phone consultation at 30 days, 6 months, and one year, and annually thereafter. The inclusion of patients in this study was approved in each centre by a local ethics committee or per local practice for clinical data collection.
DEFINITIONS
All patients included in the TTVI study had symptomatic at least severe TR. Transcatheter therapy was conducted on an off-label or compassionate use basis after interdisciplinary Heart Team evaluation. Grading of TR severity was assessed according to a combination of semiquantitative and quantitative parameters, as recommended by the American Society of Echocardiography23 and European Association of Echocardiography guidelines24, and extended by a fourth grade22. RV function was qualitatively assessed in the apical four-chamber view and quantified by tricuspid annular plane systolic excursion (TAPSE).
Procedural success was defined as a device successfully implanted and delivery system retrieved, with a residual TR grade ≤2. Mitral Valve Academic Research Consortium criteria were used to define adverse events25.
ENDPOINTS
The primary endpoint was defined as the incidence of all-cause mortality within one year of follow-up in the matched population.
STATISTICAL ANALYSIS
Patients in the TTVI cohort were matched with conservatively managed patients using propensity scores. The following variables were used for the calculation of propensity scores: TAPSE, age, EuroSCORE II, estimated glomerular filtration rate (eGFR), left ventricular ejection fraction (LVEF), left ventricular end-diastolic diameter (LVEDD), echocardiographically determined systolic pulmonary artery pressure (sPAP), haemodialysis, New York Heart Association (NYHA) class (binary class I and II vs III and IV), presence of atrial fibrillation/flutter and NT-proBNP. Based on these propensity scores, TTVI-treated patients were matched 1:1 with control patients randomly selected from the control pool of patients defined by the parameters using the nearest neighbour rule of ±0.2 standard deviations. The balance between the groups of patients with TTVI and controls was assessed by standardised differences (defined as the difference in means or proportions divided by the mutual standard deviation). Standardised differences below 0.1 were considered not significant.
Continuous data are presented as means and standard deviations for parametric data or medians with interquartile range (IQR) for non-parametric data. The normality assumption was evaluated using the Kolmogorov-Smirnov test. Statistical comparisons were conducted by the Mann-Whitney U test for two-group comparisons and the chi-square test or Kruskal-Wallis test for multi-group analyses. For repeated measurements of non-parametric data, the Wilcoxon signed-rank test was used.
The primary endpoint was analysed using Kaplan-Meier estimates and the log-rank test was applied for group comparisons.
We stratified patients according to their TAPSE into quintiles and performed separate Cox regression analyses to obtain hazard ratios for survival comparing TTVI with conservative treatment. The hazard ratios and their 95% confidence bands were fitted in cubic non-linear curves. Due to a non-linear association of TTVI with all-cause mortality in relationship with TAPSE, we stratified patients according to RV function into three groups with respective preserved (TAPSE >17 mm), mid-range (TAPSE 13-17 mm) and reduced (TAPSE <13 mm) function. This stratification was based on identification of the TAPSE quintiles with the lowest p-value and their corresponding borders.
Cox regression analyses were carried out to identify predictors for the occurrence of one-year survival in patients with mid-range RVD. The proportionality of hazards assumption was confirmed for all Cox models.
A two-sided p-value <0.050 was considered statistically significant. Kaplan-Meier curves were created with GraphPad Prism 8.0 (GraphPad Software Inc, San Diego, CA, USA). All statistical analyses were performed with SPSS, Version 25 (IBM Corp., Armonk, NY, USA).
Results
STUDY POPULATION AND CHARACTERISTICS OF THE PROPENSITY-MATCHED COHORTS
We combined 684 patients from the TriValve registry with 914 patients from a registry of conservatively managed patients with severe TR from Charité/Berlin for a total of 1,598 patients. After exclusion of cases for lack of reported TAPSE, age, EuroSCORE II, eGFR, LVEF, LVEDD, sPAP, haemodialysis, NYHA class, presence of atrial fibrillation/flutter, NT-proBNP, follow-up below 31 days without an event, or non-functional aetiology, 850 patients were included in the analysis (Supplementary Figure 1). Baseline characteristics by conservative versus interventional treatment are shown in Table 1. Patients in the unmatched TTVI cohort had significantly higher age, EuroSCORE II, higher rates of atrial fibrillation, higher LVEF, larger LVEDD and lower rates of haemodialysis, TAPSE, lower proportion of mitral regurgitation (MR) ≥grade 3 and sPAP as compared to the unmatched conservatively treated cohort (all p<0.050).
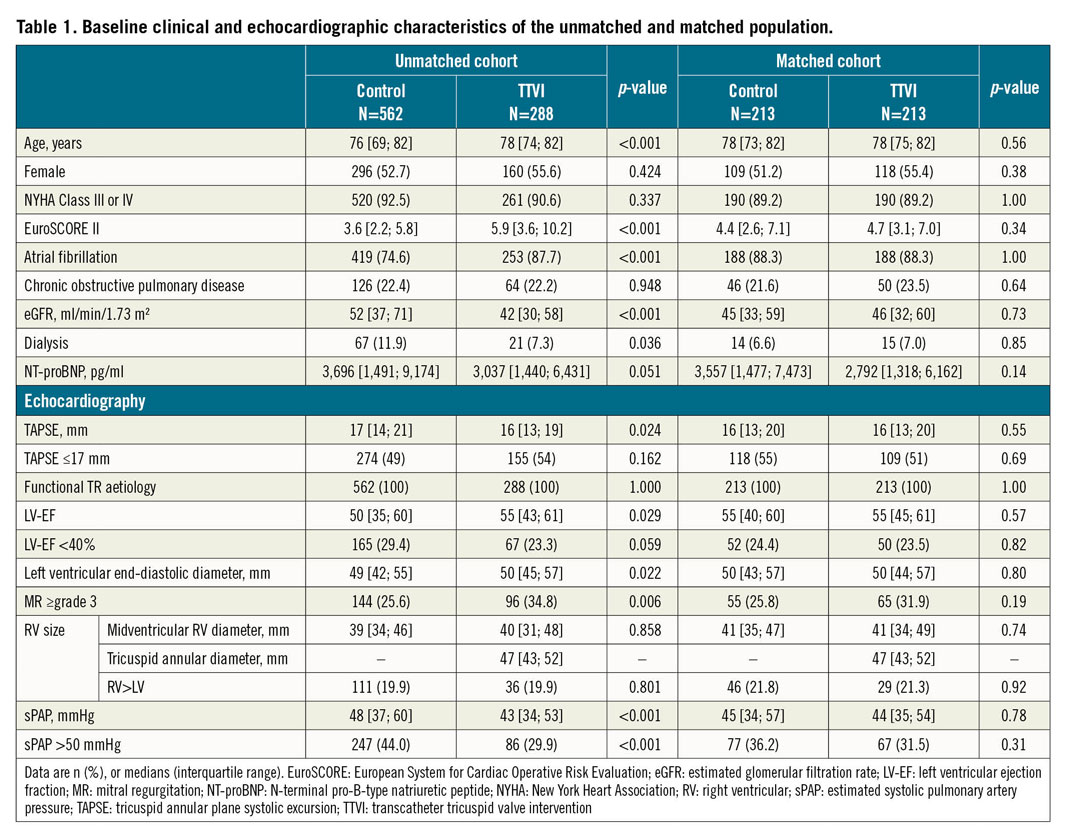
Propensity score matching identified 213 pairs of matched patients for a total of 426 patients. Baseline characteristics of the matched cohorts are shown in Table 1. No significant differences between unmatched and matched patients were observed (Table 1, Supplementary Figure 2).
In the matched TTVI cohort, procedural success was achieved in 167 patients (80.7%). Overall, 54 (32.9%) had concomitant mitral procedures for significant left-sided valve disease (MitraClip in all cases). The MitraClip system was predominantly used for TTVI (n=192 [90.0%]) (Supplementary Table 1).
TRANSCATHETER VERSUS CONSERVATIVE TREATMENT FOR SEVERE TR
In the matched cohort, the estimated mortality rate after one year was 25.4% in the conservatively treated cohort and 13.1% in the TTVI cohort (p=0.031) (Figure 1A). Mortality was significantly reduced in patients with successful TTVI as compared to conservatively managed patients (p=0.007) (Figure 1B), but not in patients with procedural failure when compared to conservatively treated patients (Figure 1B). In isolated TTVI, the one-year mortality rate was also significantly lower in the matched TTVI cohort when compared to either conservative treatment or conservative treatment without MR ≥grade 3 (p=0.001 and p=0.006, respectively) (Figure 1C).
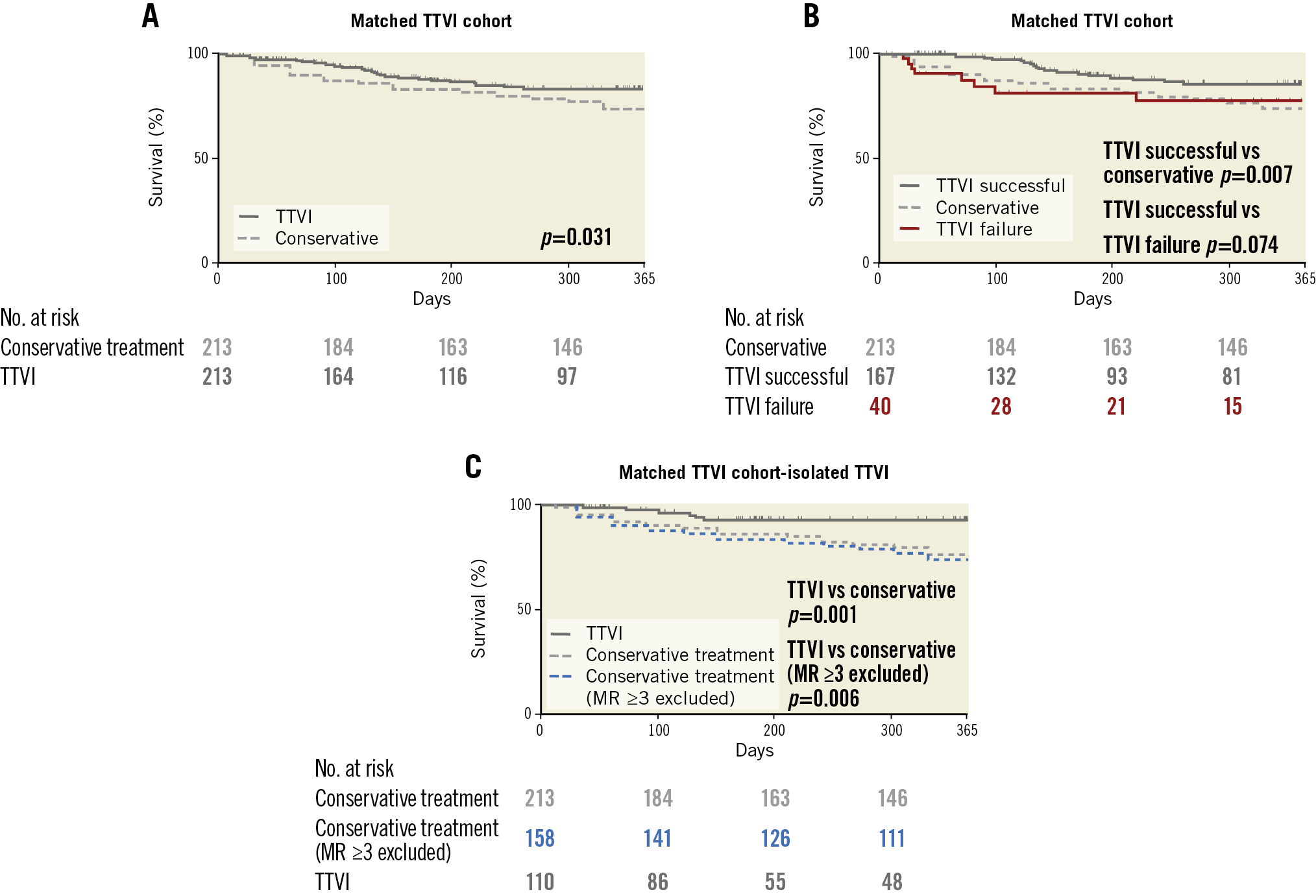
Figure 1. Reduced mortality after transcatheter tricuspid valve intervention (TTVI) compared to conservative treatment. A) Survival in patients after TTVI or conservative treatment in the propensity score-matched cohort. Kaplan-Meier analysis; N=426; p for log-rank test. B) Kaplan- Meier analysis for survival in patients after TTVI at one year stratified for procedural success in the propensity score-matched TTVI cohort. N=420; p for log-rank test. C) Survival in patients after TTVI or conservative treatment (patients with MR ≥grade 3 excluded) in the propensity score-matched cohort. Kaplan-Meier analysis; N=268; p for log-rank test.
RELATIONSHIP BETWEEN RVD AND TTVI OUTCOME
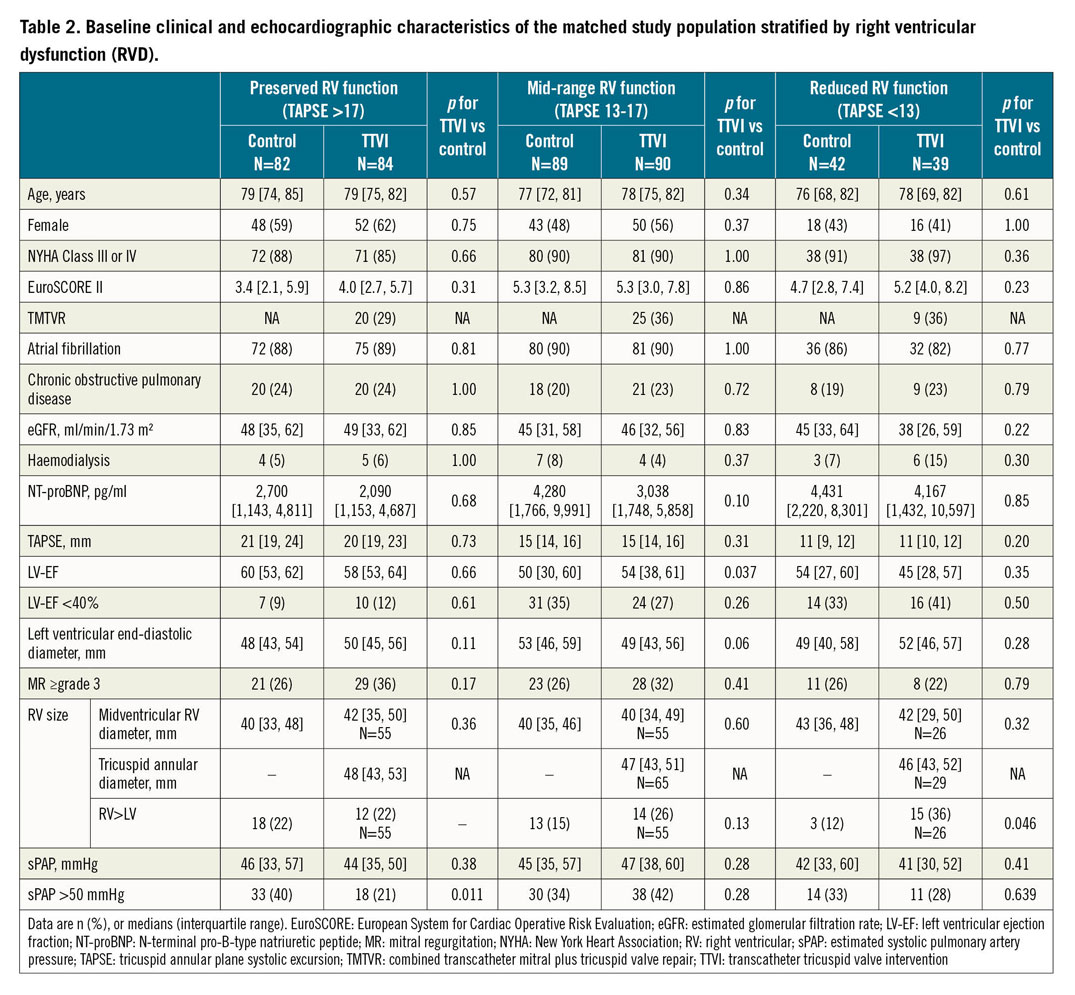
We observed a non-linear relationship of the prognostic impact of TTVI with TAPSE (Central illustration, top panel). Overall, 166 patients had preserved, 179 mid-range reduced and 81 reduced RV function, with no significant difference between TTVI and conservative therapy (p>0.05 for all). There were no significant differences between TTVI and control patients in the respective subgroups except for a clinically irrelevant lower LVEF in the control cohort in the mid-range RV function group and slightly higher rates of RV >LV size in TTVI patients in the reduced RV function group (Table 2).
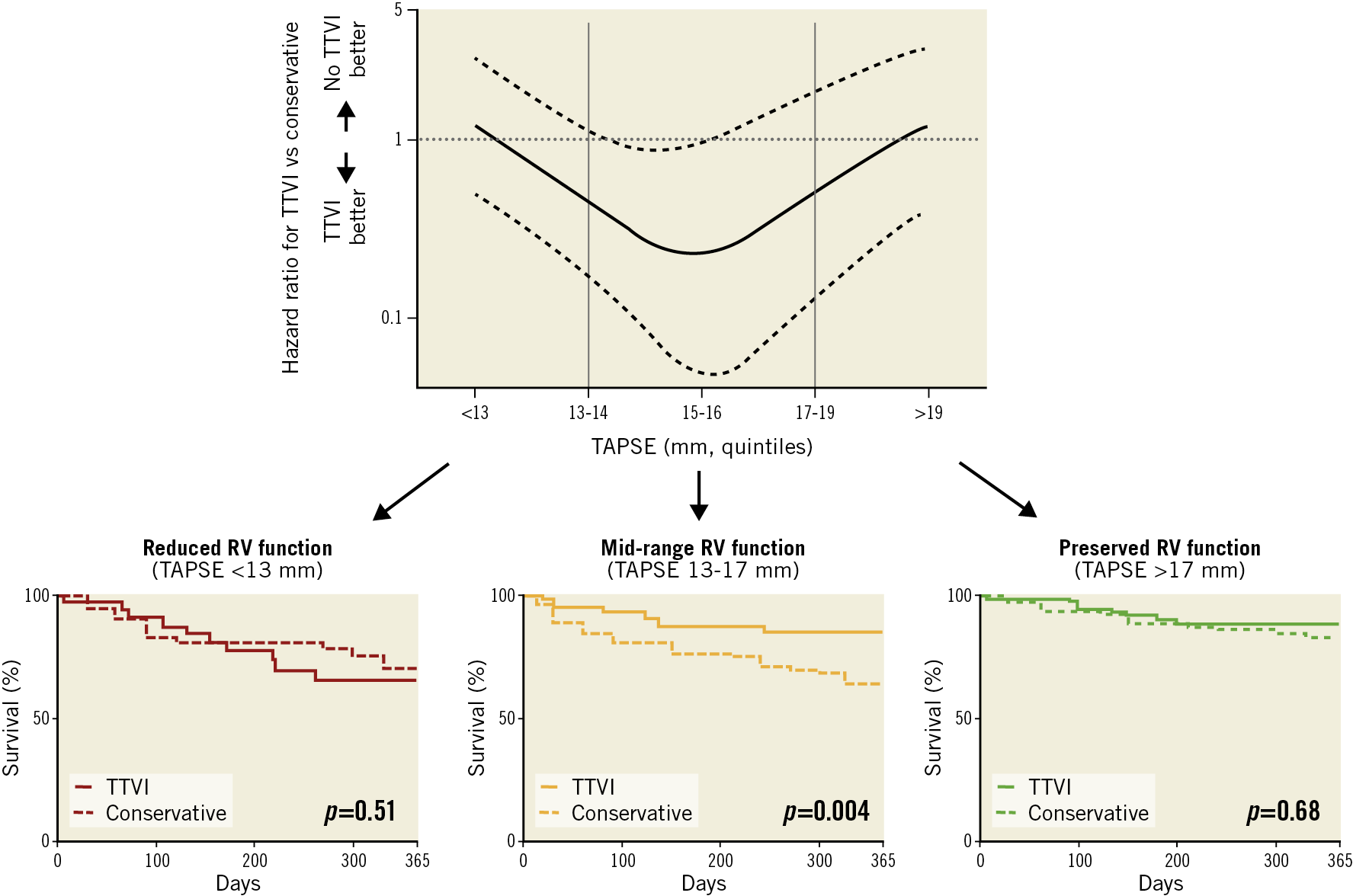
Central illustration. Reduced mortality after transcatheter tricuspid valve intervention (TTVI) compared to conservative treatment in patients with mid-range right ventricular (RV) function. Top panel. Hazard ratio for TTVI versus conservative treatment per tricuspid annular plane systolic excursion (TAPSE) quintile. Curve interpolation by polynomial function. Dotted lines represent 95% CI. Lower panels. Survival in patients with reduced, mid-range and preserved RV function at one year in the propensity score-matched cohort. Kaplan-Meier analysis; N=166, N=179, N=81, respectively; p for log-rank test.
In patients with mid-range RV function, TTVI was associated with a survival benefit when compared to conservative therapy, while there was no survival benefit in patients with preserved or reduced RV function (Central illustration, lower panels).
In patients undergoing TTVI or conservative therapy, reduced RV function was associated with impaired outcome (p log-rank 0.032 and 0.020, respectively) (Figure 2A, Figure 2B). In TTVI patients, interventional TR treatment improved outcome of patients with mid-range RV function to the level of patients with preserved RV function (Figure 2B).
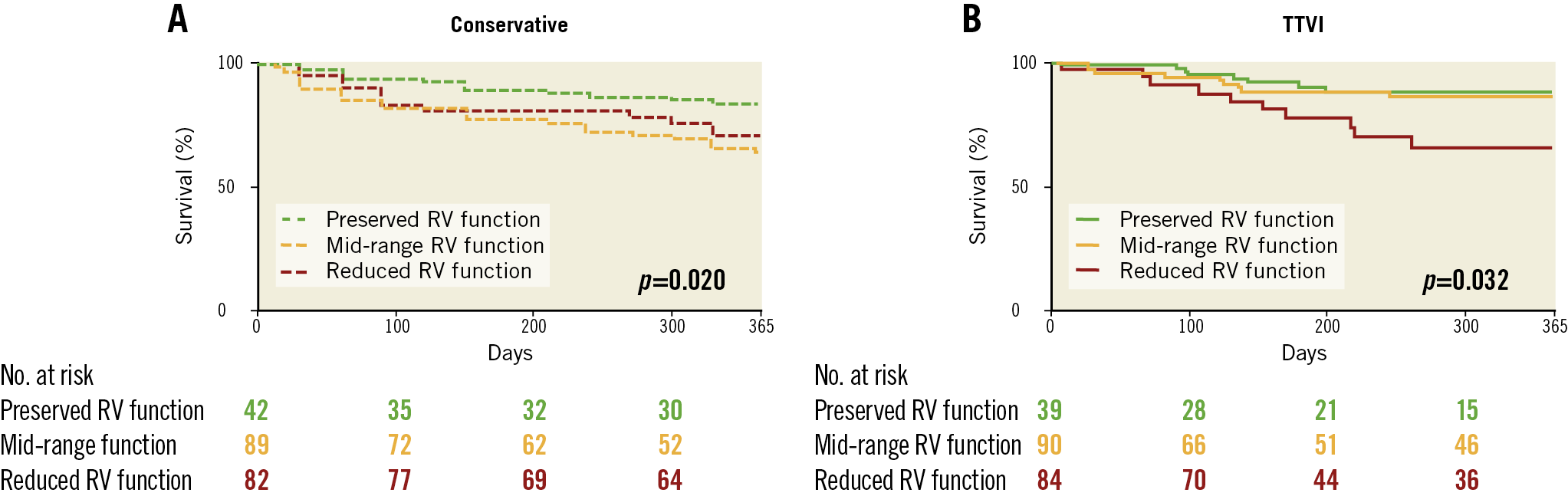
Figure 2. Increased mortality in reduced right ventricular (RV) function in conservatively treated tricuspid regurgitation (TR) and after transcatheter tricuspid valve intervention (TTVI). A) Survival in patients after conservative treatment in the propensity-matched cohort stratified by RV function. Kaplan-Meier analysis; N=213; p for log-rank test. B) Kaplan-Meier analysis for survival in patients after TTVI at one year stratified for RV function. N=213; p for log-rank test.
In patients with mid-range RV function, procedural success, EuroSCORE II, LVEF <40%, NT-proBNP and eGFR were associated with all-cause mortality. However, on multivariable analysis, only procedural success (HR 0.22; 95% CI: 0.09, 0.57) and EuroSCORE II (HR 1.10; 95% CI: 1.01, 1.20) remained independent predictors of an adverse outcome in this patient population (Supplementary Table 2). Rates of procedural success and post-procedural TR were not statistically different among patients with preserved, mid-range or reduced RV function (Supplementary Table 3).
Discussion
Our study is the first to analyse comprehensively the role of RV function in TTVI as compared to conservative therapy in a large cohort (n=426) of 1:1 propensity-matched patients with severe functional TR. Specific findings include: when compared to matched controls treated conservatively, TTVI shows a survival benefit in patients with severe TR; TTVI improves one-year survival in a non-linear fashion according to RV function with the highest observable treatment benefits among patients with mid-range RV function.
In the absence of randomised controlled trials, propensity score matching offers a valuable tool to glean information from a matched cohort analysis. One such analysis with propensity matching for age, EuroSCORE and pulmonary artery pressure has been performed for TTVI, using a registry of interventions and two large cohort studies15. In that study, TTVI was associated with improved survival and reduced HF hospitalisation compared with medical therapy15. Our current analysis utilised an expanded TriValve registry and data from two different tertiary care centres. The two studies thus differ in the patient populations studied. Compared to the current study, the control cohort in the study by Taramasso et al15 had a lower incidence of RVD (29% vs 55%) and NYHA Classes III and IV (23% vs 89%). Compared to their respective controls, TTVI patients in the study by Taramasso et al had a higher incidence of RVD, NYHA Class III/IV, mitral regurgitation >2+, atrial fibrillation and pacemaker/defibrillators. In our study, the matching equalised the differences in baseline variables. Despite the differences in comorbidity burden and completely separate control cohorts, both studies found a consistent association of TTVI with improved clinical outcomes compared to medically managed controls.
Right ventricular dysfunction is a frequent finding in significant TR, as changes in RV morphology influence ventricular performance and valvular geometry alike. The interplay between RV function and TR remains incompletely understood. While data on the role of RV function in TR are emerging17, the role of RV function in TTVI is largely undefined, with a suggestion of poorer RV function associated with worse outcomes in small case studies12. In contrast, Karam et al reported similar outcomes of TTVI in patients stratified according to TAPSE26. These conflicting results and the lack of comparative outcomes of conservative treatment complicate the use of RV function as either a clinical selection criterion for TTVI or as a subgroup analysis for the interpretation of TTVI results.
This is the first study to evaluate specifically the role of RV function for TTVI outcome by comparing results of TTVI with conservative treatment in patients with different degrees of RVD. Importantly, we now demonstrate a U-shaped relationship of RV function and potential benefits of TTVI as compared to conservative treatment. Only by appreciation of this non-linear relationship and the comparison of TTVI to conservative treatment can the previous controversy about the prognostic value of RV function in TR and TTVI be understood. Mid-range RV function is associated with impaired outcome in conservatively treated patients (Figure 2A), but not in TTVI patients, which is explained by the finding that TTVI improved survival in mid-range RV function patients to the level of patients with preserved RV function (Figure 2B). Consequently, the treatment effect of TTVI diminishes the prognostic value of mid-range RV function.
The greatest survival benefit of TTVI in the mid-range TAPSE group suggests that clinical benefit may be highest in patients at the onset of RVD. It has been speculated that the improved survival may in part be due to breaking the vicious circle of volume overload mediated RV remodelling and dysfunction caused by TR15,27. We hypothesise that the reduction of venous congestion after TTVI may be a function of the RV’s potential to undergo reverse remodelling, ultimately impacting on clinical events. This might be less reversible in patients presenting at a late stage of the disease with a TAPSE <13, possibly explaining the comparable one-year survival as compared to conservative treatment. In contrast, patients with normal RV function might present too early to detect a survival difference with a limited follow-up of one year, given the overall low mortality rate in this RV function subgroup. Longer follow-up could reveal differences in outcomes in this subgroup.
However, this study cannot draw conclusions on the effects of TTVI on heart failure hospitalisations in comparison to the matched cohort as no heart failure hospitalisation follow-up data were available in the matched cohort. Therefore, we cannot exclude that patients with preserved or reduced RV function might not benefit from TTVI, but rather we can state that the treatment effect is smaller as compared to patients with mid-range RV function. Therefore, larger trials will be necessary to identify relevant changes in mortality. Nonetheless, in these early stages of TTVI trial design, patients with mid-range RV function should be considered an important target subgroup for treatment. Given our limited understanding of RV function assessment and recovery, patients with RVD deserve further study. In addition, future trials should provide data on the performance of TTVI versus surgical repair and the role of RVD in this comparison.
Limitations
Matched cohort studies may still be subject to bias from unidentified confounders, and timing of diagnosis and treatment initiation relative to registry inclusion may play a role; therefore, the results must be interpreted with caution. As data on the concomitant treatment of tricuspid and mitral valve regurgitation are promising28,29, our analysis also includes cases with transcatheter mitral and tricuspid valve intervention (TMTVR). Since the majority of patients with concomitant significant MR underwent TMTVR, we accounted for this by excluding cases with significant MR from the control group in individual sub-analyses that evaluated isolated TTVI procedures to address selection bias. The effect size and statistical significance of TTVI versus control in isolated TTVI procedures were not altered by excluding significant MR. However, selection bias cannot be fully excluded.
As discussed previously, outcome considered survival only; results might differ with respect to rates of hospitalisation and symptomatic outcome.
Although TAPSE is easily evaluated and is a robust parameter owing to its high degree of reproducibility30, there was no central echocardiographic core laboratory involved.
Inclusion of additional parameters for the evaluation of RV function would have been desirable31. TAPSE is influenced by afterload and probe angulation, as well as the degree of TR itself, as it may lead to pseudonormalisation. Speckle tracking or 3D-RV parameters for the evaluation of RVD could be implemented in future trial protocols.
Conclusions
TTVI is associated with reduced mortality compared to conservative therapy and might exert its highest treatment effect in patients with mid-range RV function.
|
Impact on daily practice TTVI is associated with reduced mortality compared to conservative therapy in a propensity-matched cohort study and might exert its highest treatment effect in patients with mid-range reduced RV function. RV function should be assessed as part of the evaluation before interventional tricuspid valve therapies and should be included in the design of future randomised trials. |
Conflict of interest statement
M. Miura is a consultant for Japan Lifeline. G.H.L. Tang reports personal fees from Abbott Structural Heart outside the submitted work. J. Rodès-Cabau reports grants and personal fees from Edwards Lifesciences, personal fees from NaviGate Cardiac Structures Inc. outside the submitted work. D. Braun reports personal fees from speaker honoraria from Abbott Vascular, during the conduct of the study. D. Himbert reports personal fees from Edwards Lifesciences and Abbott Vascular. P. Denti reports personal fees from Abbott, and personal fees from Edwards outside the submitted work. R. Estevez-Loureiro reports grants and personal fees from Abbott, and personal fees from Boston Scientific during the conduct of the study. E. Lubos has received lecture fees, grants and travel expenses from Abbott Vascular and Edwards Lifesciences, and honoraria for advisory board activities from New Valve Technology. S. Ludwig reports non-financial support from Edwards Lifesciences outside the submitted work. F. Kreidel received speaker’s honoraria and travel grants from Abbott and Edwards Lifesciences. E. Brochet reports personal fees from Abbott Vascular outside the submitted work. D. Kalbacher reports personal fees and non-financial support from Edwards Lifesciences, and personal fees and non-financial support from Abbott outside the submitted work. K. Connelly reports personal fees from Abbott during the conduct of the study. S. Windecker reports grants from Abbott, Amgen, BMS, Bayer, Boston Scientific, Biotronik, Cardinal Health, CSL Behring, Daiichi Sankyo, Edwards Lifesciences, Johnson&Johnson, Medtronic, Guerbet, Polares, Sanofi, and Terumo, outside the submitted work. S. Windecker serves as an unpaid member of the steering/executive group of trials funded by Abbott, Amgen, BMS, Boston Scientific, Biotronik, Cardiovalve, Edwards Lifesciences, MedAlliance, Medtronic, Polares, Sinomed, V-Wave and Xeltis, but has not received personal payments by any pharmaceutical company or device manufacturer. He is also a member of the steering/executive committee group of several investigator-initiated trials that receive funding by industry without impact on his personal remuneration. H. Sievert reports relationships with industry limited to reimbursement for clinical trials; personal honoraria have not been paid. A. Latib reports consulting for Medtronic, Abbott Vascular, Boston Scientific and Edwards Lifesciences. M. Gavazzoni is speaker, proctor, and preceptor for Abbott Switzerland. R.S. von Bardeleben reports personal fees from Abbott Structural, and personal fees from Edwards Lifesciences outside the submitted work. A. Vahanian reports current consultancy for Cardiovalve and previous consultancy for Abbott Vascular, Edwards Lifesciences and Medtronic. R. Kaple is a speaker for Abbott. T. Nazif reports personal fees and other from Venus Medtech, personal fees from Edwards Lifesciences, Medtronic, and Boston Scientific, outside the submitted work. J. Webb reports consultancy and physician training for Edwards Lifesciences. F. Maisano reports grants and personal fees from Abbott, Medtronic, and Edwards Lifesciences, grants from Biotronik, Boston Scientific, NVT, and Terumo, other from SwissVortex and Perifect, personal fees from Xeltis, other from Transseptal Solutions, personal fees and other from Cardiovalve, personal fees and other from Magenta, other from CardioGard, and other from 4Tech, during the conduct of the study. In addition, F. Maisano has a patent US10058323B2 issued, a patent ITMI20070906A1 issued, a patent US7674286B2 with royalties paid, a patent WO2014170890A1 issued, a patent US8236049B2 issued, a patent US8147542B2 issued, a patent WO2020060587A1 issued, and a patent DTMI20060963A1 issued. J. Hausleiter reports grants and personal fees from Abbott Vascular and Edwards Lifesciences outside the submitted work. R. Hahn reports personal fees from Baylis, other from Boston Scientific, personal fees from Edwards Lifesciences, Medtronic, and Abbott Vascular, other from NaviGate outside the submitted work; she is also Chief Scientific Officer for the Echocardiography Core Laboratory at the Cardiovascular Research Foundation for multiple industry-sponsored trials, for which she receives no direct industry compensation. A. Lauten has a patent with and is a consultant for TricValve licensed to TricValve and is co-founder of devie medical. M. Taramasso reports personal fees from Abbott, Boston Scientific, 4Tech, Edwards Lifesciences, CoreMedic, Mitraltech, and SwissVortex, outside the submitted work. P. Lurz reports grants from Abbott and Edwards Lifesciences, outside the submitted work. M. Zuber is a consultant for Abbott, Edwards Lifesciences, Cormedics, and Cardiovalve and has received speaker honoraria from Pfizer and Canon. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.