Abstract
Aims: The aim of this study was to investigate the procedural feasibility and short-term durability of the transcatheter tricuspid valve edge-to-edge repair technique in highly symptomatic patients with severe tricuspid regurgitation (TR).
Methods and results: Eighteen consecutive patients suffering from severe right-sided heart failure (NYHA Class III-IV), primarily due to moderate to severe tricuspid regurgitation, were included in the study. Applying a modified steering technique for the clip delivery system, six patients were treated for isolated severe TR, while 12 patients were treated for moderate to severe TR and concomitant severe mitral regurgitation. The primary objectives were procedural success, defined as reduction of at least one TR grade, and 30-day echocardiographic and clinical outcomes. A total of 41 clips (2.3±0.7 per patient) were placed into the tricuspid valve of high surgical risk patients (EuroSCORE II: 10±8%). Procedural success was achieved in all patients; no MACCE occurred in hospital. The presence of a TR grade ≥3 was reduced from 94% (17 patients) before the procedure to 33% (six patients) at 30-day follow-up (p<0.001). Sixteen patients (89%) reported an improvement in NYHA functional class at 30 days.
Conclusions: Applying a modified steering technique, the edge-to-edge repair technique can be successfully used for the treatment of TR. At 30-day follow-up, the short-term durability of TR reduction appeared promising and the majority of patients improved clinically. Further studies with larger patient populations and longer follow-up have to define the role of this novel treatment option for patients with right-sided heart failure and severe TR.
Abbreviations
ACE-I: angiotensin-converting enzyme inhibitor
ARB: angiotensin II receptor blocker
ASA: acetylsalicylic acid
CDS: clip delivery system
CRT: cardiac resynchronisation therapy
EROA: effective regurgitant orifice area
ICD: implantable cardioverter defibrillator
ICE: intracardiac echocardiography
LV: left ventricle
MACCE: major adverse cardiac and cerebrovascular events
MLHFQ: Minnesota Living with Heart Failure Questionnaire
MR: mitral regurgitation
NYHA: New York Heart Association
NT-proBNP: N-terminal pro-brain natriuretic peptide
RA: right atrium
RV: right ventricle
STS: Society of Thoracic Surgeons
TAPSE: tricuspid annular plane systolic excursion
TEE: transoesophageal echocardiography
TR: tricuspid regurgitation
TTE: transthoracic echocardiography
Introduction
Severe tricuspid regurgitation (TR) has been shown to be associated with significant morbidity and mortality1,2. Current guidelines recommend surgical tricuspid valve repair in patients with severe symptomatic TR. In addition, tricuspid valve repair should be considered in patients with mild to moderate TR due to annulus dilatation undergoing left-sided valve surgery3,4. However, a large number of patients are ineligible for surgical tricuspid valve repair.
Although several experimental approaches for interventional tricuspid valve repair have been developed, there is no established interventional treatment option for patients with severe symptomatic TR ineligible for cardiac surgery5. In contrast, for patients with severe symptomatic mitral regurgitation (MR) at high risk for cardiac surgery, the MitraClip® system (Abbott Vascular, Santa Clara, CA, USA) has been established as an effective and durable alternative treatment option6-11. Recently, the MitraClip system has also been successfully used for the treatment of severe tricuspid regurgitation in selected cases12,13. However, there are three main reasons which have hindered the broader use of this technique for the treatment of TR so far. 1) The complex and variable anatomy of the tricuspid valve with three leaflets precludes a “double orifice” strategy analogous to percutaneous edge-to-edge repair of the mitral valve. 2) Visualisation of the tricuspid valve leaflets using transoesophageal echocardiography (TEE) is difficult due to poor imaging windows resulting in lower image quality and hence difficulties in the assessment of leaflet insertion using standard views. 3) Steering of the currently available MitraClip system in the right atrium is limited when adhering to standard techniques.
Here, we sought to assess the feasibility, short-term durability and clinical outcome of transcatheter repair of severe tricuspid regurgitation applying a modified steering technique for the MitraClip delivery system.
Methods
STUDY DESIGN
Eighteen consecutive patients who were treated for symptomatic moderate to severe TR using the MitraClip system from March to June 2016 at the University Hospital of the Ludwig-Maximilians-Universität Munich were included in the study. All patients suffered from severe right-sided heart failure (NYHA Class III-IV) despite optimal medical therapy and were deemed inoperable by the Heart Team. Six patients were treated for isolated severe TR, while 12 patients were treated for moderate to severe TR as well as concomitant severe mitral regurgitation. The indication for the combined treatment of the mitral as well as the tricuspid valve was the presence of severe biventricular heart failure attributed to severe regurgitation of these valves. Patients with moderate TR were considered eligible for clip therapy in the presence of a tricuspid annular dilatation of >40 mm. The aetiology of tricuspid regurgitation was primarily functional, secondary to pulmonary hypertension or volume overload (17 out of 18 patients). Severe pulmonary hypertension was not an exclusion criterion for this study. Furthermore, there was no upper limit of malcoaptation and annulus size. Patients with pacemaker leads through the tricuspid valve were considered eligible for interventional treatment if TR was not primarily caused by the lead.
The primary objective of this prospective analysis was to determine the feasibility of the MitraClip procedure at the tricuspid valve. Procedural success was defined as a reduction of at least one TR grade. At 30-day follow-up, transthoracic echocardiographic TR severity grade and NYHA functional class were assessed as major outcome parameters, along with major adverse cardiac and cerebrovascular events (MACCE) during and following the MitraClip procedures. Secondary objectives were the assessment of transthoracic echocardiographic parameters of right ventricular size and function, six-minute walk distance, NT-proBNP as well as quality of life as assessed by the Minnesota Living with Heart Failure Questionnaire (MLHFQ) score at 30-day follow-up. Additional follow-up time points were scheduled at six and 12 months.
PROCEDURAL TECHNIQUE
If present, concomitant severe MR was treated in a first step as described previously6. In order to implant MitraClips successfully between tricuspid leaflets, we developed a modified steering technique for the clip delivery system. The MitraClip system was introduced through the right femoral vein to access the tricuspid valve. However, the standard orientation of the MitraClip delivery system has limited steering options due to the proximity of the inferior vena cava orifice to the atrial septum as well as the short distance of the inferior vena cava orifice to the tricuspid valve coaptation line. Thus, steering of the MitraClip delivery system perpendicular to the tricuspid valve plane is difficult. To overcome these limitations, we inserted the clip delivery system (CDS) 90° counterclockwise into the guide. This allows an outward, clockwise rotation of the guide and enables the “A-knob” to bend the CDS into a direction perpendicular to the tricuspid valve plane.
ECHOCARDIOGRAPHY
The severity of tricuspid regurgitation was graded using transthoracic echocardiography (TTE) according to current guidelines4,14,15 at baseline, before discharge and at 30-day follow-up. Moreover, massive, “torrent” tricuspid regurgitation without significant valve function (vena contracta >1.5 cm, effective loss of tricuspid valve gradient) was assessed as TR grade 4 in order to account for significant TR reduction in terms of regurgitant volume but with residual severe TR post clip implantation. The parameters of right ventricular (RV) size, including tricuspid annulus and RV function, were measured in the apical four-chamber view according to current guidelines16. Clip implantation was guided using a sequential combination of transoesophageal and transgastric multiplane two-dimensional (2D) TEE views as well as multiplane 2D transthoracic views for clip steering and leaflet grasping in the anteroseptal and the posteroseptal tricuspid commissures.
MEDICATION
In patients with oral anticoagulation, the existing medication was continued. In patients without oral anticoagulation, acetylsalicylic acid (ASA) for at least six months and clopidogrel for at least one month was recommended as previously suggested for patients following edge-to-edge repair of the mitral valve6. Postprocedural changes of the concomitant heart failure medication were at the discretion of the primary care physician.
STATISTICAL ANALYSIS
Continuous variables are presented as means±standard deviations. We used Fisher’s exact test to compare categorial variables and the Wilcoxon test for the comparison of continuous variables. A two-tailed p-value <0.05 was regarded as statistically significant.
Results
A total of 18 consecutive patients with a mean age of 78±7 years were considered to be at high surgical risk as expressed by an EuroSCORE II of 10±8% as well as an STS score of 5±3%. All patients suffered from right-sided heart failure due to moderate to high grade tricuspid regurgitation (TR ≥3). The aetiology of tricuspid regurgitation was functional in all but one patient. Consistent with TR aetiology, the majority of patients suffered from pulmonary hypertension as expressed by a right ventricular/right atrial gradient of 37±12 mmHg. Severe pulmonary hypertension (RV/RA >50 mmHg) was present in three patients. Six patients were treated for isolated tricuspid regurgitation, while 12 patients were treated for moderate to severe tricuspid regurgitation as well as concomitant severe mitral regurgitation. Patient characteristics are summarised in Table 1.
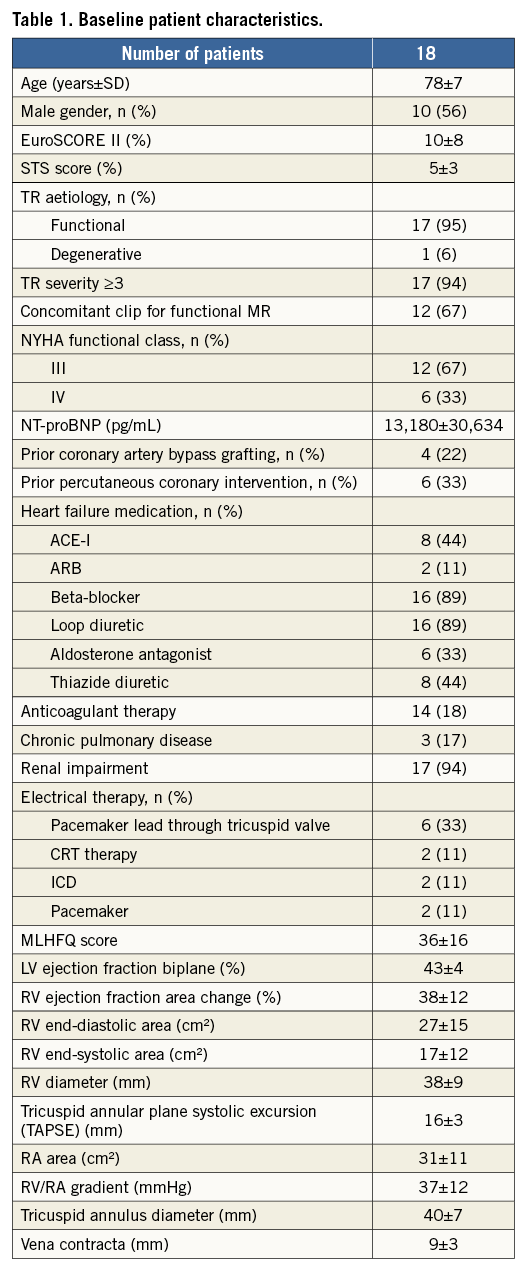
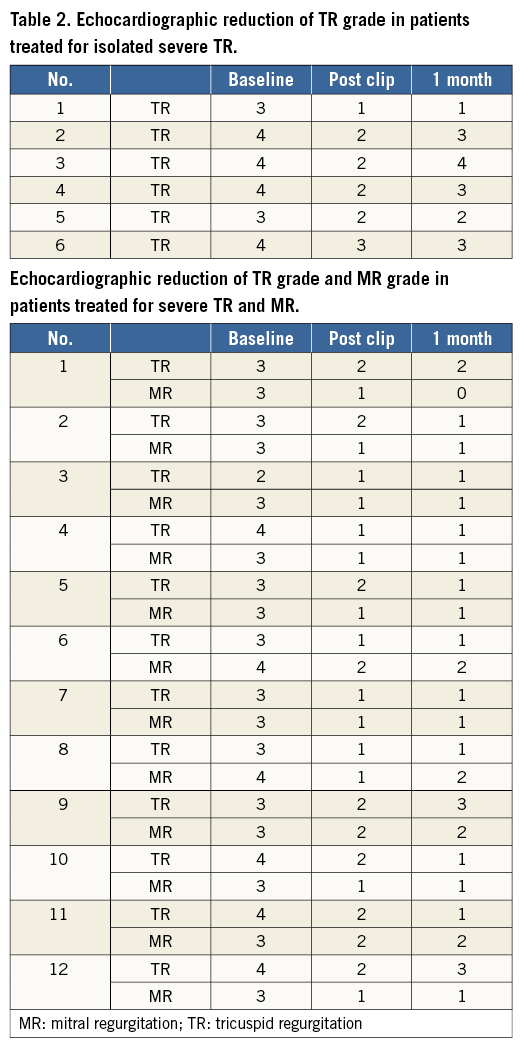
A total of 41 clips (2.3±0.7) were implanted into the tricuspid valve. In all patients we implanted at least one clip between the anterior and septal tricuspid leaflets (total of 30 clips). Eleven additional clips were placed between the posterior and septal tricuspid leaflets. The duration of the tricuspid edge-to-edge procedure was 114±36 minutes. A primarily successful procedure with reduction of tricuspid regurgitation by at least one grade was achieved in all patients. No major adverse cardiac and cerebrovascular events (MACCE) occurred in hospital. In all 12 patients with concomitant MitraClip implantation for severe mitral regurgitation the MR grade could be reduced to MR ≤2. Table 2 depicts the echocardiographic reduction of TR grade and, if applicable, MR grade after the procedures and at one-month follow-up.
30-DAY OUTCOME
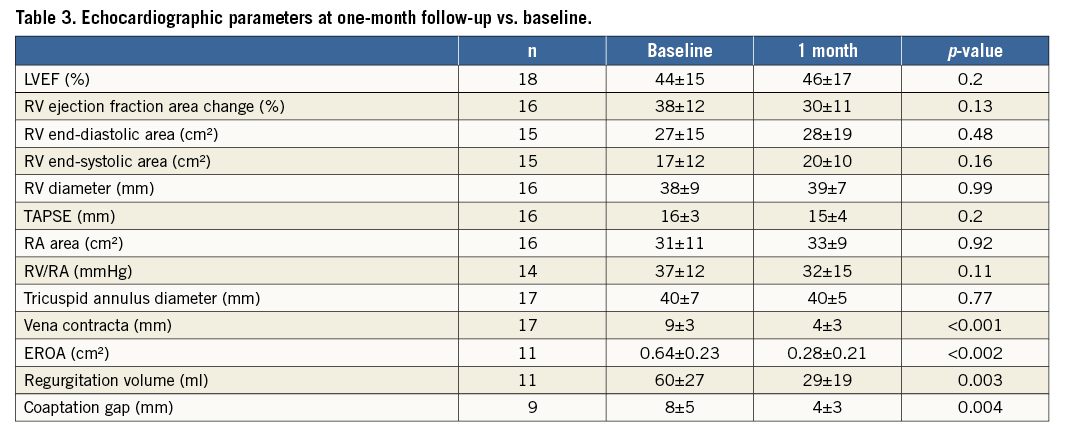
Echocardiography demonstrated a reduction in TR of at least one grade in 16 patients (89%). The presence of a TR grade ≥3 was reduced from 94% (17 patients) before the procedure to 33% (six patients) at 30-day follow-up (p<0.001) (Figure 1). The mean TR grade decreased from 3.4±0.6 at baseline to 1.8±1.0 (p<0.001) at follow-up. Considering quantitative parameters of TR, vena contracta, effective regurgitant orifice area (EROA), regurgitant volume as well as the coaptation gap could be significantly reduced. Table 3 depicts relevant echocardiographic parameters at one-month follow-up vs. baseline.
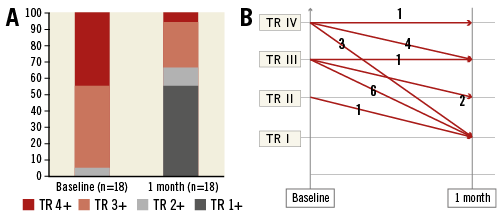
Figure 1. Tricuspid regurgitation grade. A) TR grade at baseline vs. one-month follow-up. B) Procedural change of TR grade for each individual patient. TR: tricuspid regurgitation
Sixteen patients (89%) reported an improvement in NYHA functional class. The incidence of patients with NYHA functional Class ≥III was reduced from 100% (18 patients) to 33% (six patients; p<0.001) (Figure 2). The mean NYHA class decreased from 3.3±0.5 at baseline to 2.3±0.6 at 30-day follow-up (p<0.001).
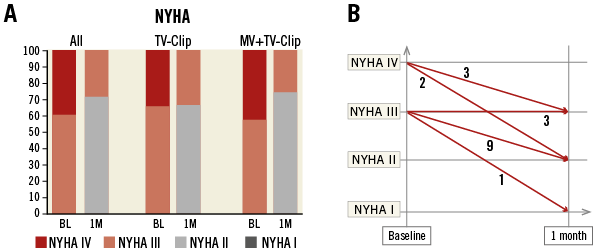
Figure 2. NYHA functional class. A) NYHA status at baseline vs. one-month follow-up for all patients (All), for patients treated for isolated TR (TV-Clip) and for patients treated for severe TR and concomitant severe MR (MV+TV-Clip). B) Procedural change of NYHA status for each individual patient. BL: baseline; 1M: one-month follow-up
In patients treated for isolated tricuspid regurgitation, the NHYA functional class improved by at least one grade in five out of six (83%) patients and the incidence of patients with NYHA Class ≥III was reduced from 100% (six patients) to 33% (two patients) (p=0.06) (Figure 2). In the sixth patient, without improvement of NYHA functional class, we observed single-leaflet clip detachment (one of three clips partially detached) after an initially successful procedure. Due to the recurrent TR, this patient was subsequently treated by placing another MitraClip in the posteroseptal commissure, resulting in an overall TR reduction by one grade.
A patient with severe biventricular heart failure treated for mitral and tricuspid regurgitation developed a cardioembolic stroke approximately two weeks following the procedure while being on adequate anticoagulation for atrial fibrillation.
Considering the secondary trial objectives, we did not observe any worsening of right ventricular function (tricuspid annular plane systolic excursion [TAPSE] at baseline 16.5±3.7 mm vs. 15.5±4.3 mm at 30-day follow-up, p=0.35) despite an effective reduction of tricuspid regurgitation. The six-minute walking distance increased by 25% from 214.7±105.1 m to 267.4±108.4 m (p=0.08). Furthermore, the level of NT-proBNP as a laboratory marker of heart failure decreased from 14,468±33,309 pg/ml to 11,649±24,654 pg/ml (p=0.18). Quality of life, as assessed by the MLHFQ score, improved (37.7±16.4 before the procedure vs. 30.6±19.1 at follow-up, p=0.07). Finally, changes in diuretic dosage at follow-up were determined: diuretic dosages were reduced in nine of 18 patients, while they were maintained unchanged or increased in four and five patients, respectively. The concomitant heart failure medication remained basically unchanged.
Discussion
Severe tricuspid regurgitation has been shown to be associated with significant morbidity and mortality1,2. The gold standard for the treatment of severe TR remains surgical tricuspid valve repair3,4. However, a significant number of patients are deemed inoperable or are at high risk for a surgical approach. To date, there is no established interventional treatment option for these patients. In contrast, percutaneous edge-to-edge repair of the mitral valve has been established for the treatment of severe mitral regurgitation for patients at high risk for cardiac surgery6-8. This interventional approach is based on the surgical Alfieri stitch. The purpose of this prospective study was to evaluate the feasibility and safety of transcatheter repair of the tricuspid valve using the edge-to-edge repair technique in selected patients with right-sided heart failure deemed inoperable by the Heart Team.
A major limitation for interventional tricuspid valve repair is the difficulty of obtaining high-resolution images of the tricuspid valve sufficient for the guidance and steering of interventional procedures. For the treatment of mitral regurgitation using the MitraClip, standard multiplane 2D and three-dimensional (3D) TEE images are usually adequate for clip steering and the visualisation of the leaflet grasping process17. For the treatment of tricuspid regurgitation, we used a sequential combination of transoesophageal (from mid- and end-oesophageal probe positions) and transgastric multiplane 2D TEE views, as well as multiplane 2D transthoracic views (parasternal, apical and subxiphoidal views) for clip steering and leaflet grasping in the anteroseptal and the posteroseptal tricuspid commissures. This combination of echocardiographic techniques appeared to be necessary to address the complex anatomy of the tricuspid valve and to guarantee sufficient leaflet grasping for enduring TR reduction. Intracardiac echocardiography (2D-ICE) was used in some patients in order to improve the procedural guidance. However, we felt that this technique did not help to overcome the limitations of TEE and TTE due to the limited flexibility of the ICE catheter. In this context, the development of 3D-ICE systems might add additional information.
A second major limitation of the MitraClip system for tricuspid valve repair is the difficulty of grasping two tricuspid leaflets simultaneously during clip pullback. This difficulty is based mainly on the close proximity of the guiding catheter with its clip delivery system to the septum in the right atrium, resulting in a non-perpendicular trajectory of the clip system to the tricuspid plane. Furthermore, bending the guiding catheter with the clip delivery system into the right ventricle (using the “+-knob”) will significantly reduce the available length for pulling back the clip in order to capture the leaflets on both arms of the clip. To overcome both limitations, we developed a modified technique for steering the clip delivery system in the tricuspid valve. Instead of the standard orientation, the clip delivery system is inserted into the guiding catheter with a 90° counterclockwise rotation. After straddling the clip delivery system with the guiding catheter, the “A-knob” allows a left rotation of the clip delivery system into the tricuspid valve. This manoeuvre will reduce the proximity to the right atrial septum and will align the clip system with a trajectory perpendicular to the tricuspid plane, which is necessary to load both leaflets simultaneously onto the clip during pullback.
The three leaflets of the tricuspid valve preclude the creation of a double orifice analogous to percutaneous edge-to-edge repair of the mitral valve. However, although tricuspid valve repair using ring annuloplasty is currently the preferred surgical treatment option, bicuspidalisation annuloplasty has been described as an effective alternative surgical treatment option for severe TR (Kay procedure)18-21. In this context, we propose that a similar bicuspidalisation technique of the tricuspid valve using the MitraClip system could be a promising interventional treatment option for patients at high risk for cardiac surgery. Tricuspid bicuspidalisation can be obtained with the clip system by a modified “zipping technique” of the anteroseptal tricuspid commissure22. The first clip is placed into the anteroseptal commissure closest to the tricuspid annulus, while the subsequent clips, usually one or two, are placed inwards in close proximity to the previous clips (Figure 3). This intentionally close positioning of clips results in an approximation of the anterior to the septal leaflet with a fusion and closure of the anteroseptal commissure. The technique may help to overcome the difficulty of treating patients with excessive right ventricular ring dilatations and large central tricuspid coaptation defects.
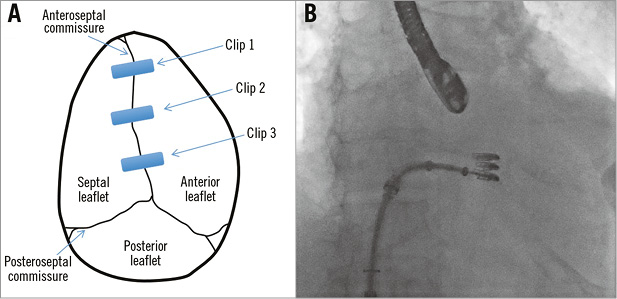
Figure 3. “Zipping technique” to achieve bicuspidalisation of the tricuspid valve. A) Schematic view of the tricuspid valve treated with three MitraClips. B) Corresponding fluoroscopic view following implantation of three MitraClips.
This study, which is the largest consecutive series of patients treated for severe tricuspid regurgitation with the MitraClip system, demonstrates the feasibility, safety and short-term durability of the MitraClip system for transcatheter tricuspid valve repair. The interventional procedures were performed successfully in all 18 patients using the described modified steering approach of the clip system. As expected, NYHA class improved in patients with concomitant treatment for tricuspid and mitral regurgitation at 30-day follow-up, but an improvement was also observed in five out of six patients treated for isolated tricuspid regurgitation. In the sixth patient, NYHA functional class improved until single leaflet clip detachment at the tricuspid valve occurred in the third week after treatment, indicating that the initially achieved reduction of TR was important for the clinical improvement.
The absence of any major adverse cardiac and cerebrovascular events during in-hospital stay demonstrates a comparable safety profile of the tricuspid clip procedure compared to mitral clip procedures. During 30-day follow-up, one cardioembolic stroke occurred in a patient with severe biventricular heart failure treated for severe mitral and tricuspid regurgitation approximately two weeks following the procedure while being on sufficient anticoagulation for atrial fibrillation. Such events have also been reported previously in patients with severely depressed left ventricular function and are possibly explained by thrombus formation due to increased blood stasis23,24. Accordingly, the observed stroke is most probably not related to the described tricuspid but possibly the mitral valve repair.
We observed trends for improvements in six-minute walking distance, NT-proBNP and the MLHFQ score. One reason for the non-significant results could be the relatively low patient number. On the other hand, the process of cardiac recompensation with haemodynamic adjustments and modifications in pharmacologic treatment may take longer than one month in this population of frail and multimorbid patients with severe right-sided heart failure. In this context it will be interesting to evaluate the further clinical outcome beyond one month.
Current knowledge about the use of the edge-to-edge technique for tricuspid repair is based on only a few case reports. In the “largest” series of three consecutive patients, a significant reduction of severe TR was achieved in two of three patients using a transjugular access12.
Limitations
One major limitation of our study is the low patient number. Furthermore, 12 out of 18 patients were treated concomitantly for tricuspid and mitral regurgitation. Hence, clinical improvement could also be due to the reduction in mitral regurgitation in these patients. However, patients treated for isolated tricuspid regurgitation appeared to benefit from the procedure to a similar extent.
Combined percutaneous edge-to-edge repair of the mitral as well as the tricuspid valve was performed in patients with severe left- and right-sided heart failure. The rationale for treating both valves simultaneously in one procedure was the observation that significant TR reduction may persist in a considerable proportion of patients following edge-to-edge repair of the mitral valve25. Furthermore, it has been shown that the presence of moderate-to-severe tricuspid regurgitation independently predicts mortality and re-hospitalisation for heart failure at 12 months after mitral valve edge-to-edge repair26. However, an alternative staged strategy with an initial mitral valve repair followed by a subsequent tricuspid valve repair in patients without TR improvement is possible. In this context, further studies need to define the optimal strategy in this patient subset.
Conclusions
Transcatheter edge-to-edge repair of the tricuspid valve using a modified steering approach is feasible and safe. Furthermore, the successful interventional reduction of TR grade in patients with severe right-sided heart failure appears to be associated with a clinical improvement at 30 days. This improvement was observed in patients treated with isolated interventional tricuspid repair and combined tricuspid and mitral repair. However, further studies with larger patient populations and longer clinical follow-up are necessary to confirm the durability of interventional tricuspid edge-to-edge repair.
| Impact on daily practice Patients with severe tricuspid regurgitation frequently present with severe right-sided heart failure despite optimal medical therapy. However, most patients are not eligible for a surgical approach. Trancatheter repair of severe TR using the edge-to-edge repair technique is feasible and may improve clinical outcome. |
Funding
The current study is an investigator-intiated trial that was conducted without external funding.
Conflict of interest statement
D. Braun has received speaker honoraria from Abbott Vascular. M. Nabauer has received speaker honoraria from Abbott Vascular. M. Orban has received speaker honoraria from Roche and travel grants from Roche and Abbott Vascular. J. Mehilli has received speaker honoraria from Abbott Vascular/Terumo/Lilly/Daiichi Sankyo/BMS/Edwards Lifesciences, as well as institutional research grants from Abbott Vascular and Edwards Lifesciences. J. Hausleiter has received speaker honoraria from Abbott Vascular and Edwards Lifesciences. The other authors have no conflicts of interest to declare.